Most people are aware of the importance of good nutrition these days. Everyone and their grandmother know that when they eat a certain way, they feel better and perform better. However, most people are unaware of just how important nutrition is. Similarly, a lot of people overemphasise the importance of nutrition and incorrectly assume it is more important than it is, compared to something like exercise or sleep (especially in a preventive medicine context).
So, the goal of this article is to detail why nutrition is important, and exactly how important it is.
Before we get stuck in, I would just like to remind you that we offer comprehensive online coaching. So if you need help with your own exercise program or nutrition, don’t hesitate to reach out. If you are a coach (or aspiring coach) and want to learn how to coach nutrition, then consider signing up to our Nutrition Coach Certification course. We do also have an exercise program design course in the works, if you are a coach who wants to learn more about effective program design and how to coach it. We have many other courses available on our education courses home page.
Table of Contents
- 1 Nutrition and Health
- 1.1 Metabolic Health
- 1.2 Obesity and Weight Management
- 1.3 Heart Health
- 1.4 Inflammation
- 1.5 Immune Function
- 1.6 Cancer
- 1.7 Digestive and Gut Health
- 1.8 Allergies and Food Intolerances
- 1.9 Mental and Cognitive Health
- 1.10 Hormonal and Reproductive Health
- 1.11 Hair, Skin and Nail Health
- 1.12 Bone Health
- 1.13 Oral Health
- 1.14 Liver and Kidney Health
- 1.15 Nutrient Related Diseases
- 1.16 Nutrition and Quantity of Life
- 1.17 Nutrition and Quality of Life
- 2 Nutrition and Exercise
- 3 Nutrition and Sleep
- 4 Nutrition and Stress
- 5 Why Is Nutrition Important
- 6 Author
Nutrition and Health
To understand why nutrition is important, we have to start by discussing the role nutrition plays in health. While health can be defined as the absence of disease, we generally don’t think that this fully encompasses what health means. However, it is much easier to detail the role nutrition plays in treating or supporting the recovery from disease than it is to detail the importance of nutrition in preventing disease. It is also difficult to detail all the benefits nutrition has in not just preventing disease, but in facilitating human flourishing. Most people aren’t looking to just survive, they likely want to thrive.
This article certainly won’t be able to capture every aspect of why nutrition is important, but it should hopefully give you the broad brush strokes of why nutrition is important.
The reality is that nutrition does play a role in so many aspects of human health, and you could pretty much summarise this article by saying that “good nutrition is good for all things health”. However, I realise that this isn’t exactly all that enlightening. You want the details, not just the rough outline.
To give you the details, I am going to break this section down into rough body systems or organs. However, I do want to emphasise that these things are all connected and the body doesn’t work in isolated systems. It is easier to discuss things as isolated systems, but this can lead to a situation where you don’t really see the bigger picture and just how connected everything is.
“Good nutrition” also isn’t just a single easily identifiable thing, and different aspects of the diet may be better or worse for different specific issues. Different diet patterns are associated with different health benefits. So, I will be talking in a very general sense when I talk about nutrition being good for specific things. I will of course be detailing what good nutrition looks like in further articles in this series, but for now, I am just going to be discussing good nutrition in a vague sense. Most people are aware of what good nutrition roughly looks like, and what a “balanced diet” is and what “healthy foods” are, so this isn’t a big issue.
However, I am also aware that many of you are reading this series because you want to learn what healthy eating and good nutrition looks like, and as a result, this article may feel like it is skipping ahead with things and assuming everyone already knows many things about nutrition. Unfortunately, there is no real way around this, and you may just need to read through this article with the understanding that you may need to come back to this when you have read the rest of the articles in this series and understand more about what good nutrition looks like.
With that out of the way, we can get stuck into things. To do this, I am just going to go through various systems and specific organs in the body that are impacted by nutrition. But as I said above, this is just for ease of discussion and in reality, everything works in concert together. I am also not ordering these in any meaningful way, so don’t think that this discussion is in some way reflective of the ordering of what systems are more impacted by nutrition.
Metabolic Health
Nutrition plays a key role in overall metabolic health. Metabolism can be broadly thought of as the sum of all the metabolic reactions within the body. These metabolic reactions generally are fuelled by the energy extracted from nutrition, and utilise the fundamental components of nutrition (macronutrients and micronutrients).
When we talk about metabolic health, we are effectively talking about how efficiently the body converts food into energy, how efficiently it transports, uses and/or stores that energy, and how efficiently it uses the various components supplied by the diet.
Good metabolic health generally refers to the optimal functioning of various bodily processes that manage and regulate the body’s energy production, storage, and usage. It means that your body can efficiently convert food into energy, maintain stable blood sugar levels, regulate cholesterol and triglyceride levels, and store and use fat appropriately.
Naturally, the type of diet you eat impacts your metabolic health. If you don’t supply the right kinds of nutrients your body needs to run efficiently (for example, insufficient intake of certain B vitamins can lead to inefficient energy production), or you supply too little or too much of specific nutrients (for example, eating too much refined carbohydrates can lead to poor blood sugar regulation), then this can lead to poor metabolic health. There are other factors beyond nutrition (such as exercise and sleep) that also affect your metabolic health.
As a result, individuals with good metabolic health are less likely to develop conditions like obesity, type 2 diabetes, cardiovascular disease, and metabolic syndrome. Individuals with these conditions who switch to a better diet pattern also tend to manage these conditions and their overall metabolic health much better.
Good metabolic health combined with good dietary practices leads to more optimal energy levels across the day. This leads to fewer energy crashes throughout the day, which tends to lead to more activity and higher energy expenditure across the day (which can lead to better metabolic health). This then becomes a positive feedforward loop where your better metabolic health makes it easier to maintain and even improve your metabolic health.
Obesity and Weight Management
Somewhat related is the fact that nutrition plays a key role in obesity and weight management. A diet that is balanced in nutrients and calorie intake helps maintain a healthy weight, reducing the risk of obesity-related conditions such as type 2 diabetes, heart disease, and certain cancers.
We live in a world of abundance (at least in the developed world), which has led to it being more difficult to maintain a healthy weight. Good nutrition practices play a key role in helping to prevent obesity and excess body fat storage, and the downstream negative health consequences.
Good nutrition practices also play a role in helping individuals improve their health if they are dealing with obesity, and they also play a role in helping individuals dealing with obesity to lose weight. Losing weight is only one aspect of treating obesity though, as the weight loss must be maintained if we are to see the full benefit of the improvements. Good nutrition practices also play a role in long-term weight maintenance, so we have to aim to build a long term sustainable diet rather than a quick fix diet.
Heart Health
Good nutrition plays a key role in heart health. This is probably the area (outside of treating specific nutrient deficiencies or inborn errors of metabolism) where nutrition has an outsized impact on health compared to the other pillars of health (exercise, sleep and stress management).
Good nutrition practices can help regulate bad cholesterol levels (more specifically LDL-C, and even more specifically ApoB), blood pressure, and inflammation, reducing the risk of heart disease and stroke.
Good nutrition practices combined with good exercise practices could probably prevent the vast majority of heart disease. As heart disease is the biggest killer of humans, this is an area where we could see a huge return on investment of effort.
Beyond the role good nutrition plays in preventing heart disease, good nutrition also plays a role in the long term treatment of individuals who have already had a cardiac event.
Inflammation
Good nutrition also plays a role in balancing inflammation in the body. Excess and chronic inflammation is linked to a variety of health conditions, including heart disease, arthritis, and certain cancers. Nutrition can play a role in reducing inflammation.
The overall magnitude of the effect nutrition plays in managing inflammation is debatable, but it does nonetheless play a role. The types and quantities of food you eat can either support lower inflammation, or they can support higher inflammation. As high levels of inflammation aren’t ideal from a health perspective, it makes sense to eat a diet that leads to lower inflammation levels.
Immune Function
A healthy immune system is vital to long term health. A healthy immune system is better able to defend against infection caused by viruses, bacteria and other pathogens. A healthier immune system is also better able to fight off cancer.
Good nutrition practices that supply the body with the right vitamins, minerals and antioxidants can help to support the immune system. This can lead to lower incidences of illness and disease. However, it can also lead to better outcomes for individuals who are already sick or dealing with issues that require a strong immune system.
Nutrition plays a role in both ensuring the immune system is able to fight off illness and in fighting illness when you are ill. As a result, good nutrition practices that improve your immune system generally tend to lead to less illness and a shorter recovery time when you do get sick.
Nutrition also plays a role in autoimmune diseases. Unfortunately, some autoimmune conditions are caused by or exacerbated by certain nutrition practices (for example celiac disease is triggered by gluten). As a result, specific nutrition practices may be needed to help deal with specific autoimmune conditions. Some autoimmune conditions can be pretty significantly improved with specific nutrition practices. With specific nutrition practices, many individuals with autoimmune conditions are able to manage their disease much better and thus lead more normal lives.
Cancer
As nutrition plays a role in the immune system, it naturally plays a role in cancer. Good nutrition is associated with better immune function, and as a result, may contribute to a lower risk of cancer development and progression.
Nutrition also plays a role in individuals who are already diagnosed with cancer. Good nutrition practices can play a vital role in the care and treatment of individuals who have been diagnosed with cancer. While nutrition alone cannot cure cancer, it significantly impacts the overall well-being, quality of life, and outcomes for cancer patients.
A well-nourished body is better able to tolerate and respond to cancer treatments such as chemotherapy, radiation, and surgery. Good nutrition helps maintain strength, immune function, and body weight, all of which are crucial for withstanding the rigours of treatment.
Cancer and its treatments can lead to muscle wasting (cachexia), which significantly weakens the body. Adequate protein intake is essential for maintaining muscle mass, strength, and overall energy levels, allowing patients to stay active and better cope with treatment.
Some studies suggest that good nutritional practices during cancer treatment are associated with better treatment outcomes and potentially improved survival rates. Patients who maintain healthy nutritional practices are more likely to complete their treatment as planned, which is crucial for the effectiveness of cancer therapy.
Good diet practices are also potentially associated with reduced recurrence of cancer. Cancer survivors are often encouraged to adopt eating patterns like the Mediterranean diet, which emphasises plant-based foods, healthy fats, and lean proteins, as this diet is associated with lower rates of cancer recurrence and better overall health.
There are certain diet practices that are associated with an increased/decreased risk of developing certain cancers. Some of these dietary practices are broader in nature (for example, high intakes of fruit and vegetables are associated with a lower incidence of a variety of cancers, especially cancers of the digestive tract), although some of them are more specific (for example, excess sodium intake is associated with increased gastric cancer risk).
Digestive and Gut Health
Rather intuitively, the diet you eat affects your digestive and gut health. Certain diet practices are associated with healthy digestive patterns, regular bowel movements and reduced risk for digestive issues like constipation, diverticulosis and even colorectal cancer.
The gut microbiome is believed to play a role in good health, good digestion, immune function and even mental health. The gut microbiome consists of trillions of bacteria, and these bacteria are fed by your diet. Certain dietary practices, such as high fibre intake along with the consumption of fermented foods, can positively impact your gut microbiome. However, the gut microbiome can also be negatively impacted by poorer dietary choices.
The diet also plays a role in helping to manage many digestive issues, notably irritable bowel syndrome and irritable bowel disease. Both of these can be impacted by dietary choices, and specific dietary patterns are associated with better symptom management for these (and other) conditions.
Most people are also aware that certain foods don’t sit well with their digestive system, or they don’t quite feel their best when they eat a certain way. Optimising the diet for you as an individual can lead to better digestive health overall.
Allergies and Food Intolerances
Related to the last section, tailoring the diet to the individual is even more important for individuals who have specific allergies or food intolerances. These allergies or intolerances can lead to digestive health issues (such as constipation or diarrhoea) or whole-body issues (such as anaphylaxis).
There are too many potential allergies or food intolerances to discuss here, but it is hopefully pretty intuitive to understand that if you have an allergy or intolerance to certain foods, then including them in the diet is unlikely to lead to the best health outcomes. Including these components in the diet may lead to death or it may just lead to a bit of an upset stomach and looser stools. So this really does need to be tailored to the individual’s needs.
Mental and Cognitive Health
Good nutrition positively benefits both mental health and cognitive health and performance. The brain is an organ like every other organ, and as such, requires nutrients and energy to perform effectively. This is especially true of the developing brain. Adequate nutrition during the development of the brain (both in the developing fetus and all the way through to adulthood) is essential to optimal cognitive development.
Good nutrition practices affect cognitive health in a number of ways, from supplying the raw nutrients needed all the way to providing the energy required for cognition. Most people are aware that certain dietary patterns lead to better or worse cognitive performance. This is very obvious in the case of dietary components such as alcohol or caffeine, but it is also the case for calorie and macronutrient intake. Most people just perform better with a more optimal intake of calories and macronutrients.
In an increasingly cognitively demanding working world, good cognitive abilities can result in significant advantages in your earning potential. Even small improvements in cognition can result in more money in your pocket. We know that higher incomes are associated with better health outcomes (to an extent), so the fact that we can improve cognition with good nutrition practices is pretty significant.
Nutrition not only plays a role in improving cognition, but it also plays a role in maintaining good cognition as you age. Good nutrition practices are associated with reduced risk of cognitive decline and diseases like Alzheimer’s and dementia. If you do happen to experience cognitive decline, Alzheimer’s or dementia, then good nutrition practices potentially play a role in reducing further cognitive decline, and supporting overall health while dealing with these issues.
Beyond cognition, nutrition also plays a role in mood. Good nutrition practices are generally associated with reduced risk of mental health disorders such as anxiety and depression. Good nutrition tends to have mood-boosting effects, and generally enhanced happiness. While good nutrition is unlikely to be the cure for mental health issues, it does have the potential to significantly improve these issues in many people.
Beyond just the specific dietary components, food does offer an opportunity for individuals to foster social connections, reduce stress and enhance overall happiness. While the social aspects of eating are generally over-hyped in the context of health and physiology, for improving mood and potentially reducing mental health issues, the hype is real. Most people have felt the benefits of sharing a nice meal with someone else, so I won’t belabour the point.
Hormonal and Reproductive Health
Good nutrition practices are generally associated with a more favourable hormone profile and better reproductive health. In both men and women, good diet practices are associated with better hormonal balance and are associated with reduced risk for hormonal imbalance and hormone-related issues.
Specific nutrition practices can also help support individuals experiencing hormone-related issues. While nutrition alone may not treat or cure these hormone issues, it can play a significant role in improving symptoms, supporting the resolution of the issues and/or improving quality of life while dealing with these issues.
Good nutrition practices also support hormonal health as you age. This is especially important for women going through menopause. Nutrition not only plays a role in supporting healthy hormonal ageing but also in managing and supporting the symptoms and issues that may come along with menopause (e.g. osteoporosis).
Good nutrition practices are also associated with improved fertility in both men and women. This is fairly obvious, as evolution has favoured reducing fertility in times of nutritional hardship (for example, reducing fertility when in a starvation setting). Many people are unaware of how beneficial good nutrition practices are to improving fertility, and in many cases, good nutrition practices can resolve fertility-related issues. Of course, this is not always the case, but it is often surprising how powerful good nutrition can be when it comes to improving fertility.
Not only does good nutrition increase fertility, it is also incredibly important for healthy pregnancies. This is for both the mother and the developing child. Good nutrition supports foetal development, contributes to healthy birth weight, helps prevent birth defects, supports healthy brain development, and reduces the risk of gestational diabetes and preeclampsia. Good nutrition is also important for breastfeeding mothers, as this is a calorie and nutrient-intensive process.
Hair, Skin and Nail Health
Good nutrition practices are also very important for healthy hair, skin and nails. This may seem superficial, and merely an aesthetic concern, but individuals who look in the mirror and see a healthy person looking back at them are more likely to look after themselves. We also live in a society where looks do matter, and thus looking after them is beneficial. Plus, the hair, skin and nails are organs of the body, so why would you not look after organs of the body?
Good diet practices can help to improve the appearance and health of the hair, skin and nails, along with maintaining the health and appearance of them in individuals who already have healthy hair, skin and nails. Good diet practices can also improve the youthfulness of hair, skin and nails, and stave off visual ageing of these organs (especially the skin).
Poor nutrition practices are associated with brittle nails, weak hair and less vital-looking skin. Poor nutrition practices can even lead to hair loss, premature ageing of the skin and premature greying of hair.
Good nutrition practices also play a role in improving acne and reducing the risk of developing acne. Eczema and psoriasis may also be improved or better managed with good nutrition practices.
Bone Health
Most people are aware of the importance of good nutrition to optimal bone health. Good nutrition practices are associated with stronger and healthier bones and teeth. Good nutrition practices also reduce the risk of developing osteoporosis, osteopenia and teeth problems. Good nutrition is also associated with reduced risk of bone fractures and potentially breaks. Good nutrition is also vital in the recovery from fractures and breaks, and in helping individuals to better manage their osteoporosis and osteopenia.
Oral Health
Good nutrition practices are associated with better oral health. Most people are aware that there is a link between the diet and the development of dental cavities. But the link between nutrition and oral health goes deeper than this. Good nutrition practices are a vital part of preventing the development of dental cavities, and gum disease, and are associated with better overall oral health. Optimal management and treatment of these issues also generally require the transition to better nutrition practices.
Liver and Kidney Health
The liver, kidneys, and other organs are responsible for detoxifying the body and are at the “front line” between what you put in your body and how that is then utilised by your body. Good nutrition practices are generally associated with better liver and kidney health. Good nutrition practices are generally associated with better liver and kidney function, and better health overall.
Good nutrition practices are vital in preventing liver and kidney issues. For example, non-alcoholic fatty liver disease risk can be drastically reduced with good nutrition practices. Kidney stone risk is also drastically reduced with good nutrition practices.
Proper long-term management of many liver and kidney diseases and issues also requires a move to good nutrition practices. While the diet alone may not be able to treat many liver and kidney diseases, in almost all cases, these diseases and issues can be improved with better nutrition practices.
Nutrient Related Diseases
Of course, it goes without saying that the many nutrient-related diseases and issues naturally require good nutrition practices to properly treat/manage. It also goes without saying that good nutrition practices are vital in preventing and treating malnutrition.
For example, anaemia is one of the most prevalent nutrient deficiencies worldwide and can be treated with good nutrition practices related to iron intake (although oftentimes, medical intervention may be needed to optimally manage anaemia).
Similarly, diseases like scurvy can be prevented with good nutrition practices. This may seem like it is an issue from a bygone time, but unfortunately, many populations are at risk for vitamin C deficiency (mostly individuals and groups who don’t consume enough fresh fruit and veg, like students, lower-income families and individuals living in areas without regular access to fruit and veg).
Inborn errors of metabolism, like phenylketonuria, can really only effectively be managed with diet. In these conditions, the individuals will need to eat a very specific diet, and avoid certain nutrients.
So, the diet is important for preventing, treating and managing the many nutrient-related diseases.
Nutrition and Quantity of Life
Now, it is all fine and well that good nutrition practices are associated with prevention, better management and sometimes even treatment of specific diseases or issues, but is good nutrition actually associated with improvements in the quantity of life you live? Are you getting more years of life if you follow good nutrition practices?
Well, this is a tricky question to answer. Most studies do agree that following good diet practices could extend life expectancy by several years. Depending on the exact diet principles and the exact population being studied, life expectancy can be increased by 3-10 years, which is pretty significant.
However, it is difficult to truly pinpoint the magnitude of effect, because there are a few issues with the studies looking at this issue.
The first issue is that it depends on what exactly you define as good nutrition practices. There are some commonalities between different healthy diets, but there are also some differences. For example, a primarily plant-based diet and a Mediterranean diet both could be thought of as good diets. However, while they have some similarities, they are also quite different. But both are associated with improvements in life expectancy.
Which brings us to the next issue, what are we comparing the good nutrition practices to? Comparing “good diet” (the diet that follows generally good nutrition practices) to the standard American diet (SAD) is going to result in a huge benefit and improvement in life expectancy. But comparing the “good diet” to the diet of someone who tries to eat healthy when they can but also isn’t following any particular diet, is likely to result in a much lower improvement in life expectancy versus the improvements seen from the SAD comparison. So what we are comparing “good diet” to does impact the magnitude of effect.
The next issue is, who are we talking about? What individual or population are we discussing? If we are looking at a population that is at a high risk for developing heart disease, then “good diet” is likely to significantly boost lifespan. However, if we are talking about a population that already has a relatively long life expectancy, and is generally healthy with low disease risk burden, then we are likely to see a lower lifespan improvement from following “good diet”. This also applies at the individual level (i.e. the magnitude of effect depends on how the individual’s baseline diet compares to “good diet”).
For example, you may be following the general guidelines around saturated fat intake, but you may still have an elevated risk of developing heart disease due to genetically having high levels of lipoprotein(a). This isn’t really modifiable with nutrition and would need pharmacological intervention. So you are unlikely to see a huge increase in life expectancy from good nutrition practices, because they wouldn’t have necessarily decreased your risk of heart disease (although you may still see some increase in life expectancy).
The next issue is that it is hard to detangle the effects of the diet from the rest of the healthy habits someone engages in. Many people who follow good nutrition practices also engage in other healthy habits, such as exercise. This “healthy user bias” makes it difficult to identify the benefits from the diet versus the benefits from the other healthy habits.
Much like with exercise, there are actually different levels of “following good nutrition principles”. For example, we could split the groups into the following:
- Group 1: Someone who follows the standard American diet.
- Group 2: Someone who follows generally good diet principles most of the time, but is a bit looser with the diet every weekend.
- Group 3: Someone who follows good diet principles the vast majority of the time.
- Group 4: Someone who follows good diet principles that are tailored to optimise specific end points such as body composition, blood lipids, HbA1c, etc.
Each of these is going to see a difference in the benefits they get from the diet. You would expect that the more tailored and optimised the diet is to you as an individual and your specific needs, the more benefit you will get.
There are other issues, but you get the idea. It is quite difficult to know the overall increase in lifespan you get from following good nutrition practices. However, it does appear that most people will see an increase in their life expectancy by following good nutrition practices. Ultimately, following good nutrition practices tends to significantly reduce the risk for many chronic diseases, and thus you would expect that to translate into an increase in life expectancy.
I think the best way to illustrate this is to just quickly go through the major diseases that kill humans, and then briefly show whether nutrition plays a role in preventing these diseases and/or supporting health in individuals who already have these diseases.
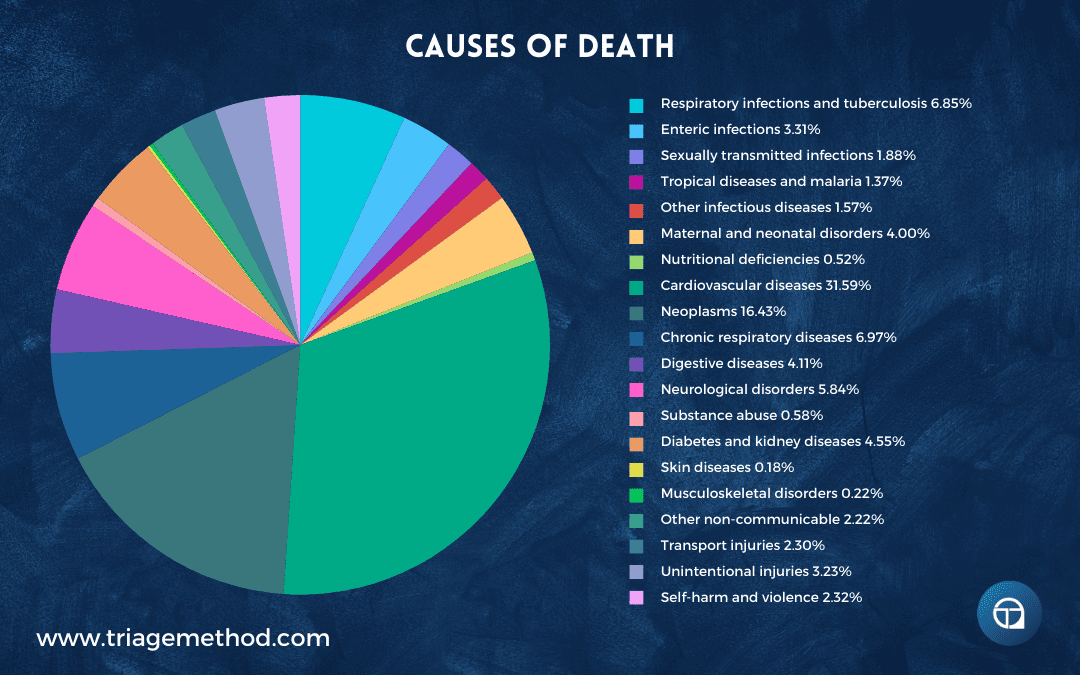
With these major causes of death in mind, we can do a rough assessment of whether or not these issues could be prevented by good nutrition practices (or at least reduce the risk for them) or if good nutrition practices can help lower the burden of these diseases.
| Disease/Disorder Category | Percent | Impact of Nutrition on Disease Burden | Prevention by Nutrition |
| Cardiovascular diseases | 31.59 | Strongly positive (lowers blood pressure, cholesterol, and inflammation) | Strongly yes (significant reduction in risk factors) |
| Neoplasms | 16.43 | Positive (certain diets reduce the risk of some cancers) | Yes (for some types, e.g., colorectal, breast, and stomach cancer) |
| Chronic respiratory diseases | 6.97 | Positive (supports lung health and reduces inflammation) | Yes (especially in managing COPD and asthma with anti-inflammatory diets) |
| Respiratory infections and tuberculosis | 6.85 | Positive (supports immune function) | Potential (stronger immune system may help prevent infections) |
| Neurological disorders | 5.84 | Positive (supports brain health and cognitive function) | Yes (reduces the risk of dementia and supports mental health) |
| Diabetes and kidney diseases | 4.55 | Strongly positive (crucial in blood sugar control and kidney health) | Strongly yes (key in prevention and management) |
| Digestive diseases | 4.11 | Strongly positive (supports digestive health and reduces risk factors) | Yes (prevents digestive issues like IBS and reduces obesity-related risks) |
| Maternal and neonatal disorders | 4.00 | Strongly positive (supports maternal and fetal health) | Yes (reduces the risk of complications like gestational diabetes and preeclampsia) |
| Unintentional injuries | 3.23 | Indirectly (good nutrition supports recovery and overall health) | Indirect (proper nutrition supports overall health and resilience) |
| Enteric infections | 3.31 | Positive (supports immune function and gut health) | Limited (hygiene and safe food handling are crucial) |
| Self-harm and violence | 2.32 | Positive (supports mental health through balanced nutrition) | Indirectly (can reduce risk factors by supporting mental health) |
| Transport injuries | 2.30 | No direct impact | No (nutrition is unrelated) |
| Sexually transmitted infections | 1.88 | Indirect (supports overall immune function) | No (safe practices are key) |
| Other infectious diseases | 1.57 | Positive (supports immune function and recovery) | Potential (proper nutrition can support a stronger immune system) |
| Tropical diseases and malaria | 1.37 | No direct impact | No (prevention through vector control) |
| Musculoskeletal disorders | 0.22 | Strongly positive (supports bone and muscle health through proper nutrition) | Yes (prevents osteoporosis and supports joint health) |
| Other non-communicable | 2.22 | Varies (generally positive depending on the condition) | Varies (depends on the specific condition and nutritional intervention) |
| Substance abuse | 0.58 | Positive (can support recovery through balanced nutrition) | Indirectly (helps with recovery and overall health) |
| Nutritional deficiencies | 0.52 | Strongly positive (directly addresses and prevents deficiencies) | Yes (proper diet prevents nutrient deficiencies) |
| Skin diseases | 0.18 | Positive (certain nutrients improve skin health) | Limited (depends on the type of skin condition) |
So, it should be obvious enough from that table that nutrition plays a role in many of the things that cause humans to die, and as a result, it should not be surprising that good nutrition practices lead to increases in life expectancy. Ultimately, while it is hard to pinpoint the exact quantity of life you could gain from good diet practices, they do seem to result in increases in lifespan.
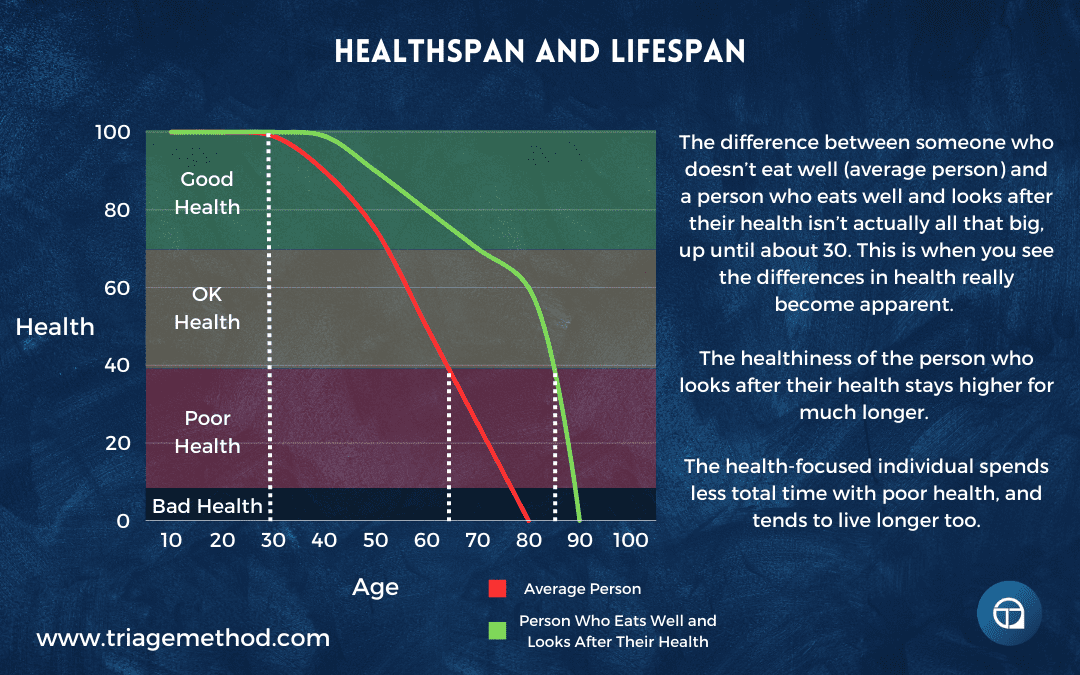
Not only do you get an increase in the quantity of life you get to live, but you also get an increase in the quality of life.
Nutrition and Quality of Life
Most people don’t want to live longer if it means they simply get to live longer with a low quality of life. People want to live for longer while still experiencing good health. Luckily for us, good nutrition practices support this.
Good nutrition practices support a higher quality of life, and most people are aware of this. Even just from a “feeling good” perspective, most people will simply feel much better when eating a healthier diet. General mood is enhanced when following good diet practices, so people tend to just feel better. Combined with the fact that energy levels are better, along with general health being better (thus reduced symptoms interfering with feeling good), most people lead a higher quality of life when following good nutrition practices.
A big win is that cognition and energy levels are improved when following good nutrition practcies. This tends to lead to people getting more done with their days, and feeling like they are living life to the fullest compared to individuals who are eating a poorer diet.
Good nutrition practices also facilitate better weight and body composition management. This is crucial to staving off issues such as metabolic syndrome, but it also generally allows you to maintain better physical functioning throughout your life (especially when combined with exercise). This means you are much better able to engage with life and interact with the world around you more easily.
Related to this is the fact that following good nutrition practices tends to lead to less muscle wasting as you age, thus better functional capacity as you age. As a result, you can do things for much longer into your old age, have a reduced risk for falls (and thus reduced time spent rehabbing injuries) and you can stay more independent as you age. All of which improve your quality of life.
Good nutrition practices also tend to lead to better immune function. This enhanced immune function potentially leads to fewer sick days, and thus fewer days away from enjoying life.
Chronic diseases and their symptoms are generally better managed and potentially alleviated when following good nutrition practices. This is an immeasurable increase in quality of life, as anyone who is dealing with a chronic disease will tell you.
Most people want to stay looking youthful as they age. Good nutrition practices support this goal. Seeing a more youthful-looking person looking back at you in the mirror tends to lead to better care for your health, and thus you tend to see a better lifespan and a higher quality of life.
Overall, good nutrition practices tend to result in an improvement in quality of life. Your healthspan (the years spent with good health) tends to be much higher when following good nutrition practices. So you not only get more years to your life, but those years also tend to be higher quality.
Nutrition and Exercise
Nutrition and exercise are intrinsically linked. Nutrition has a huge effect on exercise, and the vice versa is also true. They are both also foundational health habits, so getting both dialled in can rather dramatically improve your health, body composition and overall life performance. Luckily for us, we also have a huge amount of control over both these areas.
How The Diet Affects Exercise
Most people are aware that what you eat serves as fuel for exercise. So it should be obvious enough that the diet has a large impact on exercise.
You need to actually consume energy to be able to fuel the energy you spend during exercise. Now, you can use stored fat for the fuel (this is why going into a calorie deficit causes fat loss), but this is just food you have previously eaten and stored as energy. You also burn fewer calories from exercise when you are under-fuelled, as you simply don’t have as much energy to perform the exercise effectively.
Which is the next point in how the diet affects exercise, as too little fuel (i.e. low calories) leads to poorer exercise performance. This poorer exercise performance is further compounded by the fact that low energy intake also leads to poorer recovery from exercise and thus you are able to exercise less often.
While not perfectly linear, there’s a strong relationship between calorie intake and exercise performance. Generally, increasing calorie intake improves performance until reaching about 20-30% above maintenance calories, after which further increases provide diminishing returns. Similarly, decreasing calories below maintenance usually reduces performance, but beyond a certain point (roughly 20-30% below maintenance), further cuts may not significantly worsen performance, as it’s already impaired. However, individual responses can vary, and in weight-dependent sports (like running) and weight class sports, this relationship is a bit more complex.
Most people will also be more or less motivated to actually exercise, depending on the quantity of calories they consume regularly. If you are poorly fuelled, you are less likely to be highly motivated to exercise intensely, and conversely, if you are adequately fuelled, you are more likely to actually want to exercise. While physiology is impacted by how well-fuelled you are, so too is psychology.
But the diet is not just energy, and this discussion is not just about calories. The macronutrient composition of the diet also affects exercise. Carbohydrates are the body’s primary source of energy during moderate to high-intensity exercise. Consuming sufficient carbohydrates before exercise ensures adequate glycogen stores in the muscles and liver, and glucose in the blood, which are essential for sustained energy during prolonged or intense workouts. Carbohydrates consumed before exercise can improve endurance, delay fatigue, and enhance performance. You don’t quite get these benefits from consuming fats or protein.
However, protein is essential for muscle repair, growth, and recovery following exercise. Consuming an adequate amount of protein, supports muscle protein synthesis and facilitates muscle repair and adaptation to exercise. With low protein intakes, recovery is impacted and potentially the results you get from exercise are reduced.
Proper hydration is also essential for optimal exercise performance and recovery. Water is involved in numerous physiological processes, including temperature regulation, nutrient transport, and waste removal. Dehydration can reduce exercise performance, increase the risk of heat-related issues, and delay recovery. Electrolytes are also important in the context of proper hydration, as exercising generally leads to sweating which in turn leads to electrolyte loss. Optimal hydration and electrolyte consumption tends to lead to better exercise performance and recovery.
Micronutrient intake is also important for optimal exercise performance, and as such, eating a diet that is low in nutrients is detrimental to performance, especially given the increased micronutrient needs in exercising individuals. This doesn’t mean you need to focus on individual micronutrients, but it does suggest that eating a micronutrient-dense and varied diet would be a good idea.
Nutrient timing can also impact exercise performance and recovery. Consuming carbohydrates and protein before and after exercise can help to optimise glycogen replenishment, muscle repair, and adaptation to exercise. Eating large meals, especially ones that are high in fibre, before exercise can also lead to gastrointestinal discomfort for some people. So meal composition and timing can affect exercise performance.
Ultimately, the diet profoundly influences your ability to exercise to your highest capabilities, recover from that exercise, and adapt and get better from that bout of exercise.
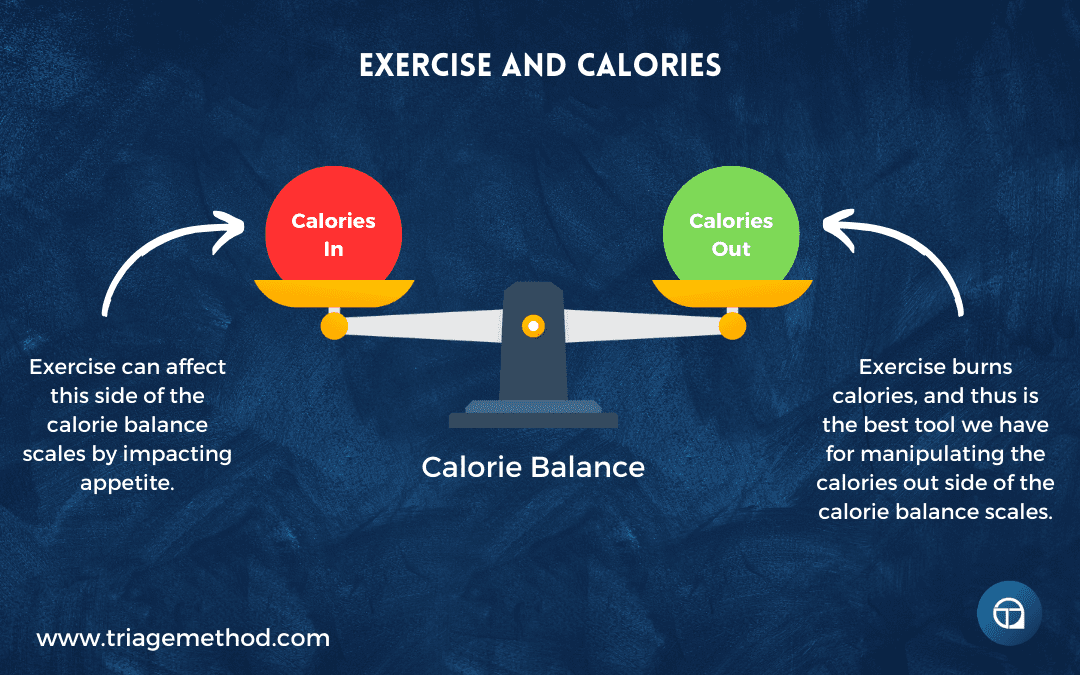
How Exercise Affects The Diet
Exercise affects the diet in a number of ways, and some of these are obvious, while others are less obvious. Understanding how your exercise habits affect your diet is important, and it allows you to further refine your dietary practices and really tailor the diet to your needs.
Exercise increases energy expenditure, meaning your body burns more calories, and as a result, exercise influences the calorie balance equation. With increased energy expenditure, to maintain your weight, you will need to consume more calories. If you instead want to lose weight, you can forgo consuming more calories, and this will tip you into a calorie deficit.
However, the trade off is that you will have less fuel for your workouts (as discussed above). The fact that moving more (exercising) leads to more calories being burned and thus a higher calorie requirement is pretty obvious. However, exercising more potentially also changes how you need to make up those calories (i.e. it influences what you need to eat).
Exercise can influence your macronutrient requirements, with different types and intensities of exercise requiring varying amounts of protein, carbohydrates and fats for optimal performance and recovery. For example, endurance athletes may need higher carbohydrate intake to fuel prolonged exercise sessions, while strength athletes may need higher protein intake to support muscle repair and growth.
Some of this is just a function of increased caloric needs, while some of it is a function of changing physiologic needs (i.e. engaging in glycogen depleting exercise likely means you have an increased need for carbohydrates in the diet if you want to perform optimally, and engaging in exercise, especially resistance training, likely leads to an increased need for protein to fuel muscle building and recovery).
But beyond the macronutrient changes, exercise can increase the body’s demand for certain micronutrients. It is pretty intuitive that if certain micronutrients are needed for certain chemical reactions in the body, increasing the rate of those chemical reactions by exercising likely leads to an increased need for certain micronutrients (both by virtue of the exercise itself requiring more nutrients and the increased calorie intake required to support that energy expenditure also requiring more nutrients to process).
Similarly, exercise increases fluid and electrolyte loss through sweat, leading to increased hydration and electrolyte needs. Staying properly hydrated is essential for optimal health, along with optimal exercise performance and recovery. This increased need for nutrients is often forgotten in discussions of fuelling exercise, and it should be stressed that exercising individuals should prioritise a nutrient-dense diet if optimal performance is the goal (i.e. while some degree of poorer quality food choices can be used to ensure sufficient calorie intake, this has to be balanced by a generally nutrient-dense diet).
Exercise may also have effects on nutrient timing. For example, consuming carbohydrates and protein before and after exercise can really help to optimise energy levels, muscle glycogen stores, and muscle repair and growth. For some people, eating too close to exercise can lead to digestive issues, eating too far away from exercise initiation can lead to lethargy and eating too long after exercise can lead to a feeling of being very depleted. As such, exercise, and the timing of exercise, can affect how the diet needs to be set up and how food needs to be distributed across the day.
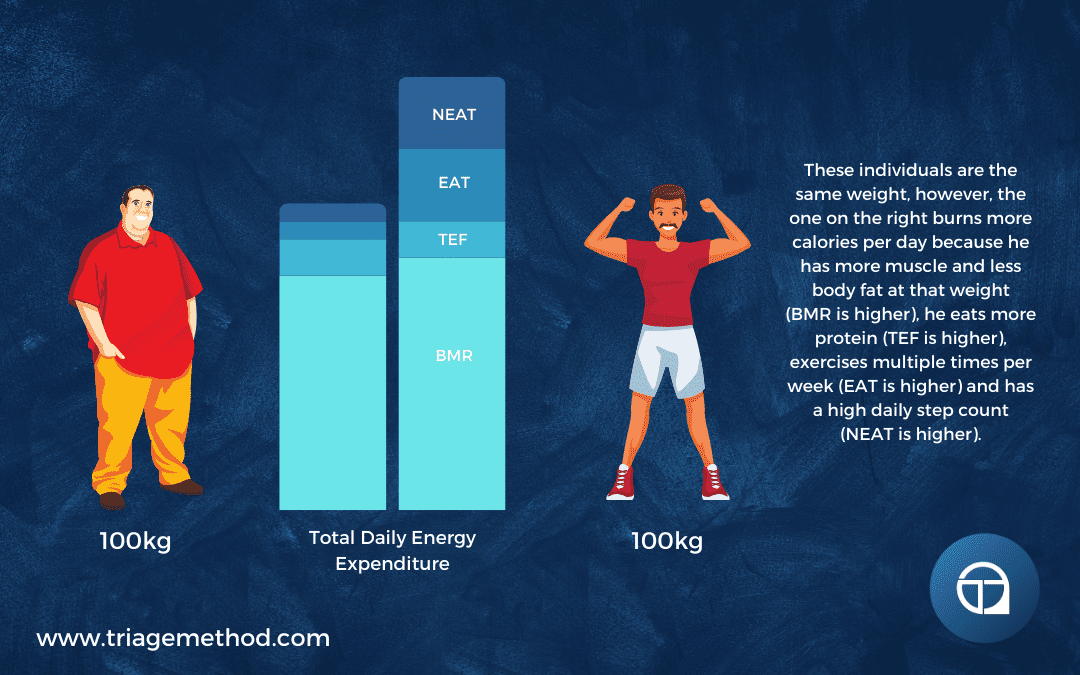
Exercise does have the ability to rather profoundly influence an individual’s metabolism. This is most obvious in its effects on energy expenditure, but it does affect metabolism in a number of other ways. Exercise can lead to muscle building, which in turn increases your basal metabolic rate (BMR), which means your daily calorie intake at baseline is going to be higher. Exercise also tends to improve metabolic flexibility, which is the ability of the body to efficiently switch between different energy substrates (i.e. carbohydrates and fats) based on the metabolic demands being placed on the body, and the availability of the substrates. Exercise also helps increase insulin sensitivity, and the ability to get nutrients into the cells. Exercise also tends to improve mitochondrial number and the efficiency of these mitochondria. As such, exercise rather profoundly improves your metabolism, making it easier to get nutrients into the cell and efficiently convert them into energy.
It can also be helpful to think of exercise as the regulator that dictates how the food you eat is used. While this isn’t a perfect metaphor, it is still important to understand that exercise does play a role in dictating how the food you eat is utilised. This is because exercise can powerfully influence both AMPK and MTOR signalling. AMPK signalling can be thought of as “go time” signalling, as it is responsible for signalling many processes that serve to break down stored nutrients or use nutrients that are circulating in the bloodstream. MTOR signalling can be thought of as “grow time” signalling, as it is responsible for building things in the body (i.e. protein structures like muscle, but also fat stores). While the diet (energy intake, macronutrient intake, and timing) also powerfully influences both AMPK and MTOR, exercise influences them in an arguably more beneficial way (i.e. it tends to lead to the utilisation of fat stores and the building up of muscle).
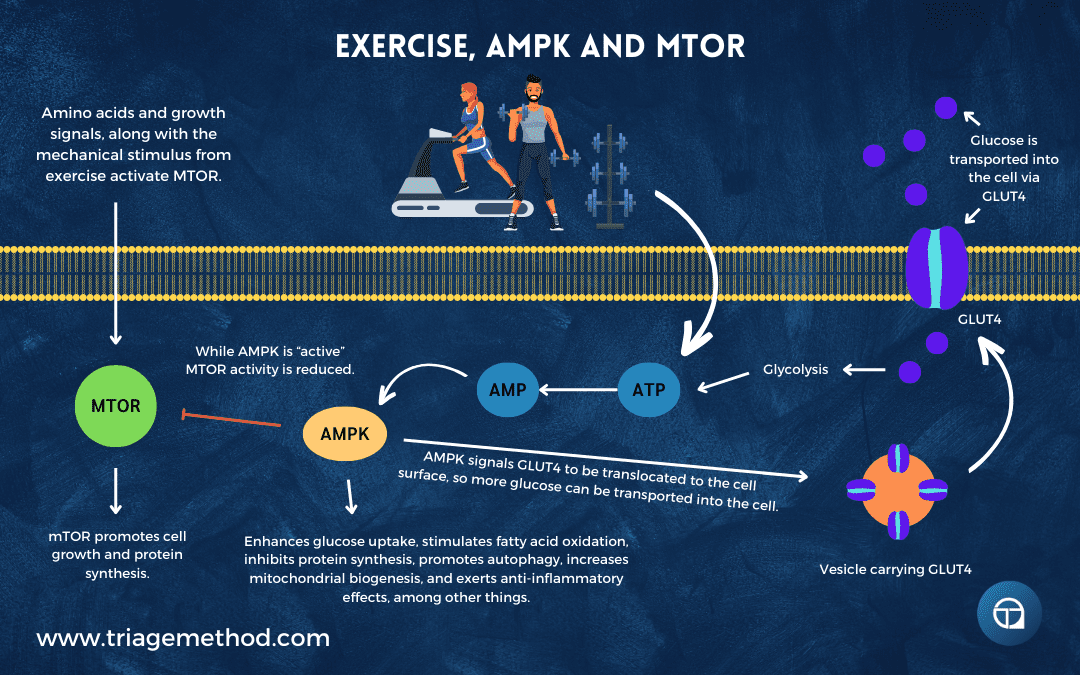
Many people use fasting (i.e. not eating) as a method of activating AMPK pathways, in the belief that this will reduce their risk of disease and potentially also extend their lifespan. However, a much better way to get this AMPK signalling is through exercise, as you also get a host of other positive effects from the exercise, and you don’t get the negative effects of not eating (e.g. reduced metabolism, muscle wasting, hormonal dysregulation etc.).
Exercise also improves appetite regulation, which in turn makes sticking to any diet much easier. Better blood glucose control and metabolic flexibility can lead to better appetite control, and reduced cravings for many individuals. However, this can be quite nuanced and many people experience different appetite and hunger effects from exercise. Unfit people can initially see an increase in appetite when they start exercising, usually due to poorer metabolic flexibility. As they exercise, they deplete the more easily utilised glycogen, and they may find it difficult to as easily utilise stored fat, leading to increased hunger and cravings.
However, generally, as people become fitter and more metabolically flexible, this tends to go away. Although some people will still notice different appetite and hunger effects from exercise, and from my experience coaching people, this can actually be quite wildly divergent. I have had clients who had pretty severe hunger suppression after exercise, which made it quite difficult to consume enough calories to support that level of activity.
Conversely, I have had clients who very acutely see hunger increase directly after exercise. To some degree, this does depend on the type of exercise being done, and the level of intensity it is being performed at, but there isn’t always a consistent logic to it between individuals (i.e. different people’s hunger/appetite react differently to the same exercise), but it is a little bit more consistent for the same individual (i.e. if you get hungry after exercise, it is more likely that this is the pattern that will occur in the future).
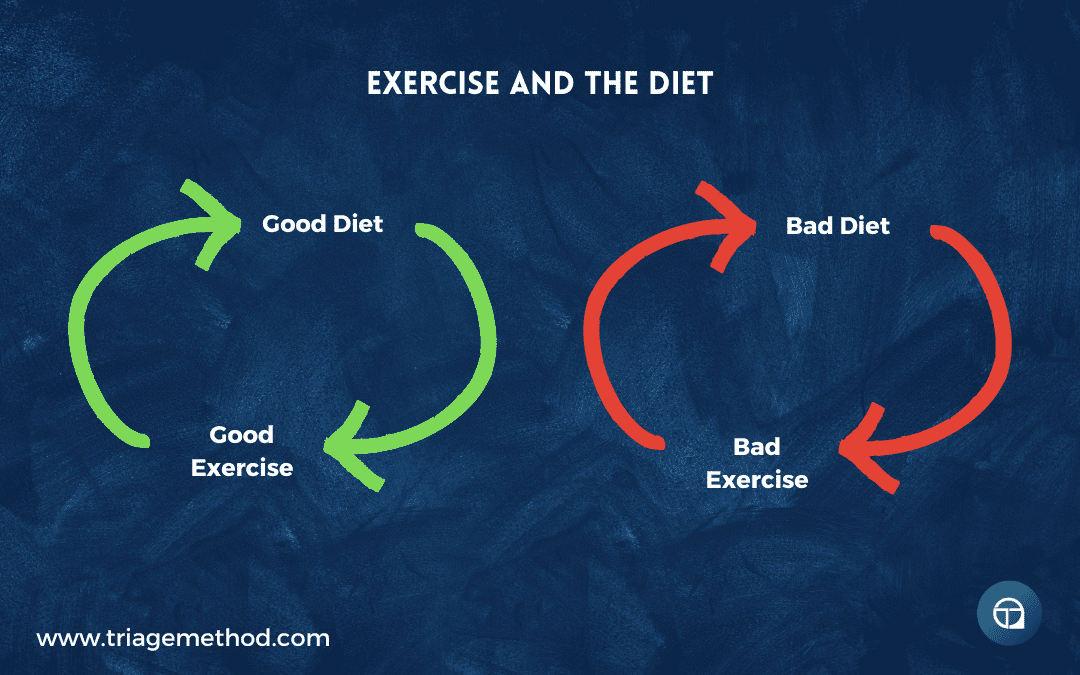
Exercise can also impact individuals’ overall dietary behaviour. Engaging in regular exercise can lead to positive changes in dietary behaviour and food choices. People who exercise regularly generally become more mindful of their dietary habits, eat more nutrient-dense foods and overall, eat in a way that supports their fitness goals and overall health. You have likely experienced this before, where you have trained hard that day, and rather than reaching for the poorer food choices, you choose the healthier option because you want to continue on the positive health streak you have created by exercising.
This is generally positive, but it can be an issue when exercise can’t be performed. In situations like this, poor diet habits can creep in. We see this all the time when we work with athletes who have retired from playing sports. They still have a larger appetite they developed while playing sports, but without the positive influence of exercise, their food selection practices can suffer.
Nutrition and Sleep
While the effects of nutrition on exercise are relatively straightforward and most people are aware of them, most people simply aren’t aware of the effects the diet has on sleep. Most people also aren’t aware of the effects of sleep on the diet. So let’s dig into this!
Diet and Sleep
Your diet and nutrition practices do actually affect your sleep. This isn’t always intuitively obvious to most people, and in our coaching practice, we very often see clients improve their sleep by simply improving their diet. So it is important to know how the diet affects sleep.
While most people think of sleep as a passive process, it does actually require fuel. You get this fuel from your diet. Therefore, it is easy enough to see how what you eat is going to affect your sleep.
The fact that you require energy for sleep is probably most evident in individuals who are eating in a calorie deficit. These individuals, especially if they have been dieting for a longer period of time and/or they are quite lean already, may experience poorer sleep. This is generally due to low blood sugar levels, general hunger being higher, and potentially also higher stress levels (which are serving to mobilise stored fuel (fat)). Obviously, if you have less fat stores and/or you are in a greater deficit, the sleep disturbances may be more pronounced.
Your body doesn’t want to “run out” of fuel while you are sleeping. So it will wake you up, or keep you awake, in an effort to have you spend more time searching for food. So having too few calories in the system will generally lead to poor sleep.
Similarly, some individuals who are more insulin resistant (and thus aren’t getting the glucose into the cells) may find that unless they eat carbs before bed, they will wake up due to dropping blood sugar levels.
This “fear” of running out of energy does have implications for food timing too. Some people say they sleep better when they eat before bed, and this is likely due to either eating too few calories throughout the day (this is a very common issue for people with disordered eating patterns, where they save the majority of their calories for the end of the day) or being somewhat insulin resistant.
However, the research does seem to suggest that eating in the ~2-3 hours before bed isn’t the best practice for improving sleep (or your health). It isn’t a massive issue if you do eat before bed, especially if the vast majority of your lifestyle and sleep practices are dialled in, but it is quite common for sleep quality to be lowered when eating before bed. You may get to sleep more quickly with a belly full of food, but the recovery and repair processes that are supposed to happen when you are asleep can’t occur until the food in your stomach is dealt with. So leaving a bit of a gap between the last meal and sleep makes sense (we generally recommend 2-3 hours between the last bite of food and sleep).
It’s not all just about calories, however. The macronutrient composition of the diet also plays a role too. Protein intake seems to play a role in good quality sleep. Higher protein diets seem to be correlated with improved sleep quality. So it makes sense to ensure that protein intake is sufficient. This generally means eating enough protein throughout the day, rather than trying to hit your protein target right before bed.
Carbohydrates are anecdotally associated with better sleep quality and also with helping people get to sleep faster. There are many potential mechanisms for carbs helping you to fall asleep faster, but it is quite an individualised thing and doesn’t seem to be consistent across people. However, if you notice eating more carbs improves your sleep, then that is obviously a tool in your toolbox to use to improve your sleep.
Some people also find eating some fat, and potentially fibre, before bed does help them to get better sleep. This is likely due to slowing digestion, and causing a much more steady blood glucose level across the night. Having a slow digesting meal is likely the best option for getting a consistently good night’s sleep.
Being poorly hydrated also can lead to poorer sleep, which is a tricky one to deal with, as some people find that drinking water in the lead-up to sleep increases the likelihood of them having to get up to urinate during the night. So you have to ensure hydration is in a good place throughout the day, if you want to ensure hydration is sufficient across the night. This is especially important if you live in a warmer climate (or you create a warmer micro-climate with multiple clothing layers, blankets, heating etc.) and this causes you to sweat through the night. Hydrating through the day and then perhaps tapering off your water intake closer to bed likely leads to improved sleep quality.
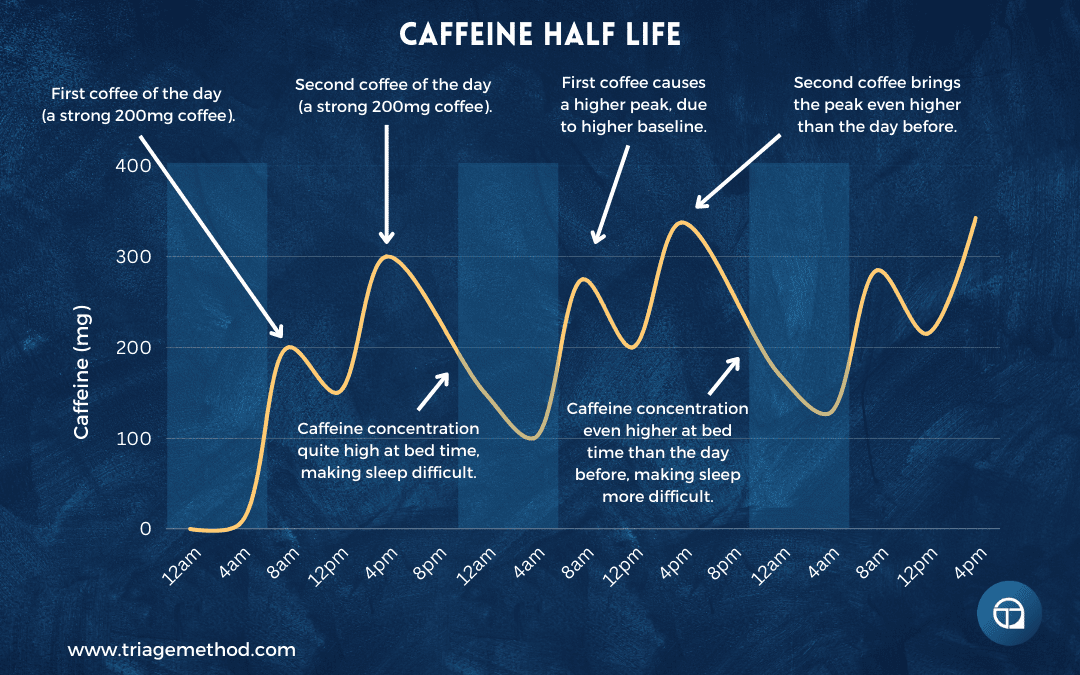
Coffee intake is also associated with poorer sleep, especially if that coffee intake is later in the day. Caffeine is a stimulant, and thus it is not conducive to high-quality sleep or to helping you get to sleep quickly. The unfortunate thing is that caffeine does actually stay in your system for quite a long time, especially if you are a slow caffeine metaboliser. Even if you can get to sleep, if you have an excessive amount of caffeine in your system, sleep quality will likely be reduced. Generally, consuming less than 400mg of caffeine in a day, and having a cut-off for coffee 9-10 hours before bed is best practice, but even this is associated with some reductions in sleep quality.
Alcohol is another drink that negatively affects sleep. Some people will argue that some alcohol is good for sleep as it helps them to get to sleep a bit faster, but even if this were the case, their sleep quality is still reduced. Even with 1 drink, sleep quality is reduced, so it is best to avoid alcohol if you care about your sleep.
Finally, eating foods that just don’t sit well with your digestive system is likely going to negatively impact your sleep. You are unlikely to get high-quality sleep if your stomach is doing somersaults all night. So choosing foods that sit well with your digestion and don’t leave you feeling gassy, bloated, or generally unwell, is probably a good idea.
Sleep and Diet
While the diet impacts sleep, so too does sleep impact the diet. We will be discussing metabolism more in upcoming articles, so I won’t do a deep dive here. However, to make a long story short, sleep does actually influence our metabolism pretty profoundly. It impacts both our calorie expenditure (calories out) and our calorie intake (calories in).
When you sleep less, you end up burning fewer calories during the day at a baseline. Poor sleep results in disturbed hormones, notably thyroid hormones. Lower thyroid output leads to a lower metabolic rate. However, the bigger effect is likely due to the simple fact that being tired likely reduces your energy expenditure by reducing your output during training and your daily life (reduced exercise activity thermogenesis (EAT) and non-exercise activity thermogenesis (NEAT)).
Now, the overall impact may not ultimately add up to much, but it is important to realise that your metabolism and calorie expenditure is likely a little bit lower if you are sleep deprived. The effect could be quite large though, especially if sleep deprivation frequently leads to training being skipped due to tiredness or daily NEAT (as measured by steps for example) being very low.
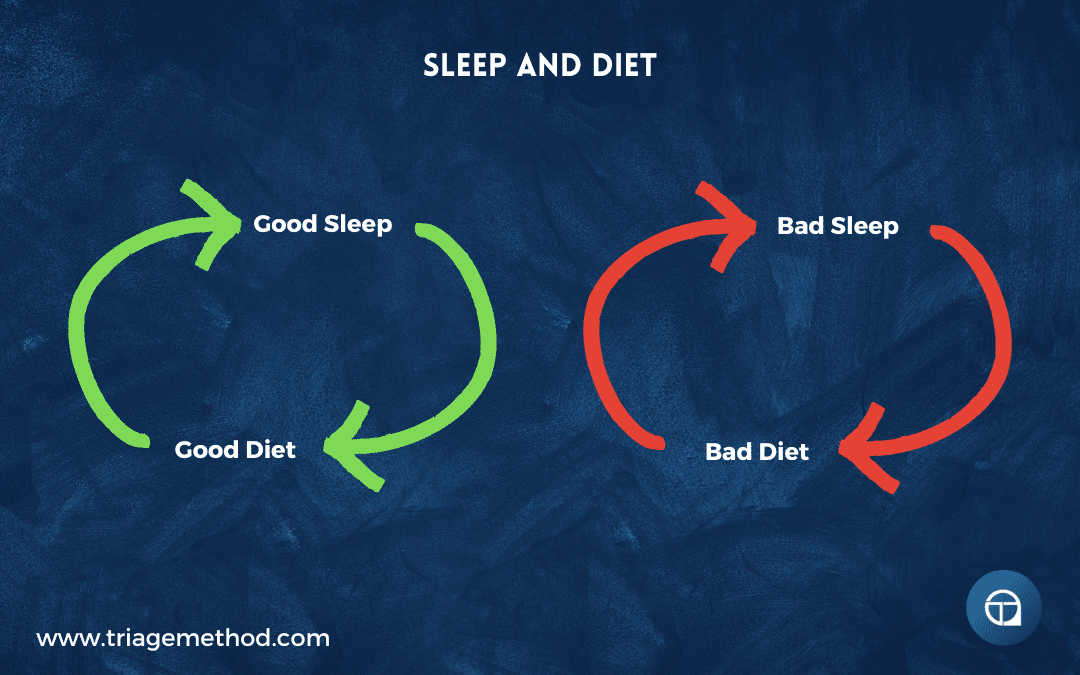
A bigger effect of poor sleep seems to be its effects on influencing your calorie intake. Poor sleep is associated with an increased energy intake (calories in). Most of you have likely experienced this, where you get a poor night of sleep and you just can’t seem to feel full and you are just constantly hungry all day as a result. This is quite common and obviously feeling excessively hungry drastically decreases the likelihood that you will be able to stick to your diet and eat a calorie-appropriate diet long term. Poor sleep is also associated with poorer mood regulation and thus your dietary adherence may also be reduced by virtue of simply feeling worse and turning to food for comfort.
But even if you were able to stick to your calories despite your poor sleep, you will likely be getting less bang for your buck from the diet. You see, a lot of the hormones that are disrupted when sleep is in a bad place, are the hormones that play a role in how the food you eat is used. Carbohydrate metabolism is negatively affected when sleep is bad, pushing you towards a more insulin-resistant state. This isn’t great from a health perspective or a muscle-gain/fat-loss perspective either. Fat metabolism is also disrupted when sleep is poor, which leads to faster storage of fat for later use (a calorie surplus is still required to add to your fat stores over time). But with reduced calorie expenditure and potentially increased food intake due to poor sleep, fat gain is more likely. The fat that is stored in this situation also tends to be visceral fat (the fat stored around your organs), which is the worst type of fat for health. Finally, protein metabolism is also affected by poor sleep. Protein synthesis is reduced (so fewer protein structures (e.g. muscle) are built) and protein degradation is increased (more protein is broken down).
Ultimately, poor sleep leads to reduced muscle anabolism (muscle building), increased fat anabolism (fat storage), increased muscle catabolism (muscle breakdown) and decreased fat catabolism (fat breakdown). While this is a bit of a simplification, and there is obviously a difference between missing an hour of sleep and chronically undersleeping, the general effect is an unfavourable one for those of us who care about our health, performance and body composition.
Getting good quality sleep brings all of these parameters back into a more advantageous position. However, getting more sleep than is needed, (unfortunately) doesn’t confer massive improvements in these various parameters. There is a Goldilocks zone with sleep and getting more sleep than you need isn’t likely to improve your health beyond a certain point, and may just be detrimental to your overall well-being (sleeping for 10+ hours each day does actually eat into your ability to do other things with your life).
Nutrition and Stress
Nutrition is heavily impacted by stress, both in how we interact with the diet on a psychological level, and how our body responds to the food we eat. However, we should also remember that there is a bi-directional pathway here, and nutrition also effects stress and can be a stressor itself.
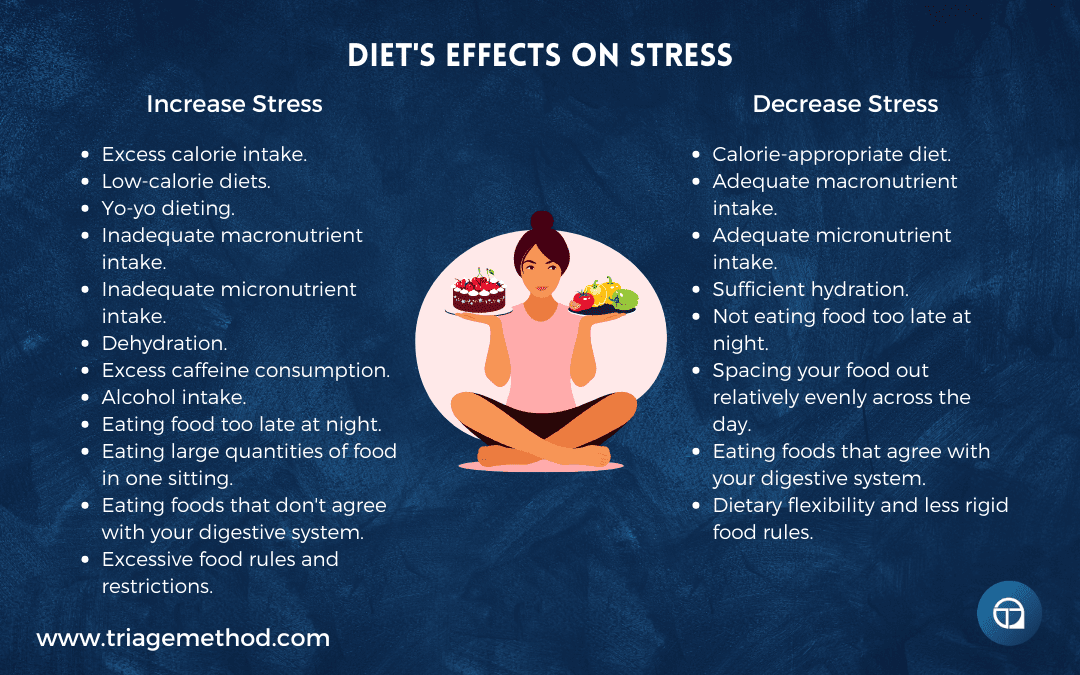
Diet and Stress
The diet can be a stressor, and stress can impact the diet itself, both in terms of quality and quantity. However, it is also important to remember that the nervous system is just responding to the stimuli it is presented with, and perception can alter this. So while I will be speaking in generalities, these should not be taken as a hard and fast rule.
For example, fasting may be a negative stressor (inducing distress) for one individual, but for another who is doing some form of fasting for religious and cultural reasons, may view that as a way to connect with their god and as such, it is a eustress for them. It is also important to remember that there is no “zero exposure” group here, as eating food can be a stressor and eating no food can be a stressor, and we all have some degree of stress impacting on our physiology and our nutrition practices in some form or another. However, despite this, we can still learn quite a lot from this discussion by speaking in generalities here.
Dealing with stress requires resources, and if you aren’t providing them from the diet, you will become less resilient to stress over time, as those resources are depleted. This is both in the form of the energy derived from the diet, the actual macronutrient constituents of the diet, but also the micronutrients obtained from the diet.
When under stress, your body may have higher demands for certain nutrients, potentially above the normally recommended daily allowances. Eating a lower nutrient-density diet can also cause stress to the body, and if this is then combined with an increased requirement for certain nutrients due to an external stressor, then the body’s capacity to deal with stress will be further diminished.
Low nutrient diets can be a cause of stress themselves, but they also lead to reduced resilience to stress from external sources. Eating a high-quality diet is vitally important to actually being able to deal with stress, unfortunately, the general population consumes a low-quality diet, and they are generally under chronic stress. This leads to a vicious cycle of reduced resilience to stress, and a higher likelihood that poorer food choices will be made, exacerbating the issue further.
Low calories diets can be a significant stressor to the body, as the body is forced to mobilise stored energy to make up the deficit of energy. This is what we want to occur when looking for fat loss, however, if the calorie deficit is too severe, goes on excessively long, or is combined with other stressors, the body may not have the capacity to effectively deal with that level of stress. This can also occur in situations where calories are actually at maintenance levels, but a certain macronutrient constituent is low (i.e. low intakes of protein, carbs or fats). While there might technically be enough energy coming in, the body may be being put under stress due to the low availability of a certain macronutrient. This is especially true of low carbohydrate diets, as the low amount of glucose in the blood signals to the body that there is low energy availability, and to not engage in growth and repair.
The psychological stress from dieting must also be factored in, especially if this is in the form of Yo-Yo dieting. The effect of going up and down in weight and calories is probably one of the worst ways you can treat your body with regard to stress and the diet. The rapid swings up and down in weight can cause undue stress on the body, especially if these are rapid and weekly changes in weight.
If you starve yourself Monday to Friday and then binge eat on the weekends, there is enormous stress put on the body from multiple fronts. Binge eating is a stressor, both on the gastrointestinal system (as the foods themselves are usually not the highest quality and you have to deal with the rapid influx of food), and on the cardiovascular system (as it has to deal with rapidly fluctuating water balance in the body).
Then the actual psychological stress that results from feeling like crap after “falling off the diet”, seeing the weight on the scales rocket up, and having to deal with the negative feelings that often occur after binge eating.
Excess nutrients may also be a source of stress on the body, as the body struggles to deal with these nutrients effectively and in a time-efficient manner. These nutrients may then stay in the bloodstream too long, causing damage there. The body will also likely start storing excess nutrients in the form of body fat, when energy is in excess.
Carrying around excess body fat is a stressor in and of itself, both because it means the body has to do more work to carry that weight around, but also because body fat secretes inflammatory signals into the body.
The amount of calories you consume does impact on the hormonal system, notably on the levels of cortisol, thyroid hormones, insulin and testosterone you secrete, and as such, this can profoundly impact your ability to deal with stress. but beyond just the magnitude of calories, the timing of calories can also be a stressor too.
Practices such as intermittent fasting or time-restricted feeding can be a source of stress on the body. Eating food late at night can also be a stressor on the body, especially if it negatively impacts upon sleep.
Higher calories can contribute to gastrointestinal distress, but so too can eating the wrong types of food. Some foods are more inflammatory than others, both on a generalised level and specifically to the individual. The types of food you eat do matter, as some foods can lead to a decline in your ability to handle stress by virtue of triggering low-grade inflammation. This is obvious enough in the case of issues like celiac disease or something like Crohn’s disease, but even in “healthy” individuals, certain foods may be causing some form of inflammation. This is especially the case with low-quality foods, such as refined and processed foods. Focusing on high-quality food selection, and an overall low inflammation style diet generally leads to better stress resilience.
Components of the diet like caffeine, alcohol or various other dietary compounds can increase stress and/or make you less resilient to stress. Caffeine is one that you will have to pay attention to, as it is a stressor in and of itself (that is why it gives you that jolt of energy), and it potentially reduces sleep quality and quantity. However, it is also one of the drugs that people reach for most often when they are stressed. Unfortunately, it is potentially a significant stressor in the diet and it is a crutch that lots of stressed individuals use to deal with their stressful lives.
Alcohol is also one that is used quite frequently as a crutch to deal with stress, with many stressed individuals far exceeding the weekly alcohol targets because they feel they need a glass of wine (or 2 or 3) at night to deal with stress. Unfortunately, alcohol is a stressor itself (it is a toxin the body has to deal with) and that glass of wine each night is likely negatively impacting sleep quality, which makes the individual more stressed and less resilient to stress over time.
Hydration can be a stressor as well, which is often not appreciated. Low hydration levels can induce stress on the body, but so too can excess hydration. While the threshold for excess hydration causing issues is likely higher than would occur in everyday life, it is still apparent in situations like water drinking competitions or sporting events where the individual is sweating a lot. A lot of this has to do with the balance of electrolytes in the body, as drinking excessive amounts of water, without consuming enough electrolytes can cause stress to the body. Similarly, drinking too little water or electrolytes, in general, can cause stress. Anyone who has been dehydrated for any length of time will know just how much overlap there is between feelings of dehydration and stress in general.
However, this relationship between the diet and stress isn’t all negative! You can actually positively influence your stress levels and make yourself more resilient to stress by making good dietary choices. Ensuring that your baseline diet is micronutrient dense, calorie and macronutrient appropriate, and made up of good quality foods that don’t cause you issues, does have a very positive impact on your overall stress levels and your ability to handle stress.
Unfortunately, when people are stressed, they tend to reach for poorer food choices, which generally serves to make things worse physiologically (although psychologically, there can be some positive benefits seen). A lot of people do find themselves caught in this negative loop of reaching for poorer food choices due to stress, thus making their overall stress levels and stress resilience worse. However, the reverse effect is also true, where making good food choices leads to lower stress levels and better stress resilience, which makes it easier to manage stress and thus make better food choices in the future.
Specific dietary intakes and patterns may also interact with stress levels, notably with regard to carbohydrate intake. Insulin is somewhat antagonistic to cortisol, and you may be able to lower cortisol levels by increasing insulin. This is potentially why some people reach for sugary foods when they are stressed, but we can still potentially use this knowledge to modulate our stress levels, without reaching for the sugary foods. In general, ensuring we are eating enough carbohydrates, and spreading this intake throughout the day will help to keep cortisol in a more manageable level.
Stress and Diet
Stress also affects the diet too. When stress is higher (SNS activity), we see an increase in catecholamines and glucocorticoids. This “fight or flight” mode is counterbalanced with the “rest and digest” action of the PSNS. This should give you a clue to the link between nutrition and stress. The high-stress environment is one where the focus is on mobilising energy to deal with the stressor, this inherently means there is a reduced focus on digesting and absorbing nutrients that have just been consumed.
When stress is higher, digestion is worse and the processes of actually utilising that consumed food for anabolic purposes are reduced. Why would you spend energy building new structures or repairing old ones, when you are dealing with a stressor that might end your life? This would be akin to the city being besieged by invaders, and rather than picking up weapons to help defend the city, instead, you go about your same daily tasks as if nothing is going on. The body is a survival machine, and as such, if stress is high, resources are going to preferentially go towards dealing with that stressor. As a result, you get worse “results” (health, performance and body composition) from the diet.
It would make intuitive sense that because higher stress leads to a situation where fuel is being mobilised more readily, surely that would make fat loss easier, right? Well, unfortunately not. For sure, dieting to lose weight is a stressor and we need that mild stress to help with fat loss, but when stress is excessively high (transiently or chronically) there is too much of a catabolic signal and we start to see more muscle loss along with fat loss. In most cases, we are looking to preserve as much muscle mass as possible while dieting, and if stress is high we, unfortunately, see excessive muscle loss.
Further to this, stress leads to a situation where you are less likely to stick to the diet you have set up. This is because those same hormones that are used to mobilise energy, also tend to lead to the body feeling like it needs to replete the energy that has just been mobilised. This is especially true of glucose, as the glucocorticoids that allow you to respond to the stress, also lead to the partial depletion of the glucose in the blood, and this can lead to all that goes along with dips in blood sugar. In general, this leads to increased cravings for high carbohydrate, sugary foods.
Glucose dysregulation is very often seen in high-stress individuals, both as a result of the stress itself (as it mobilises stored glucose) and because of the dietary patterns of high-stress individuals. Those glucocorticoids also interact with mineralocorticoid receptors and as a result, stress can also cause cravings for salty foods. Combined with this, stress can make you hold more water weight. As a result, high-stress individuals trying to diet start potentially seeing more muscle loss, the scales aren’t moving like they expect them to because of the water weight, and they are having stronger and stronger cravings for salty and high-carb foods. This is not a recipe for a successful fat loss phase, and it clearly isn’t health-promoting.
However, it isn’t just fat loss focused dieters that run into issues when stress is high. Even in a gaining phase (surplus calories), stress can cause issues. It should obviously be apparent that having a reduced ability to build muscle is less than ideal when trying to gain muscle, but unfortunately, high stress can make fat gain easier. This is also a particularly harmful type of fat gain, as it is generally in the form of visceral fat, fat stored around the organs. This type of fat leads to multiple negative health outcomes, and it further exacerbates the issues related to having high stress in the first place, as it puts further stress on the body.
High-stress levels can also negatively affect digestion (because you never actually get into that rest and digest state), and as such, this can make getting the food required to effectively gain quality muscle size harder. Hunger can be reduced, and due to stress-causing reduced gastric motility, it can feel like food is just sitting in the digestive tract. Which naturally enough, doesn’t make you feel great, and can lead to reduced adherence and enjoyment of the diet.
Ultimately, stress and the diet are very intertwined. High levels of stress and/or chronically elevated stress can negatively affect the diet, both in terms of how your body reacts to the food you eat and your ability to even stick to the diet in the first place. However, this stuff works both ways, and a poorer diet can negatively impact on your stress levels and your ability to handle stress. So when we discuss stress management, one of the keys is actually just getting really good dietary practices in place. This can be quite difficult when stress is high, but it is a very high-yield stress management practice! Similarly, working on your stress management is also a very high-yield focus when you are trying to get the most from the diet (and when you are trying to actually make it easier to stick to a healthy diet long-term).
Why Is Nutrition Important
Hopefully, you can now see just why nutrition is important. It really is one of the pillars of health. Getting the diet dialled in results in significant improvements in health, body composition and overall performance. So it is a good idea to optimise your diet and tailor it to your needs. You can do this by reaching out to us and getting online coaching, or alternatively, by interacting with our free content.
If you want more free information on nutrition, you can follow us on Instagram, YouTube or listen to the podcast, where we discuss all the little intricacies of exercise. You can always stay up to date with our latest content by subscribing to our newsletter.
Finally, if you want to learn how to coach nutrition, then consider our Nutrition Coach Certification course, and if you want to learn to get better at exercise program design, then consider our course on exercise program design. We do have other courses available too. If you don’t understand something, or you just need clarification, you can always reach out to us on Instagram or via email.
This is the first article in this series, and the next article in this series is The Goals Of Nutrition, if you are interested in continuing to learn about nutrition. You can also go to our nutrition hub to find more nutrition content.
References and Further Reading
Rattan SIS, Kaur G. Nutrition, Food and Diet in Health and Longevity: We Eat What We Are. Nutrients. 2022;14(24):5376. Published 2022 Dec 18. doi:10.3390/nu14245376 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9785741/
Visioli F, Marangoni F, Poli A, Ghiselli A, Martini D. Nutrition and health or nutrients and health?. Int J Food Sci Nutr. 2022;73(2):141-148. doi:10.1080/09637486.2021.1937958 https://pubmed.ncbi.nlm.nih.gov/34148498/
Cena H, Calder PC. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients. 2020;12(2):334. Published 2020 Jan 27. doi:10.3390/nu12020334 https://pubmed.ncbi.nlm.nih.gov/32012681/
Chen Y, Michalak M, Agellon LB. Importance of Nutrients and Nutrient Metabolism on Human Health. Yale J Biol Med. 2018;91(2):95-103. Published 2018 Jun 28. https://pubmed.ncbi.nlm.nih.gov/29955217/
Giacomello E, Toniolo L. Nutrition, Diet and Healthy Aging. Nutrients. 2021;14(1):190. Published 2021 Dec 31. doi:10.3390/nu14010190 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8746852/
Guasch-Ferré M, Willett WC. The Mediterranean diet and health: a comprehensive overview. J Intern Med. 2021;290(3):549-566. doi:10.1111/joim.13333 https://pubmed.ncbi.nlm.nih.gov/34423871/
Locke A, Schneiderhan J, Zick SM. Diets for Health: Goals and Guidelines. Am Fam Physician. 2018;97(11):721-728. https://pubmed.ncbi.nlm.nih.gov/30215930/
Kandel S. An Evidence-based Look at the Effects of Diet on Health. Cureus. 2019;11(5):e4715. Published 2019 May 22. doi:10.7759/cureus.4715 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6650179/
Chen Y, Michalak M, Agellon LB. Importance of Nutrients and Nutrient Metabolism on Human Health. Yale J Biol Med. 2018;91(2):95-103. Published 2018 Jun 28.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6020734/
Kim JY. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J Obes Metab Syndr. 2021;30(1):20-31. doi:10.7570/jomes20065https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8017325/
Thom G, Lean M. Is There an Optimal Diet for Weight Management and Metabolic Health?. Gastroenterology. 2017;152(7):1739-1751. doi:10.1053/j.gastro.2017.01.056 https://pubmed.ncbi.nlm.nih.gov/28214525/
Bennett BJ, Hall KD, Hu FB, McCartney AL, Roberto C. Nutrition and the science of disease prevention: a systems approach to support metabolic health. Ann N Y Acad Sci. 2015;1352:1-12. doi:10.1111/nyas.12945 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5298925/
Macdonald IA, Binia A. Nutrition and the Metabolic Health of Children. Nestle Nutr Inst Workshop Ser. 2023;97:41-50. doi:10.1159/000529004 https://pubmed.ncbi.nlm.nih.gov/37023734/
Wang Y, Chen B, Ma D. The Role of Nutrition and Body Composition on Metabolism. Nutrients. 2024;16(10):1457. Published 2024 May 12. doi:10.3390/nu16101457https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11123915/
Castro-Barquero S, Ruiz-León AM, Sierra-Pérez M, Estruch R, Casas R. Dietary Strategies for Metabolic Syndrome: A Comprehensive Review. Nutrients. 2020;12(10):2983. Published 2020 Sep 29. doi:10.3390/nu12102983 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7600579/
Hoyas I, Leon-Sanz M. Nutritional Challenges in Metabolic Syndrome. J Clin Med. 2019;8(9):1301. Published 2019 Aug 24. doi:10.3390/jcm8091301 https://pubmed.ncbi.nlm.nih.gov/31450565/
García-García FJ, Monistrol-Mula A, Cardellach F, Garrabou G. Nutrition, Bioenergetics, and Metabolic Syndrome. Nutrients. 2020;12(9):2785. Published 2020 Sep 11. doi:10.3390/nu12092785 https://pubmed.ncbi.nlm.nih.gov/32933003/
Kouvari M, D’Cunha NM, Travica N, et al. Metabolic Syndrome, Cognitive Impairment and the Role of Diet: A Narrative Review. Nutrients. 2022;14(2):333. Published 2022 Jan 13. doi:10.3390/nu14020333 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780484/
Keane D, Kelly S, Healy NP, McArdle MA, Holohan K, Roche HM. Diet and metabolic syndrome: an overview. Curr Vasc Pharmacol. 2013;11(6):842-857. doi:10.2174/15701611113116660173 https://pubmed.ncbi.nlm.nih.gov/24168443/
Fahed G, Aoun L, Bou Zerdan M, et al. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int J Mol Sci. 2022;23(2):786. Published 2022 Jan 12. doi:10.3390/ijms23020786 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8775991/
Fabiani R, Naldini G, Chiavarini M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients. 2019;11(9):2056. Published 2019 Sep 2. doi:10.3390/nu11092056 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770202/
Wang W, Liu Y, Li Y, et al. Dietary patterns and cardiometabolic health: Clinical evidence and mechanism. MedComm (2020). 2023;4(1):e212. Published 2023 Feb 5. doi:10.1002/mco2.212https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9899878/
Vincent GE, Jay SM, Sargent C, Vandelanotte C, Ridgers ND, Ferguson SA. Improving Cardiometabolic Health with Diet, Physical Activity, and Breaking Up Sitting: What about Sleep?. Front Physiol. 2017;8:865. Published 2017 Nov 8. doi:10.3389/fphys.2017.00865 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5682337/
Pallazola VA, Davis DM, Whelton SP, et al. A Clinician’s Guide to Healthy Eating for Cardiovascular Disease Prevention. Mayo Clin Proc Innov Qual Outcomes. 2019;3(3):251-267. Published 2019 Aug 1. doi:10.1016/j.mayocpiqo.2019.05.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6713921/
Wu JHY, Micha R, Mozaffarian D. Dietary fats and cardiometabolic disease: mechanisms and effects on risk factors and outcomes. Nat Rev Cardiol. 2019;16(10):581-601. doi:10.1038/s41569-019-0206-1 https://pubmed.ncbi.nlm.nih.gov/31097791/
Han Y, Hu Y, Yu C, et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur Heart J. 2021;42(34):3374-3384. doi:10.1093/eurheartj/ehab413https://pubmed.ncbi.nlm.nih.gov/34333624/
Chareonrungrueangchai K, Wongkawinwoot K, Anothaisintawee T, Reutrakul S. Dietary Factors and Risks of Cardiovascular Diseases: An Umbrella Review. Nutrients. 2020;12(4):1088. Published 2020 Apr 15. doi:10.3390/nu12041088 https://pubmed.ncbi.nlm.nih.gov/32326404/
Badimon L, Chagas P, Chiva-Blanch G. Diet and Cardiovascular Disease: Effects of Foods and Nutrients in Classical and Emerging Cardiovascular Risk Factors. Curr Med Chem. 2019;26(19):3639-3651. doi:10.2174/0929867324666170428103206 https://pubmed.ncbi.nlm.nih.gov/28462707/
Tada H, Takamura M, Kawashiri MA. The Effect of Diet on Cardiovascular Disease, Heart Disease, and Blood Vessels. Nutrients. 2022;14(2):246. Published 2022 Jan 7. doi:10.3390/nu14020246 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780028/
Dinu M, Pagliai G, Sofi F. A Heart-Healthy Diet: Recent Insights and Practical Recommendations. Curr Cardiol Rep. 2017;19(10):95. Published 2017 Aug 24. doi:10.1007/s11886-017-0908-0 https://pubmed.ncbi.nlm.nih.gov/28840462/
Galland L. Diet and inflammation. Nutr Clin Pract. 2010;25(6):634-640. doi:10.1177/0884533610385703 https://pubmed.ncbi.nlm.nih.gov/21139128/
Ricordi C, Garcia-Contreras M, Farnetti S. Diet and Inflammation: Possible Effects on Immunity, Chronic Diseases, and Life Span. J Am Coll Nutr. 2015;34 Suppl 1:10-13. doi:10.1080/07315724.2015.1080101 https://pubmed.ncbi.nlm.nih.gov/26400428/
Wagenaar CA, van de Put M, Bisschops M, et al. The Effect of Dietary Interventions on Chronic Inflammatory Diseases in Relation to the Microbiome: A Systematic Review. Nutrients. 2021;13(9):3208. Published 2021 Sep 15. doi:10.3390/nu13093208 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8464906/
Stromsnes K, Correas AG, Lehmann J, Gambini J, Olaso-Gonzalez G. Anti-Inflammatory Properties of Diet: Role in Healthy Aging. Biomedicines. 2021;9(8):922. Published 2021 Jul 30. doi:10.3390/biomedicines9080922 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8389628/
Minihane AM, Vinoy S, Russell WR, et al. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br J Nutr. 2015;114(7):999-1012. doi:10.1017/S0007114515002093 https://pubmed.ncbi.nlm.nih.gov/26228057/
Scheiber A, Mank V. Anti-Inflammatory Diets. [Updated 2023 Oct 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK597377/
Margină D, Ungurianu A, Purdel C, et al. Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. Int J Environ Res Public Health. 2020;17(11):4135. Published 2020 Jun 10. doi:10.3390/ijerph17114135 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7312944/
Itsiopoulos C, Mayr HL, Thomas CJ. The anti-inflammatory effects of a Mediterranean diet: a review. Curr Opin Clin Nutr Metab Care. 2022;25(6):415-422. doi:10.1097/MCO.0000000000000872 https://pubmed.ncbi.nlm.nih.gov/36039924/
Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006;48(4):677-685. doi:10.1016/j.jacc.2006.03.052https://pubmed.ncbi.nlm.nih.gov/16904534/
Childs CE, Calder PC, Miles EA. Diet and Immune Function. Nutrients. 2019;11(8):1933. Published 2019 Aug 16. doi:10.3390/nu11081933https://pubmed.ncbi.nlm.nih.gov/31426423/
Munteanu C, Schwartz B. The relationship between nutrition and the immune system. Front Nutr. 2022;9:1082500. Published 2022 Dec 8. doi:10.3389/fnut.2022.1082500https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9772031/
Calder PC. Foods to deliver immune-supporting nutrients. Curr Opin Food Sci. 2022;43:136-145. doi:10.1016/j.cofs.2021.12.006 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8702655/
Smith TJ, McClung JP. Nutrition, Immune Function, and Infectious Disease. Med J (Ft Sam Houst Tex). 2021;(PB 8-21-01/02/03):133-136. https://pubmed.ncbi.nlm.nih.gov/33666926/
Christ A, Lauterbach M, Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51(5):794-811. doi:10.1016/j.immuni.2019.09.020https://pubmed.ncbi.nlm.nih.gov/31747581/
Venter C, Eyerich S, Sarin T, Klatt KC. Nutrition and the Immune System: A Complicated Tango. Nutrients. 2020;12(3):818. Published 2020 Mar 19. doi:10.3390/nu12030818https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7146186/
Iddir M, Brito A, Dingeo G, et al. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12(6):1562. Published 2020 May 27. doi:10.3390/nu12061562 https://pubmed.ncbi.nlm.nih.gov/32471251/
Key TJ, Bradbury KE, Perez-Cornago A, Sinha R, Tsilidis KK, Tsugane S. Diet, nutrition, and cancer risk: what do we know and what is the way forward? [published correction appears in BMJ. 2020 Mar 11;368:m996. doi: 10.1136/bmj.m996]. BMJ. 2020;368:m511. Published 2020 Mar 5. doi:10.1136/bmj.m511 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7190379/
Conigliaro T, Boyce LM, Lopez CA, Tonorezos ES. Food Intake During Cancer Therapy: A Systematic Review. Am J Clin Oncol. 2020;43(11):813-819. doi:10.1097/COC.0000000000000749 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7584741/
Ubago-Guisado E, Rodríguez-Barranco M, Ching-López A, et al. Evidence Update on the Relationship between Diet and the Most Common Cancers from the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: A Systematic Review. Nutrients. 2021;13(10):3582. Published 2021 Oct 13. doi:10.3390/nu13103582 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8540388/
Mittelman SD. The Role of Diet in Cancer Prevention and Chemotherapy Efficacy. Annu Rev Nutr. 2020;40:273-297. doi:10.1146/annurev-nutr-013120-041149 https://pubmed.ncbi.nlm.nih.gov/32543948/
Wiseman MJ. Nutrition and cancer: prevention and survival. Br J Nutr. 2019;122(5):481-487. doi:10.1017/S0007114518002222 https://pubmed.ncbi.nlm.nih.gov/30213279/
Ravasco P. Nutrition in Cancer Patients. J Clin Med. 2019;8(8):1211. Published 2019 Aug 14. doi:10.3390/jcm8081211 https://pubmed.ncbi.nlm.nih.gov/31416154/
Gray A, Dang BN, Moore TB, Clemens R, Pressman P. A review of nutrition and dietary interventions in oncology. SAGE Open Med. 2020;8:2050312120926877. Published 2020 Jun 1. doi:10.1177/2050312120926877 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7268120/
Haskins CP, Champ CE, Miller R, Vyfhuis MAL. Nutrition in Cancer: Evidence and Equality. Adv Radiat Oncol. 2020;5(5):817-823. Published 2020 May 24. doi:10.1016/j.adro.2020.05.008https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7557144/
Zitvogel L, Pietrocola F, Kroemer G. Nutrition, inflammation and cancer. Nat Immunol. 2017;18(8):843-850. doi:10.1038/ni.3754 https://pubmed.ncbi.nlm.nih.gov/28722707/
Corsello A, Pugliese D, Gasbarrini A, Armuzzi A. Diet and Nutrients in Gastrointestinal Chronic Diseases. Nutrients. 2020;12(9):2693. Published 2020 Sep 3. doi:10.3390/nu12092693 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7551310/
Livovsky DM, Pribic T, Azpiroz F. Food, Eating, and the Gastrointestinal Tract. Nutrients. 2020;12(4):986. Published 2020 Apr 2. doi:10.3390/nu12040986 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7231022/
Cena H, Calder PC. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients. 2020;12(2):334. Published 2020 Jan 27. doi:10.3390/nu12020334 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7071223/
Hills RD Jr, Pontefract BA, Mishcon HR, Black CA, Sutton SC, Theberge CR. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients. 2019;11(7):1613. Published 2019 Jul 16. doi:10.3390/nu11071613 https://pubmed.ncbi.nlm.nih.gov/31315227/
Puri S, Shaheen M, Grover B. Nutrition and cognitive health: A life course approach. Front Public Health. 2023;11:1023907. Published 2023 Mar 27. doi:10.3389/fpubh.2023.1023907https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10083484/
Klimova B, Dziuba S, Cierniak-Emerych A. The Effect of Healthy Diet on Cognitive Performance Among Healthy Seniors – A Mini Review. Front Hum Neurosci. 2020;14:325. Published 2020 Aug 11. doi:10.3389/fnhum.2020.00325 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7433394/
Hong Y, Clark E, Furbish K, Maggiolo N, West E, Sylvia L. Evidence for Improved Cognitive Health with Diet: A Narrative Review. Altern Ther Health Med. 2023;29(7):12-17. https://pubmed.ncbi.nlm.nih.gov/35180098/
Marchand NE, Jensen MK. The Role of Dietary and Lifestyle Factors in Maintaining Cognitive Health. Am J Lifestyle Med. 2017;12(4):268-285. Published 2017 Apr 11. doi:10.1177/1559827617701066 https://pubmed.ncbi.nlm.nih.gov/32063810/
Fu J, Tan LJ, Lee JE, Shin S. Association between the mediterranean diet and cognitive health among healthy adults: A systematic review and meta-analysis. Front Nutr. 2022;9:946361. Published 2022 Jul 28. doi:10.3389/fnut.2022.946361 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9372716/
Kheirouri S, Alizadeh M. MIND diet and cognitive performance in older adults: a systematic review. Crit Rev Food Sci Nutr. 2022;62(29):8059-8077. doi:10.1080/10408398.2021.1925220 https://pubmed.ncbi.nlm.nih.gov/33989093/
Firth J, Gangwisch JE, Borisini A, Wootton RE, Mayer EA. Food and mood: how do diet and nutrition affect mental wellbeing? [published correction appears in BMJ. 2020 Nov 9;371:m4269. doi: 10.1136/bmj.m4269]. BMJ. 2020;369:m2382. Published 2020 Jun 29. doi:10.1136/bmj.m2382 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7322666/
Feart C, Samieri C, Barberger-Gateau P. Mediterranean diet and cognitive health: an update of available knowledge. Curr Opin Clin Nutr Metab Care. 2015;18(1):51-62. doi:10.1097/MCO.0000000000000131 https://pubmed.ncbi.nlm.nih.gov/25405316/
Lewis JE, Poles J, Shaw DP, et al. The effects of twenty-one nutrients and phytonutrients on cognitive function: A narrative review. J Clin Transl Res. 2021;7(4):575-620. Published 2021 Aug 4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8445631/
Muscaritoli M. The Impact of Nutrients on Mental Health and Well-Being: Insights From the Literature. Front Nutr. 2021;8:656290. Published 2021 Mar 8. doi:10.3389/fnut.2021.656290https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7982519/
Nagao K. Cognition and nutrition: the role of dietary protein and amino acids in cognitive health. Curr Opin Clin Nutr Metab Care. 2024;27(1):40-46. doi:10.1097/MCO.0000000000000987https://pubmed.ncbi.nlm.nih.gov/37874047/
Gómez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008;9(7):568-578. doi:10.1038/nrn2421 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805706/
Owen L, Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc Nutr Soc. 2017;76(4):425-426. doi:10.1017/S0029665117001057 https://pubmed.ncbi.nlm.nih.gov/28707609/
Loughman A, Staudacher HM, Rocks T, et al. Diet and Mental Health. Mod Trends Psychiatry. 2021;32:100-112. doi:10.1159/000510422 https://pubmed.ncbi.nlm.nih.gov/34032648/
Bremner JD, Moazzami K, Wittbrodt MT, et al. Diet, Stress and Mental Health. Nutrients. 2020;12(8):2428. Published 2020 Aug 13. doi:10.3390/nu12082428 https://pubmed.ncbi.nlm.nih.gov/32823562/
Calcaterra V, Verduci E, Stagi S, Zuccotti G. How the intricate relationship between nutrition and hormonal equilibrium significantly influences endocrine and reproductive health in adolescent girls. Front Nutr. 2024;11:1337328. Published 2024 Mar 14. doi:10.3389/fnut.2024.1337328 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10973102/
Kudesia R, Alexander M, Gulati M, Kennard A, Tollefson M. Dietary Approaches to Women’s Sexual and Reproductive Health. Am J Lifestyle Med. 2021;15(4):414-424. Published 2021 May 8. doi:10.1177/15598276211007113 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8299929/
Marks V. How our food affects our hormones. Clin Biochem. 1985;18(3):149-153. doi:10.1016/s0009-9120(85)80099-0 https://pubmed.ncbi.nlm.nih.gov/3888442/
Mazza E, Troiano E, Ferro Y, et al. Obesity, Dietary Patterns, and Hormonal Balance Modulation: Gender-Specific Impacts. Nutrients. 2024;16(11):1629. Published 2024 May 26. doi:10.3390/nu16111629 https://pubmed.ncbi.nlm.nih.gov/38892561/
Mumford SL, Chavarro JE, Zhang C, et al. Dietary fat intake and reproductive hormone concentrations and ovulation in regularly menstruating women. Am J Clin Nutr. 2016;103(3):868-877. doi:10.3945/ajcn.115.119321 https://pubmed.ncbi.nlm.nih.gov/26843151/
Skoracka K, Ratajczak AE, Rychter AM, Dobrowolska A, Krela-Kaźmierczak I. Female Fertility and the Nutritional Approach: The Most Essential Aspects. Adv Nutr. 2021;12(6):2372-2386. doi:10.1093/advances/nmab068 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8634384/
Silvestris E, Lovero D, Palmirotta R. Nutrition and Female Fertility: An Interdependent Correlation. Front Endocrinol (Lausanne). 2019;10:346. Published 2019 Jun 7. doi:10.3389/fendo.2019.00346 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6568019/
Gaskins AJ, Chavarro JE. Diet and fertility: a review. Am J Obstet Gynecol. 2018;218(4):379-389. doi:10.1016/j.ajog.2017.08.010 https://pubmed.ncbi.nlm.nih.gov/28844822/
Vitagliano A, Petre GC, Francini-Pesenti F, et al. Dietary Supplements for Female Infertility: A Critical Review of Their Composition. Nutrients. 2021;13(10):3552. Published 2021 Oct 11. doi:10.3390/nu13103552 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8541636/
Łakoma K, Kukharuk O, Śliż D. The Influence of Metabolic Factors and Diet on Fertility. Nutrients. 2023;15(5):1180. Published 2023 Feb 27. doi:10.3390/nu15051180 https://pubmed.ncbi.nlm.nih.gov/36904180/
Aoun A, Khoury VE, Malakieh R. Can Nutrition Help in the Treatment of Infertility?. Prev Nutr Food Sci. 2021;26(2):109-120. doi:10.3746/pnf.2021.26.2.109 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8276703/
Panth N, Gavarkovs A, Tamez M, Mattei J. The Influence of Diet on Fertility and the Implications for Public Health Nutrition in the United States. Front Public Health. 2018;6:211. Published 2018 Jul 31. doi:10.3389/fpubh.2018.00211 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079277/
Vanderhout SM, Rastegar Panah M, Garcia-Bailo B, et al. Nutrition, genetic variation and male fertility. Transl Androl Urol. 2021;10(3):1410-1431. doi:10.21037/tau-20-592 https://pubmed.ncbi.nlm.nih.gov/33850777/
Ferramosca A, Zara V. Diet and Male Fertility: The Impact of Nutrients and Antioxidants on Sperm Energetic Metabolism. Int J Mol Sci. 2022;23(5):2542. Published 2022 Feb 25. doi:10.3390/ijms23052542 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8910394/
Mate A, Reyes-Goya C, Santana-Garrido Á, Vázquez CM. Lifestyle, Maternal Nutrition and Healthy Pregnancy. Curr Vasc Pharmacol. 2021;19(2):132-140. doi:10.2174/1570161118666200401112955 https://pubmed.ncbi.nlm.nih.gov/32234002/
Grenier LN, Atkinson SA, Mottola MF, et al. Be Healthy in Pregnancy: Exploring factors that impact pregnant women’s nutrition and exercise behaviours. Matern Child Nutr. 2021;17(1):e13068. doi:10.1111/mcn.13068 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7729656/
Chen X, Zhao D, Mao X, Xia Y, Baker PN, Zhang H. Maternal Dietary Patterns and Pregnancy Outcome. Nutrients. 2016;8(6):351. Published 2016 Jun 7. doi:10.3390/nu8060351 https://pubmed.ncbi.nlm.nih.gov/27338455/
Jouanne M, Oddoux S, Noël A, Voisin-Chiret AS. Nutrient Requirements during Pregnancy and Lactation. Nutrients. 2021;13(2):692. Published 2021 Feb 21. doi:10.3390/nu13020692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7926714/
Plećas D, Plesinac S, Kontić Vucinić O. Nutrition in pregnancy: basic principles and recommendations. Srp Arh Celok Lek. 2014;142(1-2):125-130. doi:10.2298/sarh1402125p https://pubmed.ncbi.nlm.nih.gov/24684045/
Apostolopoulou A, Tranidou A, Tsakiridis I, Magriplis E, Dagklis T, Chourdakis M. Effects of Nutrition on Maternal Health, Fetal Development, and Perinatal Outcomes. Nutrients. 2024;16(3):375. Published 2024 Jan 27. doi:10.3390/nu16030375 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10857165/
Weaver CM. Nutrition and bone health. Oral Dis. 2017;23(4):412-415. doi:10.1111/odi.12515 https://pubmed.ncbi.nlm.nih.gov/27250737/
Rizzoli R, Biver E, Brennan-Speranza TC. Nutritional intake and bone health. Lancet Diabetes Endocrinol. 2021;9(9):606-621. doi:10.1016/S2213-8587(21)00119-4 https://pubmed.ncbi.nlm.nih.gov/34242583/
Shams-White MM, Chung M, Du M, et al. Dietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation. Am J Clin Nutr. 2017;105(6):1528-1543. doi:10.3945/ajcn.116.145110 https://pubmed.ncbi.nlm.nih.gov/28404575/
Zhang Q. New Insights into Nutrients for Bone Health and Disease. Nutrients. 2023;15(12):2648. Published 2023 Jun 6. doi:10.3390/nu15122648 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10303436/
Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004. 7, Lifestyle Approaches to Promote Bone Health. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK45523/
Karpouzos A, Diamantis E, Farmaki P, Savvanis S, Troupis T. Nutritional Aspects of Bone Health and Fracture Healing. J Osteoporos. 2017;2017:4218472. doi:10.1155/2017/4218472 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5804294/
O’Connor K, Goldberg LJ. Nutrition and hair. Clin Dermatol. 2021;39(5):809-818. doi:10.1016/j.clindermatol.2021.05.008 https://pubmed.ncbi.nlm.nih.gov/34785008/
Almohanna HM, Ahmed AA, Tsatalis JP, Tosti A. The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatol Ther (Heidelb). 2019;9(1):51-70. doi:10.1007/s13555-018-0278-6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6380979/
Guo EL, Katta R. Diet and hair loss: effects of nutrient deficiency and supplement use. Dermatol Pract Concept. 2017;7(1):1-10. Published 2017 Jan 31. doi:10.5826/dpc.0701a01 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5315033/
Rajput RJ. Influence of Nutrition, Food Supplements and Lifestyle in Hair Disorders. Indian Dermatol Online J. 2022;13(6):721-724. Published 2022 Oct 21. doi:10.4103/idoj.idoj_175_22 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9650738/
Pappas A, Liakou A, Zouboulis CC. Nutrition and skin. Rev Endocr Metab Disord. 2016;17(3):443-448. doi:10.1007/s11154-016-9374-z https://pubmed.ncbi.nlm.nih.gov/27401878/
Park K. Role of micronutrients in skin health and function. Biomol Ther (Seoul). 2015;23(3):207-217. doi:10.4062/biomolther.2015.003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428712/
Solway J, McBride M, Haq F, Abdul W, Miller R. Diet and Dermatology: The Role of a Whole-food, Plant-based Diet in Preventing and Reversing Skin Aging-A Review. J Clin Aesthet Dermatol. 2020;13(5):38-43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7380694/
Michalak M, Pierzak M, Kręcisz B, Suliga E. Bioactive Compounds for Skin Health: A Review. Nutrients. 2021;13(1):203. Published 2021 Jan 12. doi:10.3390/nu13010203 https://pubmed.ncbi.nlm.nih.gov/33445474/
Cao C, Xiao Z, Wu Y, Ge C. Diet and Skin Aging-From the Perspective of Food Nutrition. Nutrients. 2020;12(3):870. Published 2020 Mar 24. doi:10.3390/nu12030870 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7146365/
Piccardi N, Manissier P. Nutrition and nutritional supplementation: Impact on skin health and beauty. Dermatoendocrinol. 2009;1(5):271-274. doi:10.4161/derm.1.5.9706 https://pubmed.ncbi.nlm.nih.gov/20808515/
Gondivkar SM, Gadbail AR, Gondivkar RS, et al. Nutrition and oral health. Dis Mon. 2019;65(6):147-154. doi:10.1016/j.disamonth.2018.09.009 https://pubmed.ncbi.nlm.nih.gov/30293649/
Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004;7(1A):201-226. doi:10.1079/phn2003589 https://pubmed.ncbi.nlm.nih.gov/14972061/
Tungare S, Paranjpe AG. Diet and Nutrition to Prevent Dental Problems. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534248/
Shodhan Shetty A, Shenoy R, Dasson Bajaj P, et al. Role of nutritional supplements on oral health in adults – A systematic review. F1000Res. 2023;12:492. Published 2023 May 15. doi:10.12688/f1000research.134299.1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10285321/
König KG. Diet and oral health. Int Dent J. 2000;50(3):162-174. doi:10.1111/j.1875-595x.2000.tb00555.x https://pubmed.ncbi.nlm.nih.gov/10967767/
Tenelanda-López D, Valdivia-Moral P, Castro-Sánchez M. Eating Habits and Their Relationship to Oral Health. Nutrients. 2020;12(9):2619. Published 2020 Aug 27. doi:10.3390/nu12092619 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7551577/
Scardina GA, Messina P. Good oral health and diet. J Biomed Biotechnol. 2012;2012:720692. doi:10.1155/2012/720692 https://pubmed.ncbi.nlm.nih.gov/22363174/
Jackson AA. Nutrition and Liver Health. Dig Dis. 2017;35(4):411-417. doi:10.1159/000456596 https://pubmed.ncbi.nlm.nih.gov/28468010/
Jamioł-Milc D, Gudan A, Kaźmierczak-Siedlecka K, et al. Nutritional Support for Liver Diseases. Nutrients. 2023;15(16):3640. Published 2023 Aug 19. doi:10.3390/nu15163640 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10459677/
Mega A, Marzi L, Kob M, Piccin A, Floreani A. Food and Nutrition in the Pathogenesis of Liver Damage. Nutrients. 2021;13(4):1326. Published 2021 Apr 16. doi:10.3390/nu13041326https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8073814/
Parra-Vargas M, Rodriguez-Echevarria R, Jimenez-Chillaron JC. Nutritional Approaches for the Management of Nonalcoholic Fatty Liver Disease: An Evidence-Based Review. Nutrients. 2020;12(12):3860. Published 2020 Dec 17. doi:10.3390/nu12123860 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766941/
George ES, Forsyth A, Itsiopoulos C, et al. Practical Dietary Recommendations for the Prevention and Management of Nonalcoholic Fatty Liver Disease in Adults. Adv Nutr. 2018;9(1):30-40. doi:10.1093/advances/nmx007 https://pubmed.ncbi.nlm.nih.gov/29438460/
Marchesini G, Petta S, Dalle Grave R. Diet, weight loss, and liver health in nonalcoholic fatty liver disease: Pathophysiology, evidence, and practice. Hepatology. 2016;63(6):2032-2043. doi:10.1002/hep.28392 https://pubmed.ncbi.nlm.nih.gov/26663351/
Morisco F, Vitaglione P, Amoruso D, Russo B, Fogliano V, Caporaso N. Foods and liver health. Mol Aspects Med. 2008;29(1-2):144-150. doi:10.1016/j.mam.2007.09.003 https://pubmed.ncbi.nlm.nih.gov/18061253/
van Westing AC, Küpers LK, Geleijnse JM. Diet and Kidney Function: a Literature Review. Curr Hypertens Rep. 2020;22(2):14. Published 2020 Feb 3. doi:10.1007/s11906-020-1020-1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6997266/
Ko GJ, Rhee CM, Kalantar-Zadeh K, Joshi S. The Effects of High-Protein Diets on Kidney Health and Longevity. J Am Soc Nephrol. 2020;31(8):1667-1679. doi:10.1681/ASN.2020010028https://pubmed.ncbi.nlm.nih.gov/32669325/
Naber T, Purohit S. Chronic Kidney Disease: Role of Diet for a Reduction in the Severity of the Disease. Nutrients. 2021;13(9):3277. Published 2021 Sep 19. doi:10.3390/nu13093277https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8467342/
Kramer H. Diet and Chronic Kidney Disease. Adv Nutr. 2019;10(Suppl_4):S367-S379. doi:10.1093/advances/nmz011 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6855949/
Fadnes LT, Økland JM, Haaland ØA, Johansson KA. Estimating impact of food choices on life expectancy: A modeling study [published correction appears in PLoS Med. 2022 Mar 25;19(3):e1003962. doi: 10.1371/journal.pmed.1003962]. PLoS Med. 2022;19(2):e1003889. Published 2022 Feb 8. doi:10.1371/journal.pmed.1003889 https://pubmed.ncbi.nlm.nih.gov/35134067/
Fadnes LT, Økland JM, Haaland ØA, Johansson KA. Correction: Estimating impact of food choices on life expectancy: A modeling study. PLoS Med. 2022;19(3):e1003962. Published 2022 Mar 25. doi:10.1371/journal.pmed.1003962 https://pubmed.ncbi.nlm.nih.gov/35333861/
Chudasama YV, Khunti K, Gillies CL, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: A longitudinal cohort study. PLoS Med. 2020;17(9):e1003332. Published 2020 Sep 22. doi:10.1371/journal.pmed.1003332 https://pubmed.ncbi.nlm.nih.gov/32960883/
You W, Henneberg R, Saniotis A, Ge Y, Henneberg M. Total Meat Intake is Associated with Life Expectancy: A Cross-Sectional Data Analysis of 175 Contemporary Populations. Int J Gen Med. 2022;15:1833-1851. Published 2022 Feb 22. doi:10.2147/IJGM.S333004 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8881926/
Wickramasinghe K, Mathers JC, Wopereis S, Marsman DS, Griffiths JC. From lifespan to healthspan: the role of nutrition in healthy ageing. J Nutr Sci. 2020;9:e33. Published 2020 Aug 24. doi:10.1017/jns.2020.26 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7550962/
Fadnes LT, Celis-Morales C, Økland JM, et al. Life expectancy can increase by up to 10 years following sustained shifts towards healthier diets in the United Kingdom. Nat Food. 2023;4(11):961-965. doi:10.1038/s43016-023-00868-w https://pubmed.ncbi.nlm.nih.gov/37985698/
Li Y, Pan A, Wang DD, et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population [published correction appears in Circulation. 2018 Jul 24;138(4):e75. doi: 10.1161/CIR.0000000000000587]. Circulation. 2018;138(4):345-355. doi:10.1161/CIRCULATIONAHA.117.032047 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207481/
Martinez-Gonzalez MA, Martin-Calvo N. Mediterranean diet and life expectancy; beyond olive oil, fruits, and vegetables. Curr Opin Clin Nutr Metab Care. 2016;19(6):401-407. doi:10.1097/MCO.0000000000000316 https://pubmed.ncbi.nlm.nih.gov/27552476/
Longo VD, Di Tano M, Mattson MP, Guidi N. Intermittent and periodic fasting, longevity and disease. Nat Aging. 2021;1(1):47-59. doi:10.1038/s43587-020-00013-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8932957/
Govindaraju T, Sahle BW, McCaffrey TA, McNeil JJ, Owen AJ. Dietary Patterns and Quality of Life in Older Adults: A Systematic Review. Nutrients. 2018;10(8):971. Published 2018 Jul 26. doi:10.3390/nu10080971 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6115962/
Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of Diet on Fatigue and Quality of Life in Multiple Sclerosis: A Systematic Review and Network Meta-analysis of Randomized Trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371 https://pubmed.ncbi.nlm.nih.gov/36257717/
Burd NA, Tang JE, Moore DR, Phillips SM. Exercise training and protein metabolism: influences of contraction, protein intake, and sex-based differences. J Appl Physiol (1985). 2009;106(5):1692-1701. doi:10.1152/japplphysiol.91351.2008 https://pubmed.ncbi.nlm.nih.gov/19036897/
Ogasawara R, Sato K, Matsutani K, Nakazato K, Fujita S. The order of concurrent endurance and resistance exercise modifies mTOR signaling and protein synthesis in rat skeletal muscle. Am J Physiol Endocrinol Metab. 2014;306(10):E1155-E1162. doi:10.1152/ajpendo.00647.2013 https://pubmed.ncbi.nlm.nih.gov/24691029/
Thackray AE, Stensel DJ. The impact of acute exercise on appetite control: Current insights and future perspectives. Appetite. 2023;186:106557. doi:10.1016/j.appet.2023.106557 https://pubmed.ncbi.nlm.nih.gov/37044176/
Panissa VLG, Cardoso LK, Rossi PAQ, Fukuda DH, Rossi FE. The impact of acute and chronic resistance training on appetite and energy intake: A scoping review examining resistance exercise and comparisons with other exercise modalities. Appetite. 2024;193:107155. doi:10.1016/j.appet.2023.107155 https://pubmed.ncbi.nlm.nih.gov/38081545/
Hubner S, Boron JB, Koehler K. The Effects of Exercise on Appetite in Older Adults: A Systematic Review and Meta-Analysis. Front Nutr. 2021;8:734267. Published 2021 Nov 18. doi:10.3389/fnut.2021.734267 https://pubmed.ncbi.nlm.nih.gov/34869516/
Dorling J, Broom DR, Burns SF, et al. Acute and Chronic Effects of Exercise on Appetite, Energy Intake, and Appetite-Related Hormones: The Modulating Effect of Adiposity, Sex, and Habitual Physical Activity. Nutrients. 2018;10(9):1140. Published 2018 Aug 22. doi:10.3390/nu10091140 https://pubmed.ncbi.nlm.nih.gov/30131457/
Douglas JA, King JA, Clayton DJ, et al. Acute effects of exercise on appetite, ad libitum energy intake and appetite-regulatory hormones in lean and overweight/obese men and women. Int J Obes (Lond). 2017;41(12):1737-1744. doi:10.1038/ijo.2017.181 https://pubmed.ncbi.nlm.nih.gov/28769121/
Stensel D. Exercise, appetite and appetite-regulating hormones: implications for food intake and weight control. Ann Nutr Metab. 2010;57 Suppl 2:36-42. doi:10.1159/000322702 https://pubmed.ncbi.nlm.nih.gov/21346335/
Thackray AE, Deighton K, King JA, Stensel DJ. Exercise, Appetite and Weight Control: Are There Differences between Men and Women?. Nutrients. 2016;8(9):583. Published 2016 Sep 21. doi:10.3390/nu8090583 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037567/
Caruso L, Zauli E, Vaccarezza M. Physical Exercise and Appetite Regulation: New Insights. Biomolecules. 2023;13(8):1170. Published 2023 Jul 27. doi:10.3390/biom13081170 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10452291/
Martins C, Morgan L, Truby H. A review of the effects of exercise on appetite regulation: an obesity perspective. Int J Obes (Lond). 2008;32(9):1337-1347. doi:10.1038/ijo.2008.98 https://pubmed.ncbi.nlm.nih.gov/18607378/
Hargreaves M, Spriet LL. Exercise Metabolism: Fuels for the Fire. Cold Spring Harb Perspect Med. 2018;8(8):a029744. Published 2018 Aug 1. doi:10.1101/cshperspect.a029744 https://pubmed.ncbi.nlm.nih.gov/28533314/
Hargreaves M, Spriet LL. Skeletal muscle energy metabolism during exercise [published correction appears in Nat Metab. 2020 Sep 10;:]. Nat Metab. 2020;2(9):817-828. doi:10.1038/s42255-020-0251-4 https://pubmed.ncbi.nlm.nih.gov/32747792/
Spriet LL, Peters SJ. Influence of diet on the metabolic responses to exercise. Proc Nutr Soc. 1998;57(1):25-33. doi:10.1079/pns19980006 https://pubmed.ncbi.nlm.nih.gov/9571705/
Beck KL, Thomson JS, Swift RJ, von Hurst PR. Role of nutrition in performance enhancement and postexercise recovery. Open Access J Sports Med. 2015;6:259-267. Published 2015 Aug 11. doi:10.2147/OAJSM.S33605 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4540168/
Mata F, Valenzuela PL, Gimenez J, et al. Carbohydrate Availability and Physical Performance: Physiological Overview and Practical Recommendations. Nutrients. 2019;11(5):1084. Published 2019 May 16. doi:10.3390/nu11051084 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6566225/
Erlenbusch M, Haub M, Munoz K, MacConnie S, Stillwell B. Effect of high-fat or high-carbohydrate diets on endurance exercise: a meta-analysis. Int J Sport Nutr Exerc Metab. 2005;15(1):1-14. doi:10.1123/ijsnem.15.1.1 https://pubmed.ncbi.nlm.nih.gov/15902985/
Maughan RJ, Greenhaff PL, Leiper JB, Ball D, Lambert CP, Gleeson M. Diet composition and the performance of high-intensity exercise. J Sports Sci. 1997;15(3):265-275. doi:10.1080/026404197367272 https://pubmed.ncbi.nlm.nih.gov/9232552/
Kanter M. High-Quality Carbohydrates and Physical Performance: Expert Panel Report. Nutr Today. 2018;53(1):35-39. doi:10.1097/NT.0000000000000238 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5794245/
Rothschild JA, Kilding AE, Plews DJ. What Should I Eat before Exercise? Pre-Exercise Nutrition and the Response to Endurance Exercise: Current Prospective and Future Directions. Nutrients. 2020;12(11):3473. Published 2020 Nov 12. doi:10.3390/nu12113473 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7696145/
Neufer PD, Costill DL, Flynn MG, Kirwan JP, Mitchell JB, Houmard J. Improvements in exercise performance: effects of carbohydrate feedings and diet. J Appl Physiol (1985). 1987;62(3):983-988. doi:10.1152/jappl.1987.62.3.983 https://pubmed.ncbi.nlm.nih.gov/3571097/
Fleming J, Sharman MJ, Avery NG, et al. Endurance capacity and high-intensity exercise performance responses to a high fat diet. Int J Sport Nutr Exerc Metab. 2003;13(4):466-478. doi:10.1123/ijsnem.13.4.466 https://pubmed.ncbi.nlm.nih.gov/14967870/
Ribeiro AS, Nunes JP, Schoenfeld BJ, Aguiar AF, Cyrino ES. Effects of Different Dietary Energy Intake Following Resistance Training on Muscle Mass and Body Fat in Bodybuilders: A Pilot Study. J Hum Kinet. 2019;70:125-134. Published 2019 Nov 30. doi:10.2478/hukin-2019-0038 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6942464/
Cholewa JM, Newmire DE, Zanchi NE. Carbohydrate restriction: Friend or foe of resistance-based exercise performance?. Nutrition. 2019;60:136-146. doi:10.1016/j.nut.2018.09.026 https://pubmed.ncbi.nlm.nih.gov/30586657/
Ellerbroek A, Peacock CA, Orris S, et al. The effects of heavy resistance training and a high protein diet (3.4g/kg/d) on body composition, exercise performance and indices of health in resistance-trained individuals – a follow-up investigation. J Int Soc Sports Nutr. 2015;12(Suppl 1):P37. Published 2015 Sep 21. doi:10.1186/1550-2783-12-S1-P37 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4594935/
Bosse JD, Dixon BM. Dietary protein to maximize resistance training: a review and examination of protein spread and change theories. J Int Soc Sports Nutr. 2012;9(1):42. Published 2012 Sep 8. doi:10.1186/1550-2783-9-42 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3518828/
Helms ER, Zinn C, Rowlands DS, Brown SR. A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: a case for higher intakes. Int J Sport Nutr Exerc Metab. 2014;24(2):127-138. doi:10.1123/ijsnem.2013-0054 https://pubmed.ncbi.nlm.nih.gov/24092765/
Parr EB, Heilbronn LK, Hawley JA. A Time to Eat and a Time to Exercise. Exerc Sport Sci Rev. 2020;48(1):4-10. doi:10.1249/JES.0000000000000207 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6948807/
Matsumoto M, Narumi-Hyakutake A, Kakutani Y, et al. Evaluation of protein requirements using the indicator amino acid oxidation method: a scoping review. J Nutr. 2023;153(12):3472-3489. doi:10.1016/j.tjnut.2023.07.015 https://pubmed.ncbi.nlm.nih.gov/37573015/
Ruiz-Castellano C, Espinar S, Contreras C, Mata F, Aragon AA, Martínez-Sanz JM. Achieving an Optimal Fat Loss Phase in Resistance-Trained Athletes: A Narrative Review. Nutrients. 2021;13(9):3255. Published 2021 Sep 18. doi:10.3390/nu13093255 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8471721/
Bandegan A, Courtney-Martin G, Rafii M, Pencharz PB, Lemon PWR. Indicator amino acid oxidation protein requirement estimate in endurance-trained men 24 h postexercise exceeds both the EAR and current athlete guidelines. Am J Physiol Endocrinol Metab. 2019;316(5):E741-E748. doi:10.1152/ajpendo.00174.2018 https://pubmed.ncbi.nlm.nih.gov/30779631/
Mazzulla M, Abou Sawan S, Williamson E, et al. Protein Intake to Maximize Whole-Body Anabolism during Postexercise Recovery in Resistance-Trained Men with High Habitual Intakes is Severalfold Greater than the Current Recommended Dietary Allowance. J Nutr. 2020;150(3):505-511. doi:10.1093/jn/nxz249 https://pubmed.ncbi.nlm.nih.gov/31618421/
Wolfe RR, Kim IY, Park S, Ferrando A. Tracing metabolic flux to assess optimal dietary protein and amino acid consumption. Exp Mol Med. 2022;54(9):1323-1331. doi:10.1038/s12276-022-00817-w https://pubmed.ncbi.nlm.nih.gov/36075948/
Zhao, M., Tuo, H., Wang, S., & Zhao, L. (2020). The Effects of Dietary Nutrition on Sleep and Sleep Disorders. Mediators of Inflammation, 2020, 1–7. http://doi.org/10.1155/2020/3142874
Doherty, Madigan, Warrington, & Ellis. (2019). Sleep and Nutrition Interactions: Implications for Athletes. Nutrients, 11(4), 822. http://doi.org/10.3390/nu11040822
Sutanto CN, Wang MX, Tan D, Kim JE. Association of Sleep Quality and Macronutrient Distribution: A Systematic Review and Meta-Regression. Nutrients. 2020 Jan 2;12(1):126. doi: 10.3390/nu12010126. PMID: 31906452; PMCID: PMC7019667. https://pubmed.ncbi.nlm.nih.gov/31906452/
Peuhkuri, K., Sihvola, N., & Korpela, R. (2012). Diet promotes sleep duration and quality. Nutrition Research, 32(5), 309–319. http://doi.org/10.1016/j.nutres.2012.03.009
Afaghi, A., Oconnor, H., & Chow, C. M. (2007). High-glycemic-index carbohydrate meals shorten sleep onset. The American Journal of Clinical Nutrition, 85(2), 426–430. http://doi.org/10.1093/ajcn/85.2.426
Golem, D. L., Martin-Biggers, J. T., Koenings, M. M., Davis, K. F., & Byrd-Bredbenner, C. (2014). An Integrative Review of Sleep for Nutrition Professionals. Advances in Nutrition, 5(6), 742–759. http://doi.org/10.3945/an.114.006809
Grandner, M. A., Jackson, N., Gerstner, J. R., & Knutson, K. L. (2013). Sleep symptoms associated with intake of specific dietary nutrients. Journal of Sleep Research, 23(1), 22–34. http://doi.org/10.1111/jsr.12084
Porter, J., & Horne, J. (1981). Bed-time food supplements and sleep: Effects of different carbohydrate levels. Electroencephalography and Clinical Neurophysiology, 51(4), 426–433. http://doi.org/10.1016/0013-4694(81)90106-1
Halson, S. L. (2014). Sleep in Elite Athletes and Nutritional Interventions to Enhance Sleep. Sports Medicine, 44(S1), 13–23. http://doi.org/10.1007/s40279-014-0147-0
Takeda E, Terao J, Nakaya Y, et al. Stress control and human nutrition. J Med Invest. 2004;51(3-4):139-145. doi:10.2152/jmi.51.139 https://pubmed.ncbi.nlm.nih.gov/15460899/
Kipp D. Stress and nutrition. ASDC J Dent Child. 1985;52(1):68-71. https://pubmed.ncbi.nlm.nih.gov/3856595/
Gonzalez MJ, Miranda-Massari JR. Diet and stress. Psychiatr Clin North Am. 2014;37(4):579-589. doi:10.1016/j.psc.2014.08.004 https://pubmed.ncbi.nlm.nih.gov/25455067/
Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol. 2013;38(3):255-267. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4214609/
Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med. 2010;72(4):365-369. doi:10.1097/PSY.0b013e3181dbf489 https://pubmed.ncbi.nlm.nih.gov/20410248/
Bjørklund G, Chirumbolo S. Role of oxidative stress and antioxidants in daily nutrition and human health. Nutrition. 2017;33:311-321. doi:10.1016/j.nut.2016.07.018 https://pubmed.ncbi.nlm.nih.gov/27746034/
Hasan S, Fatima N, Bilal N, et al. Effect of chronic unpredictable stress on short term dietary restriction and its modulation by multivitamin-mineral supplementation. Appetite. 2013;65:68-74. doi:10.1016/j.appet.2013.02.003 https://pubmed.ncbi.nlm.nih.gov/23415982/
Bremner JD, Moazzami K, Wittbrodt MT, et al. Diet, Stress and Mental Health. Nutrients. 2020;12(8):2428. Published 2020 Aug 13. doi:10.3390/nu12082428 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468813/
Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81-121. doi:10.1007/s40279-013-0090-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894304/
Khaled, K., Tsofliou, F., Hundley, V. et al. Perceived stress and diet quality in women of reproductive age: a systematic review and meta-analysis. Nutr J 19, 92 (2020). https://doi.org/10.1186/s12937-020-00609-w
Lovallo WR, Farag NH, Vincent AS, Thomas TL, Wilson MF. Cortisol responses to mental stress, exercise, and meals following caffeine intake in men and women. Pharmacol Biochem Behav. 2006;83(3):441-447. doi:10.1016/j.pbb.2006.03.005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2249754/
Teychenne M, Stephens LD, Costigan SA, Olstad DL, Stubbs B, Turner AI. The association between sedentary behaviour and indicators of stress: a systematic review. BMC Public Health. 2019;19(1):1357. Published 2019 Oct 23. doi:10.1186/s12889-019-7717-x https://pubmed.ncbi.nlm.nih.gov/31647002/
Mastorakos G, Pavlatou M, Diamanti-Kandarakis E, Chrousos GP. Exercise and the stress system. Hormones (Athens). 2005;4(2):73-89. https://pubmed.ncbi.nlm.nih.gov/16613809/ Hamer M, Endrighi R, Poole L. Physical activity, stress reduction, and mood: insight into immunological mechanisms. Methods Mol Biol. 2012;934:89-102. doi:10.1007/978-1-62703-071-7_5 https://pubmed.ncbi.nlm.nih.gov/22933142/
Franklin BA, Rusia A, Haskin-Popp C, Tawney A. Chronic Stress, Exercise and Cardiovascular Disease: Placing the Benefits and Risks of Physical Activity into Perspective. Int J Environ Res Public Health. 2021;18(18):9922. Published 2021 Sep 21. doi:10.3390/ijerph18189922 https://pubmed.ncbi.nlm.nih.gov/34574843/
Childs E, de Wit H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front Physiol. 2014;5:161. Published 2014 May 1. doi:10.3389/fphys.2014.00161 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4013452/
Russell, V.A., Zigmond, M.J., Dimatelis, J.J. et al. The interaction between stress and exercise, and its impact on brain function. Metab Brain Dis 29, 255–260 (2014). https://doi.org/10.1007/s11011-013-9479-y https://link.springer.com/article/10.1007/s11011-013-9479-y
Loprinzi, P.D., Frith, E. Protective and therapeutic effects of exercise on stress-induced memory impairment. J Physiol Sci 69, 1–12 (2019). https://doi.org/10.1007/s12576-018-0638-0
Fillingim, R.B., Blumenthal, J.A. (1992). Does Aerobic Exercise Reduce Stress Responses?. In: Turner, J.R., Sherwood, A., Light, K.C. (eds) Individual Differences in Cardiovascular Response to Stress. Perspectives on Individual Differences. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-0697-7_11
Worthen M, Cash E. Stress Management. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 27, 2021. https://pubmed.ncbi.nlm.nih.gov/30020672/
Worthen M, Cash E. Stress Management. [Updated 2021 Aug 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513300/
Zamani-Alavijeh, F., Araban, M., Koohestani, H.R. et al. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetol Metab Syndr 10, 39 (2018). https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-018-0342-5