The next foundational sleep hygiene habit we must discuss in this series is consistent sleep and wake times. In the last article, we talked about tracking your sleep, learning to pay attention to the patterns that govern how well you rest, and building awareness of what actually affects your sleep quality versus what you assume affects it. Tracking is the diagnostic step, the foundation of informed action. But tracking alone changes nothing. You can meticulously log every night’s sleep for months and still wake up exhausted if you’re not actually doing anything differently.
This is where we shift from observation to intervention, and from understanding the problem to solving it. Over this series, we’re going to work through the essential sleep hygiene habits that actually move the needle on sleep quality. These are the practices that, when implemented properly, transform sleep from something you struggle with into something that reliably supports the life you’re trying to build.
Sleep hygiene conjures images of rigid rules and joyless optimisation, but properly understood, sleep hygiene is simply the art of working with your biology rather than against it. Your body already knows how to sleep brilliantly; it’s been doing it since you were born, governed by ancient mechanisms refined over millions of years of evolution. The problem is that modern life systematically disrupts these mechanisms, and most of us have normalised patterns that make good sleep unnecessarily difficult.
The habits we’ll cover in this series aren’t arbitrary rules invented by sleep researchers to make your life harder. They’re practical applications of what we know about how sleep actually works. Some will feel easy. Others will require genuine sacrifice. All of them work, provided you implement them consistently rather than cherry-picking the convenient bits whilst ignoring the difficult ones.
We’re starting with what is, for most people, the highest-yield habit you can adopt: maintaining consistent sleep and wake times. This is the foundation everything else builds on. It’s also, paradoxically, one of the habits people most frequently abandon because it conflicts with how we’ve been taught to think about freedom, spontaneity, and enjoying life. There’s something almost embarrassingly simple about the advice to go to bed and wake up at the same time every day. It sounds like the sort of thing your grandmother would tell you, right alongside eating your vegetables and standing up straight. And yet, when people actually implement this one habit, it tends to produce the kind of transformative results that send them looking for what else they’ve been missing.
The reason consistent sleep and wake times work so well isn’t mysterious. Your body operates on rhythms, ancient biological patterns that have been fine-tuned over evolutionary time to respond to the predictable cycle of light and dark. When you honour these rhythms, everything becomes easier. When you fight them, everything becomes harder. It’s that straightforward, though the implications run deeper than most people realise.
Table of Contents
- 1 Why Consistency is King: Understanding Your Circadian Rhythm
- 2 The Weekend Problem: Social Jet Lag Explained
- 3 Brutal Honesty About Trade-Offs
- 4 How to Actually Set Your Schedule
- 5 Making It Work in Real Life
- 6 The Wake Time Priority: Your Most Powerful Tool
- 7 The Bedtime Routine as Ritual
- 8 Troubleshooting When It Doesn’t Work
- 9 Consistent Sleep and Wake Times Conclusion
- 10 Author
Why Consistency is King: Understanding Your Circadian Rhythm
Circadian rhythm is one of the most powerful biological systems that governs our life, but most people are barely aware of it. And it’s not just about sleep; it governs body temperature, hormone secretion, immune function, metabolism, cognitive performance, and even when your body is most likely to repair damaged tissue or fight off pathogens. This rhythm exists in virtually every cell in your body, coordinated by a master clock in your brain’s suprachiasmatic nucleus that responds primarily to light exposure but also to feeding times, physical activity, and social cues.
The crucial point for those of us trying to improve sleep is that your circadian rhythm thrives on predictability. Think of it as a sophisticated timing system that needs to know what’s coming so it can prepare accordingly. When you go to bed at 10pm and wake at 7am consistently, your body doesn’t just passively accept this schedule. It actively works to support it, preparing for sleep hours before you actually lie down and preparing for waking before your alarm sounds.
About two hours before your habitual bedtime, assuming you’ve been consistent for at least a week or two, your body begins what sleep researchers call the “biological evening.” Your core temperature starts dropping from its daytime high, and this temperature decline is actually one of the signals that initiates sleepiness. The pineal gland ramps up melatonin production, with levels rising sharply about an hour before your usual bedtime. Certain neurotransmitters shift their activity. Your blood pressure decreases. Digestive processes slow. All of this happens automatically, orchestrated by your circadian clock, but only if your body has learned to trust that bedtime is actually coming at a consistent time.
If your schedule is erratic (e.g. 10 pm one night, midnight the next, 2 am on Friday, 11:30 pm on Sunday), your body can’t anticipate anything. The circadian system is like a conductor trying to lead an orchestra when the musicians might or might not show up, and the concert might start anywhere between 8 pm and midnight. It can’t coordinate the biological symphony that makes falling asleep easy because it doesn’t know when to cue the various instruments.
This is the fundamental difference between someone who falls asleep easily and someone who lies in bed for an hour actively willing themselves unconscious. It’s not willpower. It’s not some special talent for sleeping. It’s that their body knows what’s expected and has prepared the neurochemical ground accordingly. When you lie down at your consistent bedtime, you’re not fighting to fall asleep; you’re catching a wave your body has already created for you.
The same principle applies to waking, perhaps even more powerfully. When you wake at the same time every day, your circadian rhythm begins the wake-up process before you’re even conscious. Cortisol rises in what’s called the “cortisol awakening response,” peaking within thirty to forty-five minutes of your habitual wake time. This cortisol rise is natural and beneficial, and it is what increases alertness and mobilises energy for the day. Your body temperature rises from its nighttime low. Your brain reduces the production of sleep-promoting neurotransmitters and increases arousal-promoting ones. You shift from deeper to lighter sleep stages in anticipation of waking.
When this process unfolds predictably, you wake feeling relatively alert, perhaps not bright-eyed immediately, but certainly functional within minutes. But when your wake time is inconsistent, your body gets caught off guard. Sometimes you’re waking during deep slow-wave sleep, which leaves you feeling groggy and disoriented for hours (this is what researchers call “sleep inertia”). Sometimes during REM sleep, which can leave you foggy and emotionally off-kilter. Your cortisol hasn’t risen appropriately because your body didn’t know to prepare it. The result is that feeling of being dragged from the depths, that grogginess that even coffee struggles to cut through for the first part of your morning.
The Weekend Problem: Social Jet Lag Explained
Here’s where the conversation usually becomes uncomfortable, because this consistency needs to extend across your entire week. Weekends included. I know. Nobody wants to hear this. The weekend lie-in feels earned, justified, and necessary even, after a week of early alarms and obligations. Staying up late on Friday and Saturday feels like freedom, a brief respite from the tyranny of the schedule.
But what’s actually happening when you stay up until 2am on Saturday and sleep until 11am on Sunday is that you’re giving yourself the equivalent of flying from London to Delhi and back every single weekend. Sleep researchers call this “social jet lag”, which is the mismatch between your biological clock and your social clock, the difference between when your body wants to sleep and when your life allows it.
The mechanism is precise. If your weekday schedule has you sleeping from 10:30pm to 7am, your circadian rhythm has entrained to this pattern. Your melatonin rise is timed for around 9:30pm. Your cortisol awakening response is timed for 6:30-7am. But when you stay up until 2am on Saturday, you’re exposing yourself to light and activity during what your circadian system considers deep night. This light exposure (especially if it’s coming from screens) suppresses melatonin and shifts your circadian rhythm later.
Then you sleep until 11am, which means you’re getting light exposure four hours later than your weekday pattern. Light is the most powerful zeitgeber (time-giver) for your circadian rhythm, and late morning light shifts your rhythm even later. By Sunday evening, your circadian clock thinks bedtime is around 1-2am, not 10:30pm. When you try to sleep at 10:30pm Sunday night to prepare for Monday morning, your body essentially responds with “You’re joking, right? I’m not even slightly sleepy yet.”
The cost of this weekly disruption accumulates in ways people rarely connect to their weekend behaviour. Monday morning feels brutal, not just because it’s Monday, but because you’re waking several hours before your body thinks you should. You’re essentially experiencing jet lag without having travelled anywhere. This makes you irritable, cognitively slower, more prone to poor food choices, and less able to regulate your emotions.
But it doesn’t end Monday. Tuesday you’re still tired because you couldn’t fall asleep easily Monday night, because your rhythm hadn’t fully shifted back yet. Wednesday you’re starting to feel better, but still not quite right. Thursday you’re finally recovered, and then Friday evening arrives, and the cycle begins again. You’re spending the first half of every week recovering from the weekend and the last half building towards the next disruption. You’re perpetually playing catch-up with your own biology.
The research on social jet lag is quite sobering. Even controlling for sleep duration, people with a greater mismatch between weekday and weekend sleep schedules show increased risk of obesity, cardiovascular disease, metabolic dysfunction, and depression. The mechanism isn’t just about being tired; it’s about the chronic circadian disruption that affects every system in your body.
This doesn’t mean you can never stay up late or sleep in. Life is for living, and sometimes a late night with friends or a lazy Sunday morning is worth the cost. But it does mean understanding that there is a cost, and that your baseline pattern and your default when nothing special is happening needs to be consistent across the week. If every weekend means significant schedule disruption, you’re choosing to live in a state of perpetual mild jet lag, and then wondering why you never feel quite as good as you think you should.
Brutal Honesty About Trade-Offs
I know this discussion of sleep and wake times can feel quite abstract, and even quite condescending at times. So, we need to talk about what maintaining consistent sleep and wake times actually requires, because the conversation often stays too abstract. “Go to bed at the same time every night” sounds simple until you’re faced with the concrete reality of what that means for how you live.
It means that if your optimal bedtime is 10pm and you need thirty minutes to wind down, your evening social engagement needs to end by 9:30pm at the absolute latest. Not wrapping up. Ended. You leaving, saying goodnight, heading home. In practice, this means declining dinner invitations that start at 8pm. Leaving parties while they’re still in full swing. Missing the ends of films at the cinema. Saying no to spontaneous late-night plans with friends.
It means that on Friday and Saturday nights, when everyone else is staying up late without a care in the world because they can sleep in tomorrow, you’re still going to bed at your usual time. You’re watching your friends’ Instagram stories from their Friday night adventures while you’re doing your bedtime routine. You’re the one who leaves early, who doesn’t stay for “just one more,” who has to say “I’d love to, but I can’t” to things that sound genuinely fun.
It means waking at 7am on Saturday morning even though you could sleep in, even though you’re tired from the week, even though just once it would be nice to wake naturally without an alarm. It means Sunday mornings start at the same time as Tuesday mornings. It means Christmas morning and your birthday and lazy summer Sundays all begin at the same hour.
This is not small. The reason people struggle to maintain consistent sleep and wake times often isn’t lack of understanding or willpower; it’s that the social cost feels too high. Sleep regularity conflicts with how we’ve structured adult social life, which largely happens in the evenings and extends past what would be a reasonable bedtime for someone prioritising sleep. It conflicts with how we’ve come to think about weekends as time freed from constraints, including the constraint of a schedule.
Unfortunately, you need to own this choice. You cannot maintain consistent sleep and wake times while also maintaining all your current evening and weekend activities. Something has to give. This doesn’t mean you’re a prisoner of your sleep schedule, and you’re actually exercising freedom in choosing it. But freedom always involves constraint. Every choice is simultaneously a renunciation of other possibilities. Choosing consistent sleep means renouncing some of the social spontaneity and evening flexibility you might currently enjoy.
So, the question isn’t whether there’s a trade-off. There is. The real question is whether the trade-off is worth it for you, and ultimately, you’re the only person who can answer that for your life at this current point in time. But you must answer it honestly. Don’t pretend you can have both perfect sleep consistency and an unchanged social life whilst blaming your poor sleep on genetics or stress or your mattress. You’re choosing, whether you acknowledge it or not. The only question is whether you’re choosing deliberately or by default.
For some people, the trade is obviously worth it. They feel dramatically better with consistent sleep, and the activities they’re sacrificing weren’t bringing them much genuine satisfaction anyway; they were just habits or obligations dressed up as fun. For others, particularly younger people in life stages where social connection happens primarily through evening activities, the trade might not make sense right now. That’s fine. But then accept that your sleep will be somewhat compromised and stop expecting it to be perfect whilst you’re actively deprioritising it.
What doesn’t work is half-measures where you maintain consistency Monday through Thursday, blow it up Friday and Saturday, and then wonder why you feel awful. That pattern gives you the social sacrifice of consistent bedtimes without the biological benefit, because you’re still creating weekly jet lag. Better to acknowledge you’re not willing to maintain weekend consistency and at least minimise the damage by keeping weekend sleep schedule shifts to an hour or two rather than four or five. Minimise the damage, rather than try to mitigate it completely.
How to Actually Set Your Schedule
Now, setting consistent sleep and wake times isn’t conceptually complicated, but people consistently get the implementation wrong, which is why we need to walk through this precisely.
What you want to do is start with the one non-negotiable constraint most of us have: when you need to be awake and functional. If you need to be at work by 9am and you need an hour for your morning routine and commute, your wake time is 8am. Not “around 8am” or “8am-ish” or “sometime between 7:45 and 8:15.” Exactly 8am. Every day. This is your anchor point, the fixed star around which everything else rotates.
Now work backwards based on your actual sleep need. The standard recommendation is seven to nine hours for adults, but this is a range, not a target, and you probably have a sense from your sleep tracking where you fall. If you consistently feel good on eight hours and start feeling worse with seven (or even nine), eight is your number. If you genuinely need nine hours to feel properly rested, accept this rather than trying to somehow function on less because you think eight “should” be enough.
What most people get wrong is that if you need eight hours of sleep and wake at 8am, the answer is not a midnight bedtime. You need to be asleep for eight hours, which means you need to be in bed before midnight, and potentially well before that, depending on how long it takes you to fall asleep.
Most people, even with good sleep hygiene, take fifteen to twenty minutes to fall asleep. Some take longer, particularly if they’re anxious or have their mind racing about the next day. This means that to get eight hours of actual sleep from midnight to 8am, you need to be in bed with the lights off by 11:40pm at the absolute latest. And since you’re not a robot who can transition instantly from activity to lying in bed, you need a wind-down routine before that (we will talk more about wind down routines in the article series).
A realistic wind-down routine takes thirty to sixty minutes. This is time for showering, skincare, brushing teeth, setting up your bedroom, perhaps some reading or gentle stretching, and any transitional activities that signal to your body that sleep is approaching. If you need thirty minutes and want to be in bed by 11:40pm, your wind-down routine needs to begin by 11:10pm at the latest.
But you’re still not done with the calculation. You can’t be in the middle of something engaging at 11:10pm and simply drop it to start your routine. You need to have wrapped up your evening activities beforehand. This means dinner done, kitchen cleaned, any work finished, screens off, stimulating conversations concluded, all by about 11pm.
So here’s what “needing to wake at 8am and requiring eight hours of sleep” actually demands: your active evening needs to end by 11pm. Your wind-down routine runs from 11pm to 11:40pm. You’re in bed, lights off, by 11:40pm. You fall asleep by midnight. You wake at 8am having slept eight hours.
This is vastly different from how most people interpret “I need to be asleep by midnight,” which in practice means they start getting ready for bed at midnight, get into bed by 12:30am, scroll their phone until 1:30am, and then wonder why they feel terrible at 8am despite “getting enough time for sleep.”
The time in bed needs to exceed your sleep requirement by at least thirty minutes, probably forty-five, to account for sleep onset latency (time to fall asleep) and brief awakenings during the night that you might not even remember. If you need eight hours of sleep and only allocate exactly eight hours in bed, you’ll get seven to seven and a half hours of actual sleep, and you’ll be chronically underslept whilst insisting you’re giving yourself enough time.
Once you’ve calculated your proper bedtime and wake time, you need to commit to maintaining them seven days a week. This is non-negotiable if you want the full benefit. Your circadian rhythm doesn’t care that it’s Saturday. It can’t entrain to a pattern that exists five days a week and disappears for two.
If you’re currently on a significantly different schedule and need to shift to your new target times, do it gradually. Your circadian rhythm can adapt to changes of about fifteen to thirty minutes every few days without too much disruption. If you’re currently going to bed at 1am and want to shift to 10:30pm, don’t try to make the full shift at once. Move your bedtime to 12:45am for three or four days, then to 12:30am for a few more days, then to 12:15am, and so on. The process takes a few weeks, but you’ll actually succeed, whereas the “cold turkey” approach leaves you lying awake for hours at your new bedtime because your body isn’t ready.
When you mess up (and you will, because you’re human and life occasionally demands flexibility), the critical thing is your recovery strategy. If you stay up until 3am for whatever reason, the overwhelming temptation is to sleep in the next morning to “make up” the lost sleep. This feels intuitive. You’re tired. You need rest. Why wouldn’t you sleep longer?
Because “sleeping in” shifts your circadian rhythm later, which makes falling asleep at your normal bedtime tonight even harder. You’ll have less sleep pressure built up during the day. Your melatonin won’t rise at the usual time. You’ll lie awake tonight, sleep in again tomorrow, and within a few days, you’ve completely derailed your schedule.
The correct (albeit uncomfortable) response to a late night is to wake at your normal time regardless. Yes, you’ll be tired today. Very tired, possibly. But you’ll preserve your circadian rhythm. You’ll build strong sleep pressure throughout the day. Tonight, you’ll fall asleep easily at your normal bedtime and get a full night’s rest. One day of tiredness followed by rapid recovery is infinitely better than a week of disrupted sleep whilst you try to wrestle your schedule back into place.
This is hard. It requires accepting short-term discomfort (being tired today) to preserve long-term function (maintaining your rhythm). It requires trusting that the system works even when your immediate instinct says to sleep in. It requires the kind of discipline that doesn’t come naturally but pays exponential dividends.
Making It Work in Real Life
Now, the idealised version of consistent sleep and wake times works beautifully if you control every variable in your life. You don’t. You have a job with demands that don’t always respect your bedtime. You have relationships that matter, and sometimes maintaining them means staying up to have an important conversation or be present for someone in crisis. You might have children who fundamentally don’t care about your circadian rhythm. You have social obligations, family commitments, and unexpected emergencies.
This is where we separate the dogmatic from the pragmatic. Consistent sleep and wake times is a principle, not a prison. The goal is maintaining the pattern as your baseline while accepting that life will occasionally require deviation. The question is whether those deviations are genuinely necessary or merely convenient excuses.
Work schedule constraints are real, but they’re often more flexible than we pretend. If you habitually stay late at the office because there’s “always more to do,” you’re making a choice about what matters more. That’s fine, there are seasons of life where work legitimately takes priority, but you must own it. Don’t tell yourself you have no choice while simultaneously scrolling social media for thirty minutes during the workday or attending meetings that accomplish nothing. If work truly demands the hours, accept the trade-off. If it doesn’t, protect your evening boundaries.
Some jobs genuinely include unpredictable demands: doctors on call, emergency services, crisis counsellors, journalists covering breaking news. If this is your reality, you can’t maintain perfect consistency, but you can maintain a baseline schedule that you return to as quickly as possible after disruptions. The key is treating your schedule as the default that requires a genuine reason to deviate from, not a suggestion you follow when convenient.
Social life balance requires honest evaluation. If maintaining friendships genuinely requires staying out until midnight twice a week, you need to decide whether the relationships are worth the sleep cost. Often they are, and deep friendships are fundamental to wellbeing, and some phases of relationship-building require time together that conflicts with optimal sleep schedules. But be honest about whether you’re maintaining genuine connections or just following social scripts that don’t actually feed you.
There’s also the question of whether your social circle would adapt if you changed your behaviour. If you consistently left gatherings at 10pm instead of midnight, would people adjust and schedule things earlier, or would you be excluded? Sometimes the social cost is smaller than imagined. Sometimes it’s significant. But you won’t know until you actually try maintaining boundaries rather than assuming it’s impossible.
Family obligations, particularly with young children, genuinely constrain your ability to maintain perfect consistency. Small children don’t sleep on your schedule. They wake at unpredictable times with needs that don’t care about your REM cycle. They get sick. They have nightmares. They go through sleep regressions that disrupt everyone’s rest.
If you’re in this phase, beating yourself up about imperfect consistency helps nobody. Your job is to do what you can: maintain your wake time even when your toddler had you up three times in the night. Try to return to your bedtime routine as quickly as possible after disruptions. Accept that this season is temporary and that prioritising your child’s needs sometimes means sacrificing your ideal sleep schedule.
That said, many parents surrender more sleep than necessary by failing to establish boundaries around their children’s sleep. A three-year-old who’s learned that crying will bring parents running can disrupt sleep for years, whereas the same child, with consistent sleep training, might sleep through the night reliably. This is hard, it feels cruel to let your child cry, and it conflicts with certain parenting philosophies, but it’s worth considering whether you’re accepting disruption that doesn’t actually serve your child and destroys your well-being.
Shift workers face a fundamentally different challenge. Rotating shifts or irregular hours make consistent sleep and wake times in the traditional sense impossible. Your “morning” might be 4pm one week and midnight the next. This isn’t a matter of better discipline or trying harder, the work literally prevents circadian consistency.
The health consequences of shift work are well-documented and serious. The International Agency for Research on Cancer classifies shift work that involves circadian disruption as a probable carcinogen. We have robust evidence linking it to increased risk of cardiovascular disease, metabolic dysfunction, diabetes, depression, and even neurodegenerative diseases. This isn’t meant to terrify you if you work shifts, and you likely already know it’s hard on your body, but to acknowledge that you’re dealing with a legitimate biological stressor, not a failure of personal optimisation.
If you work shifts, the goal becomes creating micro-consistencies within your rotation. If you work nights for a week, maintain the same sleep schedule for that entire week. Use blackout curtains to control light exposure during daytime sleep. Consider light therapy to help shift your rhythm when your schedule changes. Prioritise sleep even more aggressively than day workers need to, because you’re already at a disadvantage.
And advocate for better shift schedules where possible. Rotating forward through shifts (day to evening to night) is easier on your circadian rhythm than rotating backward. Longer rotations (two or three weeks on the same shift) allow better entrainment than rapid rotation. Some shift patterns are genuinely more damaging than others, and employers who understand this can structure schedules that minimise harm whilst still covering necessary hours.
If you have any option to avoid shift work without sacrificing financial stability or career goals that matter to you, seriously consider it. The health cost is real and cumulative. But if shift work is your reality, optimise what you can while accepting what you can’t control.
Travel and jet lag are temporary disruptions that require their own strategy. When you cross time zones, your circadian rhythm needs to shift to match local time, and the faster you can accomplish this shift, the better you’ll feel and function.
The strategy here is that you want to immediately adopt the schedule of your destination, not some hybrid that tries to accommodate both zones. If you land in New York from London at noon local time, stay awake until a reasonable evening bedtime (say 10pm) even though your body thinks it’s 3am and you’re exhausted. Get bright light exposure during the local afternoon and evening. Avoid napping if possible, or limit it to twenty minutes maximum. The first day or two will be rough, but you’ll adapt much faster than if you try to split the difference.
When travelling east (harder on your circadian rhythm than west), get bright light exposure in the morning at your destination and avoid light in the evening. When travelling west, get light in the evening and avoid morning light until you’ve adapted. Melatonin supplementation can help, taken at the target bedtime for the first few nights, though its effectiveness varies.
For short trips (less than three or four days), you might choose to maintain your home schedule if the timezone difference is small and you have flexibility. But for trips of a week or more, adapt to local time completely. Your circadian rhythm will shift anyway through environmental cues; you might as well work with the process.
The Wake Time Priority: Your Most Powerful Tool
If life forces you to choose, and if you genuinely cannot maintain both consistent bedtime and consistent wake time, make your wake time the non-negotiable. This might seem counterintuitive. Surely it’s bedtime that matters, getting to sleep on time, allowing those crucial eight hours? But your circadian rhythm is actually more powerfully influenced by when you wake and expose yourself to light than by when you go to bed.
When you wake at the same time every day, even after a poor night’s sleep, you provide your circadian rhythm with its strongest and most reliable signal about when “day” begins. This matters more than any other single input because it sets the entire sequence of circadian events in motion. Your cortisol rises appropriately. Your body temperature begins climbing from its nighttime low. Your brain shifts neurotransmitter production from sleep-promoting to wake-promoting compounds.
More importantly, when you wake at the same time every day, you create consistent sleep pressure throughout the day. Sleep pressure (technically called adenosine accumulation) builds the longer you’re awake and is one of the two main drivers of sleepiness (the other being your circadian rhythm). If you wake at 7am every day, by 10pm you’ve been awake for fifteen hours and accumulated substantial sleep pressure. If you sometimes wake at 7am and sometimes sleep until 10am, your sleep pressure at any given evening hour is inconsistent, making falling asleep at a regular bedtime much harder.
This is why sleeping in after a bad night’s sleep, despite feeling like the natural remedy, often makes things worse. You get a bit more sleep that morning, which provides some recovery, but you’ve now shifted your circadian rhythm later and reduced the sleep pressure you’ll have accumulated by your target bedtime tonight. Tonight, you won’t feel sleepy at your usual time. You’ll stay up later, which shifts your rhythm later still. Within a few days, you’ve drifted into a later schedule that conflicts with your obligations.
The discipline of consistent wake times (even when you’re tired, even when you could sleep longer, and even when every fibre of your being wants just thirty more minutes) is one of those practices that feels punitive in the moment but pays exponential dividends over time. It’s a daily vote for the person you’re trying to become: the one who has their sleep sorted, who operates from a position of strength rather than perpetual depletion.
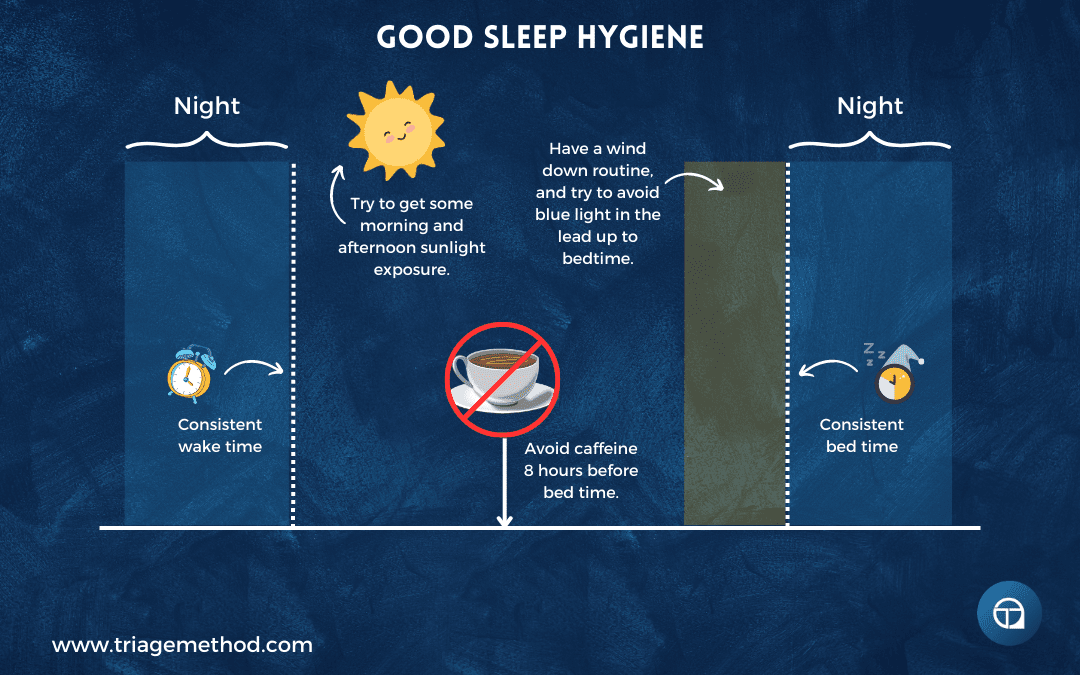
When you wake, light exposure is critical. Your circadian rhythm uses light as its primary time cue, and getting bright light into your eyes within the first hour of waking, and ideally within thirty minutes, provides the strongest possible signal that day has begun. This light exposure suppresses any residual melatonin from the night, provides an appropriate cortisol boost, and sets the timer for when melatonin will rise again roughly fourteen to sixteen hours later.
If it’s summer and the sun is already up when you wake, go outside. Five to ten minutes of natural outdoor light is more effective than any artificial light you can get indoors. If it’s winter or you wake before dawn, turn on bright lights throughout your home immediately upon waking. Sit near a window if there’s any natural light available. Consider a light therapy box (10,000 lux) if you’re serious about optimising your circadian rhythm, particularly if you struggle with morning darkness in winter.
The dose of light matters. Typical indoor lighting is 300-500 lux, which provides minimal circadian signal. Outdoor light on an overcast day is >10,000 lux. On a sunny day, it’s 50,000-100,000 lux. Your circadian system evolved to receive massive doses of light during the day, and indoor living has dramatically reduced this exposure. Getting outside for even a few minutes in the morning makes an enormous difference.
And resist the snooze button. I know it’s tempting. I know that those extra nine minutes feel precious. That half-asleep state between alarms can feel like a bonus rest you’ve earned. But what you’re actually doing is fragmenting sleep into pieces too short to be restorative while also confusing your circadian wake signal.
When you hit snooze, you’re entering light sleep that gets interrupted almost immediately. You’re not getting meaningful rest. You’re just delaying the inevitable while making waking harder. You’re also teaching your body that the alarm doesn’t actually mean it’s time to wake up, which makes every subsequent alarm less effective. Your body learns not to trust the signal, which means it doesn’t prepare the physiological wake-up process in anticipation of the alarm.
Set your alarm for when you actually need to get up. Then get up. If you need to wake more gently, consider an alarm that gradually increases volume or a dawn simulation alarm that gradually increases light in your room starting thirty minutes before your wake time. These can make the transition easier without fragmenting your sleep.
The Bedtime Routine as Ritual
Once you’ve established consistent sleep and wake times for a few weeks, something interesting happens: your bedtime routine becomes a powerful signal in its own right. This is basic Pavlovian conditioning at work. The very same mechanisms that made Pavlov’s dogs salivate at the sound of a bell, are the same processes your body uses to learn patterns throughout your life.
When you perform the same sequence of actions every night before bed (e.g. dim the lights at 9pm, wash your face at 9:30pm, brush your teeth at 9:45pm, read for twenty minutes, lights off at 10:15pm), your body begins associating these actions with sleep. After enough repetitions, just starting your bedtime routine triggers physiological changes that prepare you for sleep.
This isn’t mystical. It’s your brain recognising a pattern and responding appropriately. The routine becomes a series of cues that tell your body sleep is coming, which prompts the release of melatonin, a drop in core temperature, and the shift in neurotransmitter balance. What starts as a conscious decision of “I’m going to do these things before bed” becomes an automated trigger for the physiological cascade that makes sleep easy.
The power of ritual here can’t be overstated. Humans have used ritual to mark transitions for thousands of years because it works. Religious ceremonies, coming-of-age rites, pre-performance routines in athletics; these all leverage the brain’s pattern-recognition capacity to create psychological and physiological states that serve a purpose. Your bedtime routine is your personal ritual for transitioning from awake to sleeping, from engagement to rest. It deserves the same respect and consistency you’d give any practice that reliably improves your life.
This means starting your routine even if you don’t feel tired yet. In fact, especially if you don’t feel tired yet. You’re not waiting for sleepiness to begin the routine. The routine helps create sleepiness. If you wait until you’re falling asleep in the chair to start preparing for bed, you’ve missed the opportunity to use the routine as a tool.
The routine also serves a practical function, as it forces you to disengage from the stimulating activities of your evening and transition through progressively calming states. You can’t be in the middle of a heated social media debate or an intense work email at 10pm and then instantly fall asleep at 10:15pm. You need a bridge, a way to downregulate your nervous system from sympathetic (fight-or-flight) to parasympathetic (rest-and-digest) activation.
Your routine should be consistent in timing and sequence, but personalised to what actually relaxes you. Reading works for some people and makes others too alert. A hot bath or shower raises core temperature temporarily, which then drops afterwards and can promote sleepiness, but for some people it’s too stimulating. Gentle stretching, progressive muscle relaxation, journaling, meditation, etc. There are lots of options (which we will explore more in this series, but you will ultimately need to experiment to find what genuinely calms your mind without becoming so engaging that it keeps you awake.
The routine should also involve progressively dimming light, which we’ll cover in more detail in future articles in this series. For now, understand that bright light in the hours before bed suppresses melatonin and delays your circadian rhythm. Your routine should move you from normal room lighting to dimmer lighting to minimal lighting, mimicking the natural transition from day to evening to night that your circadian system evolved expecting.
Troubleshooting When It Doesn’t Work
Even with perfect implementation, you’ll encounter situations where maintaining consistent sleep and wake times creates problems. Let’s address the most common ones with actual solutions rather than platitudes.
You can’t fall asleep at your scheduled bedtime. This is incredibly frustrating because you’re doing everything “right,” you’re in bed at the right time, and sleep simply won’t come. Lying there for an hour, increasingly anxious about how little sleep you’re going to get, which makes sleep even less likely.
This usually means one of three things. First, you’re not actually tired enough because you haven’t been awake long enough or haven’t been active enough during the day. If you’re trying to sleep at 10pm after waking at 9am and spending the day sedentary, you haven’t built adequate sleep pressure. The solution is earlier wake times and more physical activity during the day.
Second, your sleep drive is being suppressed by light exposure, caffeine, or arousal too close to bedtime. We’ll cover this extensively in future articles, but the brief version is that bright light (especially blue wavelengths from screens) in the evening suppresses melatonin. Caffeine taken even six hours before bed can interfere with sleep onset. Intense exercise, stressful conversations, and stimulating content all can create arousal that persists past bedtime.
Third, you’ve developed conditioned arousal around your bed or bedtime. If you’ve spent months lying in bed frustrated and awake, your brain has learned to associate bed with arousal rather than sleep. The solution is stimulus control. If you’re not asleep within twenty to thirty minutes, get out of bed. Go to another room, keep the lights dim, do something calm and boring until you feel sleepy, then return to bed. Don’t stay in bed awake, strengthening the association between bed and wakefulness.
Paradoxically, sometimes the solution to consistently not falling asleep at your bedtime is reducing time in bed. If you’re spending nine hours in bed but only sleeping seven, your sleep efficiency is poor. Temporarily restricting time in bed to closer to your actual sleep duration (say, 7.5 hours) can increase sleep pressure and make falling asleep easier. Once you’re sleeping efficiently, you can gradually extend time in bed again.
You wake up before your alarm regularly. If this happens occasionally and you feel rested, it’s not a problem. Your sleep need that night was less than you allocated time for, and your body’s done what it needed to do. If it’s happening regularly and you wake feeling tired, something else is going on.
Early morning waking can indicate insufficient sleep pressure (you’re not awake long enough or active enough during the day), excessive sleep opportunity (you’re spending too much time in bed relative to your need), anxiety or stress that wakes you once sleep pressure has been partially relieved, or a circadian rhythm that’s shifted earlier than your schedule (you’re trying to sleep later than your body wants).
It can also be a sign of depression, sleep apnea, or other health issues. If early waking persists despite good sleep hygiene, particularly if it’s accompanied by difficulty getting back to sleep and daytime impairment, consult a healthcare provider.
Your chronotype doesn’t match your schedule. Some people are genuinely wired to fall asleep and wake later (evening chronotypes, “night owls”) or earlier (morning chronotypes, “larks”). This has a genetic component, and specific genes do influence circadian period length and light sensitivity. If you’re a strong evening type whose natural bedtime is 2am and natural wake time is 10am, but your job demands you wake at 6am, you’re working against your biology.
This is a real constraint, not a discipline failure. You can shift your rhythm somewhat through strategic light exposure, wake time consistency, and evening light avoidance, but you probably can’t turn a natural night owl into someone who bounces out of bed at 5am feeling energized. You’re managing a chronic mismatch.
Short of changing your job or hoping your employer embraces flexible hours (increasingly possible in many fields), you’re left doing damage control: maximising morning light exposure to shift your rhythm earlier, minimising evening light to avoid shifting it later, maintaining consistent wake times even on weekends, and accepting that you’re never going to feel as naturally alert in early morning as someone with an earlier chronotype.
This is worth advocating against when possible. School start times that demand teenagers (whose circadian rhythms naturally shift later during adolescence) wake at 6am are cruel and counterproductive. Work schedules that demand early presence for no operational reason are unnecessarily punishing to evening chronotypes. Where you have influence over your schedule, use it. Where you don’t, optimise what you can while accepting what you can’t change.
Your partner has a different schedule. This is genuinely difficult and requires negotiation rather than one person unilaterally imposing their schedule on the other. If one person’s ideal bedtime is 10pm and the other’s is midnight, someone’s compromising.
You do have options though. For example, maybe you go to bed at your bedtime while your partner stays up, and they come to bed quietly later, minimising disturbance. Maybe you both compromise on 11pm. Maybe you maintain different sleep locations for at least part of the week. Maybe you accept that relationship closeness sometimes means sacrificing optimal sleep, and that’s a trade you’re willing to make.
What doesn’t work is one person silently resenting the other while building chronic sleep debt. Talk about it. Find out what actually matters to each person. Is it falling asleep together, waking together, having evening time together, or having morning time together? You might discover that you can meet the core need without requiring identical sleep schedules.
Some couples find that separate bedrooms transform their relationship and their sleep. This goes against the romantic narrative that partners should share a bed, but if one person snores, moves frequently, runs hot, or keeps different hours, then separate sleep spaces might mean both people sleep better and are therefore better partners. It’s worth considering if sleep quality is genuinely suffering.
Children affect your schedule. Small children will disrupt your sleep. Newborns wake every few hours to feed. Toddlers have nightmares and illnesses. Even older children sometimes need parental attention at night. This is a fact of early parenthood, and no amount of sleep optimisation eliminates it.
The goal during this phase isn’t perfect consistency but maintaining as much structure as possible and recovering quickly from disruptions. If your two-year-old wakes you at 3am and keeps you up for an hour, you still wake at your normal time at 7am even though you’re exhausted. This preserves your circadian rhythm and makes it easier to sleep well the next night.
Maintain your bedtime routine even if it gets interrupted—start it again where you left off once the child settles. Protect your partner’s sleep when possible by taking turns with night wakings. Accept that you’ll accumulate some sleep debt during intense parenting phases and prioritise recovery when you can (the occasional weekend morning where your partner takes the kids and you sleep an extra hour can help without completely destroying your schedule).
As children get old enough for sleep training (and I acknowledge this is contentious and depends on your parenting philosophy), establishing consistent sleep schedules for them actually helps your sleep. A toddler with a predictable 7pm bedtime and 7am wake time creates predictable child-free evening time for you and removes the chaos of never knowing when you’ll get to start your evening.
Consistent Sleep and Wake Times Conclusion
Now, I want to end by pulling back to why this matters at a level beyond feeling less tired.
Poor sleep diminishes everything. It makes you irritable with people you love. It reduces your capacity for the difficult work that creates meaning in your life. It makes you reach for easy dopamine hits (scrolling, snacking, mindless entertainment, etc.), because you lack the executive function for anything more demanding. It narrows your window of tolerance for discomfort, which means you avoid hard conversations, challenging projects, and the very things that lead to growth.
When you’re chronically sleep-deprived, you’re not operating at a deficit across the board. Some functions decline more than others. Complex decision-making suffers. Emotional regulation suffers. Creative insight suffers. What remains intact is the ability to perform routine tasks, which means you can still go through the motions of your life while lacking the capacity for anything beyond that.
This is why fixing your sleep isn’t just about health metrics or feeling better; it’s about reclaiming your full capacity as a human being. Good sleep, the kind that comes from honouring your biology’s need for consistency, gives you back your agency. You have the energy to choose difficult things rather than defaulting to what’s easy. The patience to be kind when it’s hard rather than snapping at people who don’t deserve it. The mental clarity to work on what matters rather than just reacting to what’s urgent. The emotional resilience to face discomfort rather than avoiding anything that might require genuine effort.
This is about building the foundation for living well, not just existing. You cannot flourish while chronically sleep-deprived any more than a plant can flourish without water. The question isn’t whether you have time for consistent sleep and wake times (you’re sleeping anyway, just poorly) but whether you’re willing to prioritise it over the things currently stealing those hours.
Ultimately, you have more control here than you think you do. Not perfect control. Life intrudes, biology varies, and circumstances genuinely constrain. But you do have meaningful control. The choice to maintain consistent sleep and wake times, even when it’s inconvenient, even when you’d rather not, even when it conflicts with what you’d prefer to do with your evening, is a choice about who you’re becoming.
Every night you go to bed at your chosen time despite the pull of one more episode, one more scroll through social media, one more hour of unnecessary work, you’re voting for the person who has their foundations solid. Every morning you wake at your chosen time, despite being tired, despite wanting more sleep, despite the snooze button’s siren call, you’re voting for the person who operates from discipline rather than just following wherever impulse leads.
This isn’t optimisation for its own sake. This isn’t becoming a slave to your schedule or sacrificing all spontaneity on the altar of perfect sleep hygiene. This is reclaiming the capacity to live fully rather than perpetually operating at diminished capacity while wondering why life feels harder than it should.
You’re free to choose. You can choose to prioritise sleep consistency, accepting the social and scheduling constraints that come with it. You can choose to prioritise evening flexibility and weekend freedom, accepting the sleep quality consequences. What you cannot do is choose both while expecting your body to somehow transcend its biological requirements through force of will.
Most people haven’t genuinely chosen either path. They’ve drifted into patterns that serve neither sleep nor the things they’re supposedly staying up for. They sacrifice sleep for activities that don’t actually matter to them, like mindless scrolling, low-quality television, and staying up out of habit rather than genuine engagement. Then they wonder why they feel awful.
Start tonight. Calculate your actual required bedtime based on your wake time and sleep need. Look at what you’re doing in the hours before that bedtime and ask honestly: is this serving me? Is this in service of what I actually value? Or am I just filling time while sacrificing the foundation everything else builds on?
Tomorrow morning, wake at your chosen time regardless of how you slept. Get light in your eyes within thirty minutes. Notice how your body responds to consistency over the next week. Notice how much easier sleep becomes when your circadian rhythm knows what to expect. Notice how much more capacity you have when you’re properly rested.
This is the foundation. Everything else in this sleep series like light management, temperature optimisation, nutrition timing, stimulant use, and stress management, builds on this. You can implement every other intervention perfectly, but without consistent sleep and wake times, you’re building on sand.
Get this right first. Everything else becomes easier.
As with everything, there is always more to learn, and we haven’t even begun to scratch the surface with all this stuff. However, if you are interested in staying up to date with all our content, we recommend subscribing to our newsletter and bookmarking our free content page. We do have a lot of content on sleep in our sleep hub.
The previous article in this series was Tracking Your Sleep: Foundational Sleep Hygiene, and the next article in this series is Wind Down Routine: Foundational Sleep Hygiene.
If you would like more help with your training (or nutrition), we do also have online coaching spaces available.
We also recommend reading our foundational nutrition articles, along with our foundational articles on exercise and stress management, if you really want to learn more about how to optimise your lifestyle. If you want even more free information on sleep, you can follow us on Instagram, YouTube or listen to the podcast, where we discuss all the little intricacies of exercise.
Finally, if you want to learn how to coach nutrition, then consider our Nutrition Coach Certification course. We do also have an exercise program design course, if you are a coach who wants to learn more about effective program design and how to coach it. We do have other courses available too, notably a sleep course. If you don’t understand something, or you just need clarification, you can always reach out to us on Instagram or via email.
References and Further Reading
Vyazovskiy, V. (2015). Sleep, recovery, and metaregulation: explaining the benefits of sleep. Nature and Science of Sleep, 171. http://doi.org/10.2147/nss.s54036
Sharma, S., & Kavuru, M. (2010). Sleep and Metabolism: An Overview. International Journal of Endocrinology, 2010, 1–12. http://doi.org/10.1155/2010/270832
Yoo, S.-S., Gujar, N., Hu, P., Jolesz, F. A., & Walker, M. P. (2007). The human emotional brain without sleep — a prefrontal amygdala disconnect. Current Biology, 17(20). http://doi.org/10.1016/j.cub.2007.08.007
Copinschi G. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmacol. 2005;6(6):341-7. PMID: 16459757. https://pubmed.ncbi.nlm.nih.gov/16459757/
Spiegel, K., Leproult, R., L’Hermite-Balériaux, M., Copinschi, G., Penev, P. D., & Cauter, E. V. (2004). Leptin Levels Are Dependent on Sleep Duration: Relationships with Sympathovagal Balance, Carbohydrate Regulation, Cortisol, and Thyrotropin. The Journal of Clinical Endocrinology & Metabolism, 89(11), 5762–5771. http://doi.org/10.1210/jc.2004-1003
Nedeltcheva, A. V., Kilkus, J. M., Imperial, J., Kasza, K., Schoeller, D. A., & Penev, P. D. (2008). Sleep curtailment is accompanied by increased intake of calories from snacks. The American Journal of Clinical Nutrition, 89(1), 126–133. http://doi.org/10.3945/ajcn.2008.26574
Mullington, J. M., Chan, J. L., Dongen, H. P. A. V., Szuba, M. P., Samaras, J., Price, N. J., … Mantzoros, C. S. (2003). Sleep Loss Reduces Diurnal Rhythm Amplitude of Leptin in Healthy Men. Journal of Neuroendocrinology, 15(9), 851–854. http://doi.org/10.1046/j.1365-2826.2003.01069.x
Leproult, R., & Cauter, E. V. (2009). Role of Sleep and Sleep Loss in Hormonal Release and Metabolism. Pediatric Neuroendocrinology Endocrine Development, 11–21. http://doi.org/10.1159/000262524
Spaeth, A. M., Dinges, D. F., & Goel, N. (2013). Effects of Experimental Sleep Restriction on Weight Gain, Caloric Intake, and Meal Timing in Healthy Adults. Sleep, 36(7), 981–990. http://doi.org/10.5665/sleep.2792
Calvin, A. D., Carter, R. E., Adachi, T., Macedo, P. G., Albuquerque, F. N., Walt, C. V. D., … Somers, V. K. (2013). Effects of Experimental Sleep Restriction on Caloric Intake and Activity Energy Expenditure. Chest, 144(1), 79–86. http://doi.org/10.1378/chest.12-2829
Markwald, R. R., Melanson, E. L., Smith, M. R., Higgins, J., Perreault, L., Eckel, R. H., & Wright, K. P. (2013). Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proceedings of the National Academy of Sciences, 110(14), 5695–5700. http://doi.org/10.1073/pnas.1216951110
Cauter, E. V., Spiegel, K., Tasali, E., & Leproult, R. (2008). Metabolic consequences of sleep and sleep loss. Sleep Medicine, 9. http://doi.org/10.1016/s1389-9457(08)70013-3
Spiegel, K., Leproult, R., & Cauter, E. V. (1999). Impact of sleep debt on metabolic and endocrine function. The Lancet, 354(9188), 1435–1439. http://doi.org/10.1016/s0140-6736(99)01376-8
Ness, K. M., Strayer, S. M., Nahmod, N. G., Schade, M. M., Chang, A.-M., Shearer, G. C., & Buxton, O. M. (2019). Four nights of sleep restriction suppress the postprandial lipemic response and decrease satiety. Journal of Lipid Research, 60(11), 1935–1945. http://doi.org/10.1194/jlr.p094375
Hirotsu, C., Tufik, S., & Andersen, M. L. (2015). Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Science, 8(3), 143–152. http://doi.org/10.1016/j.slsci.2015.09.002
Morselli, L., Leproult, R., Balbo, M., & Spiegel, K. (2010). Role of sleep duration in the regulation of glucose metabolism and appetite. Best Practice & Research Clinical Endocrinology & Metabolism, 24(5), 687–702. http://doi.org/10.1016/j.beem.2010.07.005
Lamon, S., Morabito, A., Arentson-Lantz, E., Knowles, O., Vincent, G. E., Condo, D., … Aisbett, B. (2020). The effect of acute sleep deprivation on skeletal muscle protein synthesis and the hormonal environment. http://doi.org/10.1101/2020.03.09.984666
Lipton, J. O., & Sahin, M. (2014). The Neurology of mTOR. Neuron, 84(2), 275–291. http://doi.org/10.1016/j.neuron.2014.09.034
Tudor, J. C., Davis, E. J., Peixoto, L., Wimmer, M. E., Tilborg, E. V., Park, A. J., … Abel, T. (2016). Sleep deprivation impairs memory by attenuating mTORC1-dependent protein synthesis. Science Signaling, 9(425). http://doi.org/10.1126/scisignal.aad4949
Dattilo, M., Antunes, H., Medeiros, A., Neto, M. M., Souza, H., Tufik, S., & Mello, M. D. (2011). Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Medical Hypotheses, 77(2), 220–222. http://doi.org/10.1016/j.mehy.2011.04.017
Thornton, S. N., & Trabalon, M. (2014). Chronic dehydration is associated with obstructive sleep apnoea syndrome. Clinical Science, 128(3), 225–225. http://doi.org/10.1042/cs20140496
Rosinger, A. Y., Chang, A.-M., Buxton, O. M., Li, J., Wu, S., & Gao, X. (2018). Short sleep duration is associated with inadequate hydration: cross-cultural evidence from US and Chinese adults. Sleep, 42(2). http://doi.org/10.1093/sleep/zsy210
Watson, A. M. (2017). Sleep and Athletic Performance. Current Sports Medicine Reports, 16(6), 413–418. http://doi.org/10.1249/jsr.0000000000000418
Bonnar, D., Bartel, K., Kakoschke, N., & Lang, C. (2018). Sleep Interventions Designed to Improve Athletic Performance and Recovery: A Systematic Review of Current Approaches. Sports Medicine, 48(3), 683–703. http://doi.org/10.1007/s40279-017-0832-x
Saidi, O., Davenne, D., Lehorgne, C., & Duché, P. (2020). Effects of timing of moderate exercise in the evening on sleep and subsequent dietary intake in lean, young, healthy adults: randomized crossover study. European Journal of Applied Physiology, 120(7), 1551–1562. http://doi.org/10.1007/s00421-020-04386-6
Abedelmalek, S., Chtourou, H., Aloui, A., Aouichaoui, C., Souissi, N., & Tabka, Z. (2012). Effect of time of day and partial sleep deprivation on plasma concentrations of IL-6 during a short-term maximal performance. European Journal of Applied Physiology, 113(1), 241–248. http://doi.org/10.1007/s00421-012-2432-7
Azboy, O., & Kaygisiz, Z. (2009). Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiologica Hungarica, 96(1), 29–36. http://doi.org/10.1556/aphysiol.96.2009.1.3
Bird, S. P. (2013). Sleep, Recovery, and Athletic Performance. Strength and Conditioning Journal, 35(5), 43–47. http://doi.org/10.1519/ssc.0b013e3182a62e2f
Blumert, P. A., Crum, A. J., Ernsting, M., Volek, J. S., Hollander, D. B., Haff, E. E., & Haff, G. G. (2007). The Acute Effects of Twenty-Four Hours of Sleep Loss on the Performance of National-Caliber Male Collegiate Weightlifters. The Journal of Strength and Conditioning Research, 21(4), 1146. http://doi.org/10.1519/r-21606.1
Chase, J. D., Roberson, P. A., Saunders, M. J., Hargens, T. A., Womack, C. J., & Luden, N. D. (2017). One night of sleep restriction following heavy exercise impairs 3-km cycling time-trial performance in the morning. Applied Physiology, Nutrition, and Metabolism, 42(9), 909–915. http://doi.org/10.1139/apnm-2016-0698
Edwards, B. J., & Waterhouse, J. (2009). Effects of One Night of Partial Sleep Deprivation upon Diurnal Rhythms of Accuracy and Consistency in Throwing Darts. Chronobiology International, 26(4), 756–768. http://doi.org/10.1080/07420520902929037
Fullagar, H. H. K., Skorski, S., Duffield, R., Hammes, D., Coutts, A. J., & Meyer, T. (2014). Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise. Sports Medicine, 45(2), 161–186. http://doi.org/10.1007/s40279-014-0260-0
Gupta, L., Morgan, K., & Gilchrist, S. (2016). Does Elite Sport Degrade Sleep Quality? A Systematic Review. Sports Medicine, 47(7), 1317–1333. http://doi.org/10.1007/s40279-016-0650-6
Hausswirth, C., Louis, J., Aubry, A., Bonnet, G., Duffield, R., & Meur, Y. L. (2014). Evidence of Disturbed Sleep and Increased Illness in Overreached Endurance Athletes. Medicine & Science in Sports & Exercise, 46(5), 1036–1045. http://doi.org/10.1249/mss.0000000000000177
Mah, C. D., Mah, K. E., Kezirian, E. J., & Dement, W. C. (2011). The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players. Sleep, 34(7), 943–950. http://doi.org/10.5665/sleep.1132
Milewski, M. D., Skaggs, D. L., Bishop, G. A., Pace, J. L., Ibrahim, D. A., Wren, T. A., & Barzdukas, A. (2014). Chronic Lack of Sleep is Associated With Increased Sports Injuries in Adolescent Athletes. Journal of Pediatric Orthopaedics, 34(2), 129–133. http://doi.org/10.1097/bpo.0000000000000151
Mougin, F., Bourdin, H., Simon-Rigaud, M., Didier, J., Toubin, G., & Kantelip, J. (1996). Effects of a Selective Sleep Deprivation on Subsequent Anaerobic Performance. International Journal of Sports Medicine, 17(02), 115–119. http://doi.org/10.1055/s-2007-972818
Oliver, S. J., Costa, R. J. S., Laing, S. J., Bilzon, J. L. J., & Walsh, N. P. (2009). One night of sleep deprivation decreases treadmill endurance performance. European Journal of Applied Physiology, 107(2), 155–161. http://doi.org/10.1007/s00421-009-1103-9
Pallesen, S., Gundersen, H. S., Kristoffersen, M., Bjorvatn, B., Thun, E., & Harris, A. (2017). The Effects of Sleep Deprivation on Soccer Skills. Perceptual and Motor Skills, 124(4), 812–829. http://doi.org/10.1177/0031512517707412
Reilly, T., & Piercy, M. (1994). The effect of partial sleep deprivation on weight-lifting performance. Ergonomics, 37(1), 107–115. http://doi.org/10.1080/00140139408963628
Rossa, K. R., Smith, S. S., Allan, A. C., & Sullivan, K. A. (2014). The Effects of Sleep Restriction on Executive Inhibitory Control and Affect in Young Adults. Journal of Adolescent Health, 55(2), 287–292. http://doi.org/10.1016/j.jadohealth.2013.12.034
Sargent, C., & Roach, G. D. (2016). Sleep duration is reduced in elite athletes following night-time competition. Chronobiology International, 33(6), 667–670. http://doi.org/10.3109/07420528.2016.1167715
Skein, M., Duffield, R., Edge, J., Short, M. J., & Mündel, T. (2011). Intermittent-Sprint Performance and Muscle Glycogen after 30 h of Sleep Deprivation. Medicine & Science in Sports & Exercise, 43(7), 1301–1311. http://doi.org/10.1249/mss.0b013e31820abc5a
Souissi, N., Sesboüé, B., Gauthier, A., Larue, J., & Davenne, D. (2003). Effects of one nights sleep deprivation on anaerobic performance the following day. European Journal of Applied Physiology, 89(3), 359–366. http://doi.org/10.1007/s00421-003-0793-7
Caia, J., Kelly, V. G., & Halson, S. L. (2017). The role of sleep in maximising performance in elite athletes. Sport, Recovery, and Performance, 151–167. http://doi.org/10.4324/9781315268149-11
Alley, J. R., Mazzochi, J. W., Smith, C. J., Morris, D. M., & Collier, S. R. (2015). Effects of Resistance Exercise Timing on Sleep Architecture and Nocturnal Blood Pressure. Journal of Strength and Conditioning Research, 29(5), 1378–1385. http://doi.org/10.1519/jsc.0000000000000750
Kovacevic, A., Mavros, Y., Heisz, J. J., & Singh, M. A. F. (2018). The effect of resistance exercise on sleep: A systematic review of randomized controlled trials. Sleep Medicine Reviews, 39, 52–68. http://doi.org/10.1016/j.smrv.2017.07.002
Herrick, J. E., Puri, S., & Richards, K. C. (2017). Resistance training does not alter same-day sleep architecture in institutionalized older adults. Journal of Sleep Research, 27(4). http://doi.org/10.1111/jsr.12590
Edinger, J. D., Morey, M. C., Sullivan, R. J., Higginbotham, M. B., Marsh, G. R., Dailey, D. S., & McCall, W. V. (1993). Aerobic fitness, acute exercise and sleep in older men. Sleep, 16(4), 351-359. https://doi.org/10.1093/sleep/16.4.351
King, A. C. (1997). Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. JAMA: The Journal of the American Medical Association, 277(1), 32–37. http://doi.org/10.1001/jama.277.1.32
Passos, G. S., Poyares, D., Santana, M. G., Garbuio, S. A., Tufik, S., & Mello, M. T. (2010). Effect of Acute Physical Exercise on Patients with Chronic Primary Insomnia. Journal of Clinical Sleep Medicine, 06(03), 270–275. http://doi.org/10.5664/jcsm.27825
Reid, K. J., Baron, K. G., Lu, B., Naylor, E., Wolfe, L., & Zee, P. C. (2010). Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Medicine, 11(9), 934–940. http://doi.org/10.1016/j.sleep.2010.04.014
Viana, V. A. R., Esteves, A. M., Boscolo, R. A., Grassmann, V., Santana, M. G., Tufik, S., & Mello, M. T. D. (2011). The effects of a session of resistance training on sleep patterns in the elderly. European Journal of Applied Physiology, 112(7), 2403–2408. http://doi.org/10.1007/s00421-011-2219-2
Herring, M., Kline, C., & Oconnor, P. (2015). Effects of Exercise Training On Self-reported Sleep Among Young Women with Generalized Anxiety Disorder (GAD). European Psychiatry, 30, 465. http://doi.org/10.1016/s0924-9338(15)31893-9
Kredlow, M. A., Capozzoli, M. C., Hearon, B. A., Calkins, A. W., & Otto, M. W. (2015). The effects of physical activity on sleep: a meta-analytic review. Journal of Behavioral Medicine, 38(3), 427–449. http://doi.org/10.1007/s10865-015-9617-6
Yang, P.-Y., Ho, K.-H., Chen, H.-C., & Chien, M.-Y. (2012). Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. Journal of Physiotherapy, 58(3), 157–163. http://doi.org/10.1016/s1836-9553(12)70106-6
Kline, C. E., Sui, X., Hall, M. H., Youngstedt, S. D., Blair, S. N., Earnest, C. P., & Church, T. S. (2012). Dose–response effects of exercise training on the subjective sleep quality of postmenopausal women: exploratory analyses of a randomised controlled trial. BMJ Open, 2(4). http://doi.org/10.1136/bmjopen-2012-001044
Fairbrother, K., Cartner, B. W., Triplett, N., Morris, D. M., & Collier, S. R. (2011). The Effects of Aerobic Exercise Timing on Sleep Architecture. Medicine & Science in Sports & Exercise, 43(Suppl 1), 879. http://doi.org/10.1249/01.mss.0000402452.16375.20
Youngstedt, S. D., & Kline, C. E. (2006). Epidemiology of exercise and sleep. Sleep and Biological Rhythms, 4(3), 215–221. http://doi.org/10.1111/j.1479-8425.2006.00235.x
Stenholm, S., Head, J., Kivimäki, M., Hanson, L. L. M., Pentti, J., Rod, N. H., … Vahtera, J. (2018). Sleep Duration and Sleep Disturbances as Predictors of Healthy and Chronic Disease–Free Life Expectancy Between Ages 50 and 75: A Pooled Analysis of Three Cohorts. The Journals of Gerontology: Series A, 74(2), 204–210. http://doi.org/10.1093/gerona/gly01
Xiao, Q., Keadle, S. K., Hollenbeck, A. R., & Matthews, C. E. (2014). Sleep Duration and Total and Cause-Specific Mortality in a Large US Cohort: Interrelationships With Physical Activity, Sedentary Behavior, and Body Mass Index. American Journal of Epidemiology, 180(10), 997–1006. http://doi.org/10.1093/aje/kwu222
Reynolds, A. C., Dorrian, J., Liu, P. Y., Dongen, H. P. A. V., Wittert, G. A., Harmer, L. J., & Banks, S. (2012). Impact of Five Nights of Sleep Restriction on Glucose Metabolism, Leptin and Testosterone in Young Adult Men. PLoS ONE, 7(7). http://doi.org/10.1371/journal.pone.0041218
Åkerstedt, T., Palmblad, J., Torre, B. D. L., Marana, R., & Gillberg, M. (1980). Adrenocortical and Gonadal Steroids During Sleep Deprivation. Sleep, 3(1), 23–30. http://doi.org/10.1093/sleep/3.1.23
Cortés-Gallegos, V., Castañeda, G., Alonso, R., Sojo, I., Carranco, A., Cervantes, C., & Parra, A. (1983). Sleep Deprivation Reduces Circulating Androgens in Healthy Men. Archives of Andrology, 10(1), 33–37. http://doi.org/10.3109/01485018308990167
González-Santos, M. R., Gajá-Rodíguez, O. V., Alonso-Uriarte, R., Sojo-Aranda, I., & Cortés-Gallegos, V. (1989). Sleep Deprivation and Adaptive Hormonal Responses of Healthy Men. Archives of Andrology, 22(3), 203–207. http://doi.org/10.3109/01485018908986773
Penev, P. D. (2007). Association Between Sleep and Morning Testosterone Levels In Older Men. Sleep, 30(4), 427–432. http://doi.org/10.1093/sleep/30.4.427
Kloss, J. D., Perlis, M. L., Zamzow, J. A., Culnan, E. J., & Gracia, C. R. (2015). Sleep, sleep disturbance, and fertility in women. Sleep Medicine Reviews, 22, 78–87. http://doi.org/10.1016/j.smrv.2014.10.005
Mahoney, M. M. (2010). Shift Work, Jet Lag, and Female Reproduction. International Journal of Endocrinology, 2010, 1–9. http://doi.org/10.1155/2010/813764
Labyak, S., Lava, S., Turek, F., & Zee, P. (2002). Effects Of Shiftwork On Sleep And Menstrual Function In Nurses. Health Care for Women International, 23(6-7), 703–714. http://doi.org/10.1080/07399330290107449
Pal, L., Bevilacqua, K., Zeitlian, G., Shu, J., & Santoro, N. (2008). Implications of diminished ovarian reserve (DOR) extend well beyond reproductive concerns. Menopause, 15(6), 1086–1094. http://doi.org/10.1097/gme.0b013e3181728467
Axelsson, G., Rylander, R., & Molin, I. (1989). Outcome of pregnancy in relation to irregular and inconvenient work schedules. Occupational and Environmental Medicine, 46(6), 393–398. http://doi.org/10.1136/oem.46.6.393
Bisanti, L., Olsen, J., Basso, O., Thonneau, P., & Karmaus, W. (1996). Shift Work and Subfecundity: A European Multicenter Study. Journal of Occupational & Environmental Medicine, 38(4), 352–358. http://doi.org/10.1097/00043764-199604000-00012
Rossmanith, W. G. (1998). The impact of sleep on gonadotropin secretion. Gynecological Endocrinology, 12(6), 381–389. http://doi.org/10.3109/09513599809012840
Fernando, S., & Rombauts, L. (2014). Melatonin: shedding light on infertility? – a review of the recent literature. Journal of Ovarian Research, 7(1). http://doi.org/10.1186/s13048-014-0098-y
Rocha, C., Rato, L., Martins, A., Alves, M., & Oliveira, P. (2015). Melatonin and Male Reproductive Health: Relevance of Darkness and Antioxidant Properties. Current Molecular Medicine, 15(4), 299–311. http://doi.org/10.2174/1566524015666150505155530
Song, C., Peng, W., Yin, S., Zhao, J., Fu, B., Zhang, J., … Zhang, Y. (2016). Melatonin improves age-induced fertility decline and attenuates ovarian mitochondrial oxidative stress in mice. Scientific Reports, 6(1). http://doi.org/10.1038/srep35165
Espino, J., Macedo, M., Lozano, G., Ortiz, Á., Rodríguez, C., Rodríguez, A. B., & Bejarano, I. (2019). Impact of Melatonin Supplementation in Women with Unexplained Infertility Undergoing Fertility Treatment. Antioxidants, 8(9), 338. http://doi.org/10.3390/antiox8090338
Tamura, H., Takasaki, A., Taketani, T., Tanabe, M., Kizuka, F., Lee, L., … Sugino, N. (2012). The role of melatonin as an antioxidant in the follicle. Journal of Ovarian Research, 5(1), 5. http://doi.org/10.1186/1757-2215-5-5
Saaresranta, T., & Polo, O. (2003). Sleep-disordered breathing and hormones. European Respiratory Journal, 22(1), 161–172. http://doi.org/10.1183/09031936.03.00062403
Cappuccio, F. P., Cooper, D., Delia, L., Strazzullo, P., & Miller, M. A. (2011). Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal, 32(12), 1484–1492. http://doi.org/10.1093/eurheartj/ehr007
Jansen, E. C., Dunietz, G. L., Tsimpanouli, M.-E., Guyer, H. M., Shannon, C., Hershner, S. D., … Baylin, A. (2018). Sleep, Diet, and Cardiometabolic Health Investigations: a Systematic Review of Analytic Strategies. Current Nutrition Reports, 7(4), 235–258. http://doi.org/10.1007/s13668-018-0240-3
Knutson, K. L., Cauter, E. V., Rathouz, P. J., Yan, L. L., Hulley, S. B., Liu, K., & Lauderdale, D. S. (2009). Association Between Sleep and Blood Pressure in Midlife. Archives of Internal Medicine, 169(11), 1055. http://doi.org/10.1001/archinternmed.2009.119
Besedovsky, L., Lange, T., & Born, J. (2011). Sleep and immune function. Pflügers Archiv – European Journal of Physiology, 463(1), 121–137. http://doi.org/10.1007/s00424-011-1044-0
Besedovsky, L., Lange, T., & Haack, M. (2019). The Sleep-Immune Crosstalk in Health and Disease. Physiological Reviews, 99(3), 1325–1380. http://doi.org/10.1152/physrev.00010.2018
Orr, W. C., Fass, R., Sundaram, S. S., & Scheimann, A. O. (2020). The effect of sleep on gastrointestinal functioning in common digestive diseases. The Lancet Gastroenterology & Hepatology, 5(6), 616–624. http://doi.org/10.1016/s2468-1253(19)30412-1
Tang, Y., Preuss, F., Turek, F. W., Jakate, S., & Keshavarzian, A. (2009). Sleep deprivation worsens inflammation and delays recovery in a mouse model of colitis. Sleep Medicine, 10(6), 597–603. http://doi.org/10.1016/j.sleep.2008.12.009
Chen, Y., Tan, F., Wei, L., Li, X., Lyu, Z., Feng, X., … Li, N. (2018). Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose–response relationship. BMC Cancer, 18(1). http://doi.org/10.1186/s12885-018-5025-y
Almendros, I., Martinez-Garcia, M. A., Farré, R., & Gozal, D. (2020). Obesity, sleep apnea, and cancer. International Journal of Obesity, 44(8), 1653–1667. http://doi.org/10.1038/s41366-020-0549-z
Erren, T. C., Falaturi, P., Morfeld, P., Knauth, P., Reiter, R. J., & Piekarski, C. (2010). Shift Work and Cancer. Deutsches Aerzteblatt Online. http://doi.org/10.3238/arztebl.2010.0657
Bernert, R. A., Kim, J. S., Iwata, N. G., & Perlis, M. L. (2015). Sleep Disturbances as an Evidence-Based Suicide Risk Factor. Current Psychiatry Reports, 17(3). http://doi.org/10.1007/s11920-015-0554-4
Kim, J.-H., Park, E.-C., Cho, W.-H., Park, J.-Y., Choi, W.-J., & Chang, H.-S. (2013). Association between Total Sleep Duration and Suicidal Ideation among the Korean General Adult Population. Sleep, 36(10), 1563–1572. http://doi.org/10.5665/sleep.3058
Mccall, W. V., & Black, C. G. (2013). The Link Between Suicide and Insomnia: Theoretical Mechanisms. Current Psychiatry Reports, 15(9). http://doi.org/10.1007/s11920-013-0389-9
Li, S. X., Lam, S. P., Zhang, J., Yu, M. W. M., Chan, J. W. Y., Chan, C. S. Y., … Wing, Y.-K. (2016). Sleep Disturbances and Suicide Risk in an 8-Year Longitudinal Study of Schizophrenia-Spectrum Disorders. Sleep, 39(6), 1275–1282. http://doi.org/10.5665/sleep.5852
Littlewood, D. L., Gooding, P., Kyle, S. D., Pratt, D., & Peters, S. (2016). Understanding the role of sleep in suicide risk: qualitative interview study. BMJ Open, 6(8). http://doi.org/10.1136/bmjopen-2016-012113
Lin, H.-T., Lai, C.-H., Perng, H.-J., Chung, C.-H., Wang, C.-C., Chen, W.-L., & Chien, W.-C. (2018). Insomnia as an independent predictor of suicide attempts: a nationwide population-based retrospective cohort study. BMC Psychiatry, 18(1). http://doi.org/10.1186/s12888-018-1702-2
Freeman, D., Sheaves, B., Waite, F., Harvey, A. G., & Harrison, P. J. (2020). Sleep disturbance and psychiatric disorders. The Lancet Psychiatry, 7(7), 628–637. http://doi.org/10.1016/s2215-0366(20)30136-x
Benca, R. M. (1992). Sleep and Psychiatric Disorders. Archives of General Psychiatry, 49(8), 651. http://doi.org/10.1001/archpsyc.1992.01820080059010
Breslau, N., Roth, T., Rosenthal, L., & Andreski, P. (1996). Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young Adults. Biological Psychiatry, 39(6), 411–418. http://doi.org/10.1016/0006-3223(95)00188-3
Baglioni, C., Nanovska, S., Regen, W., Spiegelhalder, K., Feige, B., Nissen, C., … Riemann, D. (2016). Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychological Bulletin, 142(9), 969–990. http://doi.org/10.1037/bul0000053
Goldstein, A. N., & Walker, M. P. (2014). The Role of Sleep in Emotional Brain Function. Annual Review of Clinical Psychology, 10(1), 679–708. http://doi.org/10.1146/annurev-clinpsy-032813-153716
Postuma, R. B., Iranzo, A., Hu, M., Högl, B., Boeve, B. F., Manni, R., … Pelletier, A. (2019). Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain, 142(3), 744–759. http://doi.org/10.1093/brain/awz030
Wintler, T., Schoch, H., Frank, M. G., & Peixoto, L. (2020). Sleep, brain development, and autism spectrum disorders: Insights from animal models. Journal of Neuroscience Research, 98(6), 1137–1149. http://doi.org/10.1002/jnr.24619
Shokri-Kojori, E., Wang, G.-J., Wiers, C. E., Demiral, S. B., Guo, M., Kim, S. W., … Volkow, N. D. (2018). β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences, 115(17), 4483–4488. http://doi.org/10.1073/pnas.1721694115
Mantovani, S., Smith, S. S., Gordon, R., & Osullivan, J. D. (2018). An overview of sleep and circadian dysfunction in Parkinsons disease. Journal of Sleep Research, 27(3). http://doi.org/10.1111/jsr.12673
Malhotra, R. K. (2018). Neurodegenerative Disorders and Sleep. Sleep Medicine Clinics, 13(1), 63–70. http://doi.org/10.1016/j.jsmc.2017.09.006
Huang, L.-B., Tsai, M.-C., Chen, C.-Y., & Hsu, S.-C. (2013). The Effectiveness of Light/Dark Exposure to Treat Insomnia in Female Nurses Undertaking Shift Work during the Evening/Night Shift. Journal of Clinical Sleep Medicine, 09(07), 641–646. http://doi.org/10.5664/jcsm.2824
Zhang, Y., & Papantoniou, K. (2019). Night shift work and its carcinogenicity. The Lancet Oncology, 20(10). http://doi.org/10.1016/s1470-2045(19)30578-9
Perry-Jenkins, M., Goldberg, A. E., Pierce, C. P., & Sayer, A. G. (2007). Shift Work, Role Overload, and the Transition to Parenthood. Journal of Marriage and Family, 69(1), 123–138. http://doi.org/10.1111/j.1741-3737.2006.00349.x
Rodziewicz TL, Hipskind JE. Medical Error Prevention. 2020 May 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 29763131. https://pubmed.ncbi.nlm.nih.gov/29763131/
Tanaka, K., Takahashi, M., Hiro, H., Kakinuma, M., Tanaka, M., Kamata, N., & Miyaoka, H. (2010). Differences in Medical Error Risk among Nurses Working Two- and Three-shift Systems at Teaching Hospitals: A Six-month Prospective Study. Industrial Health, 48(3), 357–364. http://doi.org/10.2486/indhealth.48.357
Admi H, Tzischinsky O, Epstein R, Herer P, Lavie P. Shift work in nursing: is it really a risk factor for nurses’ health and patients’ safety?. Nurs Econ. 2008;26(4):250-257. https://pubmed.ncbi.nlm.nih.gov/18777974/
Clendon, J., & Gibbons, V. (2015). 12h shifts and rates of error among nurses: A systematic review. International Journal of Nursing Studies, 52(7), 1231–1242. http://doi.org/10.1016/j.ijnurstu.2015.03.011
Hammadah, M., Kindya, B. R., Allard‐Ratick, M. P., Jazbeh, S., Eapen, D., Tang, W. W., & Sperling, L. (2017). Navigating air travel and cardiovascular concerns: Is the sky the limit?, Clinical Cardiology, 40 (9), 660–666. http://doi.org/10.1002/clc.22741
Lieber, B. A., Han, J., Appelboom, G., Taylor, B. E., Han, B., Agarwal, N., & Connolly, E. S. (2016). Association of Steroid Use with Deep Venous Thrombosis and Pulmonary Embolism in Neurosurgical Patients: A National Database Analysis. World Neurosurgery, 89, 126–132. http://doi.org/10.1016/j.wneu.2016.01.033
El-Menyar, A., Asim, M., & Al-Thani, H. (2017). Obesity Paradox in Patients With Deep Venous Thrombosis. Clinical and Applied Thrombosis/Hemostasis, 24(6), 986–992. http://doi.org/10.1177/1076029617727858
Klovaite, J., Benn, M., & Nordestgaard, B. G. (2014). Obesity as a causal risk factor for deep venous thrombosis: a Mendelian randomization study. Journal of Internal Medicine, 277(5), 573–584. http://doi.org/10.1111/joim.12299
Davies, H. O., Popplewell, M., Singhal, R., Smith, N., & Bradbury, A. W. (2016). Obesity and lower limb venous disease – The epidemic of phlebesity. Phlebology: The Journal of Venous Disease, 32(4), 227–233. http://doi.org/10.1177/0268355516649333
Liljeqvist, S., Helldén, A., Bergman, U., & Söderberg, M. (2008). Pulmonary embolism associated with the use of anabolic steroids. European Journal of Internal Medicine, 19(3), 214–215. http://doi.org/10.1016/j.ejim.2007.03.016
Linton MF, Yancey PG, Davies SS, Jerome WG (Jay), Linton EF, Vickers KC. The Role of Lipids and Lipoproteins in Atherosclerosis. In: De Groot LJ, Chrousos G, Dungan K, et al., eds. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000. http://www.ncbi.nlm.nih.gov/books/NBK343489/.
Rescheduling of meals may ease the effects of jet lag. (2017). Nursing Standard, 31(48), 16–16. http://doi.org/10.7748/ns.31.48.16.s17
Ruscitto, C., & Ogden, J. (2016). The impact of an implementation intention to improve mealtimes and reduce jet lag in long-haul cabin crew. Psychology & Health, 32(1), 61–77. http://doi.org/10.1080/08870446.2016.1240174
Reid, K. J., & Abbott, S. M. (2015). Jet Lag and Shift Work Disorder. Sleep Medicine Clinics, 10(4), 523–535. http://doi.org/10.1016/j.jsmc.2015.08.006
Srinivasan, V., Spence, D. W., Pandi-Perumal, S. R., Trakht, I., & Cardinali, D. P. (2008). Jet lag: Therapeutic use of melatonin and possible application of melatonin analogs. Travel Medicine and Infectious Disease, 6(1-2), 17–28. http://doi.org/10.1016/j.tmaid.2007.12.002
Edwards, B. J., Atkinson, G., Waterhouse, J., Reilly, T., Godfrey, R., & Budgett, R. (2000). Use of melatonin in recovery from jet-lag following an eastward flight across 10 time-zones. Ergonomics, 43(10), 1501–1513. http://doi.org/10.1080/001401300750003934
Zee, P. C., & Goldstein, C. A. (2010). Treatment of Shift Work Disorder and Jet Lag. Current Treatment Options in Neurology, 12(5), 396–411. http://doi.org/10.1007/s11940-010-0090-9
https://www.nhlbi.nih.gov/health-topics/circadian-rhythm-disorders
Borodkin, K., & Dagan, Y. (2013). Diagnostic Algorithm for Circadian Rhythm Sleep Disorders. Encyclopedia of Sleep, 66–73. http://doi.org/10.1016/b978-0-12-378610-4.00284-9
Lockley, S. (2013). Special Considerations and Future Directions in Circadian Rhythm Sleep Disorders Diagnosis. Encyclopedia of Sleep, 138–149. http://doi.org/10.1016/b978-0-12-378610-4.00299-0
Crowley, S., & Youngstedt, S. (2013). Pathophysiology, Associations, and Consequences of Circadian Rhythm Sleep Disorder. Encyclopedia of Sleep, 16–21. http://doi.org/10.1016/b978-0-12-378610-4.00266-7
Franken, P., & Dijk, D.-J. (2009). Circadian clock genes and sleep homeostasis. European Journal of Neuroscience, 29(9), 1820–1829. http://doi.org/10.1111/j.1460-9568.2009.06723.x
Burgess, H. J., & Emens, J. S. (2016). Circadian-Based Therapies for Circadian Rhythm Sleep-Wake Disorders. Current Sleep Medicine Reports, 2(3), 158–165. http://doi.org/10.1007/s40675-016-0052-1
Jones, C. R., Huang, A. L., Ptáček, L. J., & Fu, Y.-H. (2013). Genetic basis of human circadian rhythm disorders. Experimental Neurology, 243, 28–33. http://doi.org/10.1016/j.expneurol.2012.07.012
Toh KL. Basic science review on circadian rhythm biology and circadian sleep disorders. Ann Acad Med Singap. 2008;37(8):662-668. https://pubmed.ncbi.nlm.nih.gov/18797559/
Farhud D, Aryan Z. Circadian Rhythm, Lifestyle and Health: A Narrative Review. Iran J Public Health. 2018;47(8):1068-1076. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6123576/
Dodson, E. R., & Zee, P. C. (2010). Therapeutics for Circadian Rhythm Sleep Disorders. Sleep Medicine Clinics, 5(4), 701–715. http://doi.org/10.1016/j.jsmc.2010.08.001
Zhu, L., & Zee, P. C. (2012). Circadian Rhythm Sleep Disorders. Neurologic Clinics, 30(4), 1167–1191. http://doi.org/10.1016/j.ncl.2012.08.011
Kim MJ, Lee JH, Duffy JF. Circadian Rhythm Sleep Disorders. J Clin Outcomes Manag. 2013;20(11):513-528. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4212693/
Zhong, G., Naismith, S. L., Rogers, N. L., & Lewis, S. J. G. (2011). Sleep-wake disturbances in common neurodegenerative diseases: A closer look at selected aspects of the neural circuitry. Journal of the Neurological Sciences, 307(1-2), 9–14. http://doi.org/10.1016/j.jns.2011.04.020
Dijk, D.-J., Boulos, Z., Eastman, C. I., Lewy, A. J., Campbell, S. S., & Terman, M. (1995). Light Treatment for Sleep Disorders: Consensus Report. Journal of Biological Rhythms, 10(2), 113–125. http://doi.org/10.1177/074873049501000204
Barion, A., & Zee, P. C. (2007). A clinical approach to circadian rhythm sleep disorders. Sleep Medicine, 8(6), 566–577. http://doi.org/10.1016/j.sleep.2006.11.017
Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4(2):97-110. https://pubmed.ncbi.nlm.nih.gov/1027738/
Adan, A., & Almirall, H. (1991). Horne & Östberg morningness-eveningness questionnaire: A reduced scale. Personality and Individual Differences, 12(3), 241–253. http://doi.org/10.1016/0191-8869(91)90110-w
Urbán, R., Magyaródi, T., & Rigó, A. (2011). Morningness-Eveningness, Chronotypes and Health-Impairing Behaviors in Adolescents. Chronobiology International, 28(3), 238–247. http://doi.org/10.3109/07420528.2010.549599
https://www.thewep.org/documentations/mctq
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. http://doi.org/10.1016/0165-1781(89)90047-4
Bastien, C. (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. http://doi.org/10.1016/s1389-9457(00)00065-4
Yang, M., Morin, C. M., Schaefer, K., & Wallenstein, G. V. (2009). Interpreting score differences in the Insomnia Severity Index: using health-related outcomes to define the minimally important difference. Current Medical Research and Opinion, 25(10), 2487–2494. http://doi.org/10.1185/03007990903167415
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep, 34(5), 601–608. http://doi.org/10.1093/sleep/34.5.601
Castriotta RJ, Wilde MC, Lai JM, Atanasov S, Masel BE, Kuna ST. Prevalence and consequences of sleep disorders in traumatic brain injury. J Clin Sleep Med. 2007;3(4):349-356. https://pubmed.ncbi.nlm.nih.gov/17694722/
Chokroverty S. Overview of sleep & sleep disorders. Indian J Med Res. 2010;131:126-140. https://pubmed.ncbi.nlm.nih.gov/20308738/
Pavlova, M. K., & Latreille, V. (2019). Sleep Disorders. The American Journal of Medicine, 132(3), 292–299. http://doi.org/10.1016/j.amjmed.2018.09.021
Olejniczak, P. W., & Fisch, B. J. (2003). Sleep disorders. Medical Clinics of North America, 87(4), 803–833. http://doi.org/10.1016/s0025-7125(03)00006-3
https://www.nhlbi.nih.gov/health-topics/sleep-apnea
https://clevemed.com/what-is-sleep-apnea/patient-sleep-apnea-screener/
Spicuzza, L., Caruso, D., & Maria, G. D. (2015). Obstructive sleep apnoea syndrome and its management. Therapeutic Advances in Chronic Disease, 6(5), 273–285. http://doi.org/10.1177/2040622315590318
Bixler, E. O., Vgontzas, A. N., Lin, H.-M., Liao, D., Calhoun, S., Fedok, F., … Graff, G. (2008). Blood Pressure Associated With Sleep-Disordered Breathing in a Population Sample of Children. Hypertension, 52(5), 841–846. http://doi.org/10.1161/hypertensionaha.108.116756
Campos, A. I., García-Marín, L. M., Byrne, E. M., Martin, N. G., Cuéllar-Partida, G., & Rentería, M. E. (2020). Insights into the aetiology of snoring from observational and genetic investigations in the UK Biobank. Nature Communications, 11(1). http://doi.org/10.1038/s41467-020-14625-1
Morgenthaler, T. I., Kagramanov, V., Hanak, V., & Decker, P. A. (2006). Complex Sleep Apnea Syndrome: Is It a Unique Clinical Syndrome? Sleep, 29(9), 1203–1209. http://doi.org/10.1093/sleep/29.9.1203
El-Ad, B., & Lavie, P. (2005). Effect of sleep apnea on cognition and mood. International Review of Psychiatry, 17(4), 277–282. http://doi.org/10.1080/09540260500104508
Morgenstern, M., Wang, J., Beatty, N., Batemarco, T., Sica, A. L., & Greenberg, H. (2014). Obstructive Sleep Apnea. Endocrinology and Metabolism Clinics of North America, 43(1), 187–204. http://doi.org/10.1016/j.ecl.2013.09.002
Sleep–Related Breathing Disorders in Adults: Recommendations for Syndrome Definition and Measurement Techniques in Clinical Research. (1999). Sleep, 22(5), 667–689. http://doi.org/10.1093/sleep/22.5.667
Ruehland, W. R., Rochford, P. D., O’Donoghue, F. J., Pierce, R. J., Singh, P., & Thornton, A. T. (2009). The New AASM Criteria for Scoring Hypopneas: Impact on the Apnea Hypopnea Index. Sleep, 32(2), 150–157. http://doi.org/10.1093/sleep/32.2.150
Selim, B. J., Koo, B. B., Qin, L., Jeon, S., Won, C., Redeker, N. S., … Yaggi, H. K. (2016). The Association between Nocturnal Cardiac Arrhythmias and Sleep-Disordered Breathing: The DREAM Study. Journal of Clinical Sleep Medicine, 12(06), 829–837. http://doi.org/10.5664/jcsm.5880
Ahmed, M. H. (2010). Obstructive sleep apnea syndrome and fatty liver: Association or causal link? World Journal of Gastroenterology, 16(34), 4243. http://doi.org/10.3748/wjg.v16.i34.4243
Singh, H., Pollock, R., Uhanova, J., Kryger, M., Hawkins, K., & Minuk, G. Y. (2005). Symptoms of Obstructive Sleep Apnea in Patients with Nonalcoholic Fatty Liver Disease. Digestive Diseases and Sciences, 50(12), 2338–2343. http://doi.org/10.1007/s10620-005-3058-y
Lawati, N. M. A., Patel, S. R., & Ayas, N. T. (2009). Epidemiology, Risk Factors, and Consequences of Obstructive Sleep Apnea and Short Sleep Duration. Progress in Cardiovascular Diseases, 51(4), 285–293. http://doi.org/10.1016/j.pcad.2008.08.001
Young, T. (2004). Risk Factors for Obstructive Sleep Apnea in Adults. Jama, 291(16), 2013. http://doi.org/10.1001/jama.291.16.2013
Yaggi, H. K., Concato, J., Kernan, W. N., Lichtman, J. H., Brass, L. M., & Mohsenin, V. (2005). Obstructive Sleep Apnea as a Risk Factor for Stroke and Death. New England Journal of Medicine, 353(19), 2034–2041. http://doi.org/10.1056/nejmoa043104
Redline, S., Budhiraja, R., Kapur, V., Marcus, C. L., Mateika, J. H., Mehra, R., … Quan, A. S. F. (2007). The Scoring of Respiratory Events in Sleep: Reliability and Validity. Journal of Clinical Sleep Medicine, 03(02), 169–200. http://doi.org/10.5664/jcsm.26818
Basheer B, Hegde KS, Bhat SS, Umar D, Baroudi K. Influence of mouth breathing on the dentofacial growth of children: a cephalometric study. J Int Oral Health. 2014;6(6):50-55. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295456/
Ruhle, K. H., & Nilius, G. (2008). Mouth Breathing in Obstructive Sleep Apnea prior to and during Nasal Continuous Positive Airway Pressure. Respiration, 76(1), 40–45. http://doi.org/10.1159/000111806
Izu, S. C., Itamoto, C. H., Pradella-Hallinan, M., Pizarro, G. U., Tufik, S., Pignatari, S., & Fujita, R. R. (2010). Obstructive sleep apnea syndrome (OSAS) in mouth breathing children. Brazilian Journal of Otorhinolaryngology, 76(5), 552–556. http://doi.org/10.1590/s1808-86942010000500003
Lee, S. H., Choi, J. H., Shin, C., Lee, H. M., Kwon, S. Y., & Lee, S. H. (2007). How Does Open-Mouth Breathing Influence Upper Airway Anatomy? The Laryngoscope, 117(6), 1102–1106. http://doi.org/10.1097/mlg.0b013e318042aef7
Tuomilehto, H. P. I., Seppä, J. M., Partinen, M. M., Peltonen, M., Gylling, H., Tuomilehto, J. O. I., … Uusitupa, M. (2009). Lifestyle Intervention with Weight Reduction. American Journal of Respiratory and Critical Care Medicine, 179(4), 320–327. http://doi.org/10.1164/rccm.200805-669oc
https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
Neill, A. M., Angus, S. M., Sajkov, D., & Mcevoy, R. D. (1997). Effects of sleep posture on upper airway stability in patients with obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine, 155(1), 199–204. http://doi.org/10.1164/ajrccm.155.1.9001312
Loord, H., & Hultcrantz, E. (2007). Positioner–a method for preventing sleep apnea. Acta Oto-Laryngologica, 127(8), 861–868. http://doi.org/10.1080/00016480601089390
Szollosi, I., Roebuck, T., Thompson, B., & Naughton, M. T. (2006). Lateral Sleeping Position Reduces Severity of Central Sleep Apnea / Cheyne-Stokes Respiration. Sleep, 29(8), 1045–1051. http://doi.org/10.1093/sleep/29.8.1045
Silverberg DS, Iaina A, Oksenberg A. Treating obstructive sleep apnea improves essential hypertension and quality of life. Am Fam Physician. 2002;65(2):229-236. https://pubmed.ncbi.nlm.nih.gov/11820487/
Aurora, R. N., Chowdhuri, S., Ramar, K., Bista, S. R., Casey, K. R., Lamm, C. I., … Tracy, S. L. (2012). The Treatment of Central Sleep Apnea Syndromes in Adults: Practice Parameters with an Evidence-Based Literature Review and Meta-Analyses. Sleep, 35(1), 17–40. http://doi.org/10.5665/sleep.1580
Hsu, A. A. L., & Lo, C. (2003). Continuous positive airway pressure therapy in sleep apnoea. Respirology, 8(4), 447–454. http://doi.org/10.1046/j.1440-1843.2003.00494.x
Patel, S. R., White, D. P., Malhotra, A., Stanchina, M. L., & Ayas, N. T. (2003). Continuous Positive Airway Pressure Therapy for Treating gess in a Diverse Population With Obstructive Sleep Apnea. Archives of Internal Medicine, 163(5), 565. http://doi.org/10.1001/archinte.163.5.565
Sundaram, S., Lim, J., & Lasserson, T. J. (2005). Surgery for obstructive sleep apnoea in adults. Cochrane Database of Systematic Reviews. http://doi.org/10.1002/14651858.cd001004.pub2
Chen, H., & Lowe, A. A. (2012). Updates in oral appliance therapy for snoring and obstructive sleep apnea. Sleep and Breathing, 17(2), 473–486. http://doi.org/10.1007/s11325-012-0712-4
Gaisl, T., Haile, S. R., Thiel, S., Osswald, M., & Kohler, M. (2019). Efficacy of pharmacotherapy for OSA in adults: A systematic review and network meta-analysis. Sleep Medicine Reviews, 46, 74–86. http://doi.org/10.1016/j.smrv.2019.04.009
Ohayon, M., Wickwire, E. M., Hirshkowitz, M., Albert, S. M., Avidan, A., Daly, F. J., … Vitiello, M. V. (2017). National Sleep Foundations sleep quality recommendations: first report. Sleep Health, 3(1), 6–19. http://doi.org/10.1016/j.sleh.2016.11.006
Youngstedt, S. D., Goff, E. E., Reynolds, A. M., Kripke, D. F., Irwin, M. R., Bootzin, R. R., … Jean-Louis, G. (2016). Has adult sleep duration declined over the last 50 years? Sleep Medicine Reviews, 28, 69–85. http://doi.org/10.1016/j.smrv.2015.08.004
Chaput, J.-P., Mcneil, J., Després, J.-P., Bouchard, C., & Tremblay, A. (2013). Seven to Eight Hours of Sleep a Night Is Associated with a Lower Prevalence of the Metabolic Syndrome and Reduced Overall Cardiometabolic Risk in Adults. PLoS ONE, 8(9). http://doi.org/10.1371/journal.pone.0072832
Wild, C. J., Nichols, E. S., Battista, M. E., Stojanoski, B., & Owen, A. M. (2018). Dissociable effects of self-reported daily sleep duration on high-level cognitive abilities. Sleep, 41(12). http://doi.org/10.1093/sleep/zsy182
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., Doncarlos, L., … Hillard, P. J. A. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40–43. http://doi.org/10.1016/j.sleh.2014.12.010
Cappuccio, F. P., Delia, L., Strazzullo, P., & Miller, M. A. (2010). Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep, 33(5), 585–592. http://doi.org/10.1093/sleep/33.5.585
Gottlieb, D. J., Punjabi, N. M., Newman, A. B., Resnick, H. E., Redline, S., Baldwin, C. M., & Nieto, F. J. (2005). Association of Sleep Time With Diabetes Mellitus and Impaired Glucose Tolerance. Archives of Internal Medicine, 165(8), 863. http://doi.org/10.1001/archinte.165.8.863
Short, M. A., Agostini, A., Lushington, K., & Dorrian, J. (2015). A systematic review of the sleep, sleepiness, and performance implications of limited wake shift work schedules. Scandinavian Journal of Work, Environment & Health, 41(5), 425–440. http://doi.org/10.5271/sjweh.3509
Cappuccio, F. P., Taggart, F. M., Kandala, N.-B., Currie, A., Peile, E., Stranges, S., & Miller, M. A. (2008). Meta-Analysis of Short Sleep Duration and Obesity in Children and Adults. Sleep, 31(5), 619–626. http://doi.org/10.1093/sleep/31.5.619
Mong, J. A., & Cusmano, D. M. (2016). Sex differences in sleep: impact of biological sex and sex steroids. Philosophical Transactions of the Royal Society B: Biological Sciences, 371(1688), 20150110. http://doi.org/10.1098/rstb.2015.0110
Krishnan, V., & Collop, N. A. (2006). Gender differences in sleep disorders. Current Opinion in Pulmonary Medicine, 12(6), 383–389. http://doi.org/10.1097/01.mcp.0000245705.69440.6a
Mehta, N., Shafi, F., & Bhat, A. (2015). Unique Aspects of Sleep in Women. Missouri medicine, 112(6), 430–434. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6168103/
Moline, M. L., Broch, L., & Zak, R. (2004). Sleep in women across the life cycle from adulthood through menopause. Medical Clinics of North America, 88(3), 705–736. http://doi.org/10.1016/j.mcna.2004.01.009
He, Y., Jones, C. R., Fujiki, N., Xu, Y., Guo, B., Holder, J. L., … Fu, Y.-H. (2009). The Transcriptional Repressor DEC2 Regulates Sleep Length in Mammals. Science, 325(5942), 866–870. http://doi.org/10.1126/science.1174443
Theorell-Haglöw, J., Berglund, L., Berne, C., & Lindberg, E. (2014). Both habitual short sleepers and long sleepers are at greater risk of obesity: a population-based 10-year follow-up in women. Sleep Medicine, 15(10), 1204–1211. http://doi.org/10.1016/j.sleep.2014.02.014
Mezick, E. J., Wing, R. R., & Mccaffery, J. M. (2014). Associations of self-reported and actigraphy-assessed sleep characteristics with body mass index and waist circumference in adults: moderation by gender. Sleep Medicine, 15(1), 64–70. http://doi.org/10.1016/j.sleep.2013.08.784
Kim, S. J. (2011). Relationship Between Weekend Catch-up Sleep and Poor Performance on Attention Tasks in Korean Adolescents. Archives of Pediatrics & Adolescent Medicine, 165(9), 806. http://doi.org/10.1001/archpediatrics.2011.128
Kim, C.-W., Choi, M.-K., Im, H.-J., Kim, O.-H., Lee, H.-J., Song, J., … Park, K.-H. (2012). Weekend catch-up sleep is associated with decreased risk of being overweight among fifth-grade students with short sleep duration. Journal of Sleep Research, 21(5), 546–551. http://doi.org/10.1111/j.1365-2869.2012.01013.x
Sun, W., Ling, J., Zhu, X., Lee, T. M.-C., & Li, S. X. (2019). Associations of weekday-to-weekend sleep differences with academic performance and health-related outcomes in school-age children and youths. Sleep Medicine Reviews, 46, 27–53. http://doi.org/10.1016/j.smrv.2019.04.003
Kang, S.-G., Lee, Y. J., Kim, S. J., Lim, W., Lee, H.-J., Park, Y.-M., … Hong, J. P. (2014). Weekend catch-up sleep is independently associated with suicide attempts and self-injury in Korean adolescents. Comprehensive Psychiatry, 55(2), 319–325. http://doi.org/10.1016/j.comppsych.2013.08.023
Zhao, M., Tuo, H., Wang, S., & Zhao, L. (2020). The Effects of Dietary Nutrition on Sleep and Sleep Disorders. Mediators of Inflammation, 2020, 1–7. http://doi.org/10.1155/2020/3142874
Doherty, Madigan, Warrington, & Ellis. (2019). Sleep and Nutrition Interactions: Implications for Athletes. Nutrients, 11(4), 822. http://doi.org/10.3390/nu11040822
Sutanto CN, Wang MX, Tan D, Kim JE. Association of Sleep Quality and Macronutrient Distribution: A Systematic Review and Meta-Regression. Nutrients. 2020 Jan 2;12(1):126. doi: 10.3390/nu12010126. PMID: 31906452; PMCID: PMC7019667. https://pubmed.ncbi.nlm.nih.gov/31906452/
Peuhkuri, K., Sihvola, N., & Korpela, R. (2012). Diet promotes sleep duration and quality. Nutrition Research, 32(5), 309–319. http://doi.org/10.1016/j.nutres.2012.03.009
Afaghi, A., Oconnor, H., & Chow, C. M. (2007). High-glycemic-index carbohydrate meals shorten sleep onset. The American Journal of Clinical Nutrition, 85(2), 426–430. http://doi.org/10.1093/ajcn/85.2.426
Golem, D. L., Martin-Biggers, J. T., Koenings, M. M., Davis, K. F., & Byrd-Bredbenner, C. (2014). An Integrative Review of Sleep for Nutrition Professionals. Advances in Nutrition, 5(6), 742–759. http://doi.org/10.3945/an.114.006809
Grandner, M. A., Jackson, N., Gerstner, J. R., & Knutson, K. L. (2013). Sleep symptoms associated with intake of specific dietary nutrients. Journal of Sleep Research, 23(1), 22–34. http://doi.org/10.1111/jsr.12084
Porter, J., & Horne, J. (1981). Bed-time food supplements and sleep: Effects of different carbohydrate levels. Electroencephalography and Clinical Neurophysiology, 51(4), 426–433. http://doi.org/10.1016/0013-4694(81)90106-1
Halson, S. L. (2014). Sleep in Elite Athletes and Nutritional Interventions to Enhance Sleep. Sports Medicine, 44(S1), 13–23. http://doi.org/10.1007/s40279-014-0147-0
Rondanelli, M., Opizzi, A., Monteferrario, F., Antoniello, N., Manni, R., & Klersy, C. (2011). The Effect of Melatonin, Magnesium, and Zinc on Primary Insomnia in Long-Term Care Facility Residents in Italy: A Double-Blind, Placebo-Controlled Clinical Trial. Journal of the American Geriatrics Society, 59(1), 82–90. http://doi.org/10.1111/j.1532-5415.2010.03232.x
Tahara, Y., & Shibata, S. (2014). Chrono-biology, Chrono-pharmacology, and Chrono-nutrition. Journal of Pharmacological Sciences, 124(3), 320–335. http://doi.org/10.1254/jphs.13r06cr
Landolt, H.-P., Werth, E., Borbély, A. A., & Dijk, D.-J. (1995). Caffeine intake (200 mg) in the morning affects human sleep and EEG power spectra at night. Brain Research, 675(1-2), 67–74. http://doi.org/10.1016/0006-8993(95)00040-w
Gottesmann, C. (2002). GABA mechanisms and sleep. Neuroscience, 111(2), 231–239. http://doi.org/10.1016/s0306-4522(02)00034-9
Campbell, S. S., Dawson, D., & Anderson, M. W. (1993). Alleviation of Sleep Maintenance Insomnia with Timed Exposure to Bright Light. Journal of the American Geriatrics Society, 41(8), 829–836. http://doi.org/10.1111/j.1532-5415.1993.tb06179.x
Zhao, J., Tian, Y., Nie, J., Xu, J., & Liu, D. (2012). Red Light and the Sleep Quality and Endurance Performance of Chinese Female Basketball Players. Journal of Athletic Training, 47(6), 673–678. http://doi.org/10.4085/1062-6050-47.6.08
Smolensky, M. H., Sackett-Lundeen, L. L., & Portaluppi, F. (2015). Nocturnal light pollution and underexposure to daytime sunlight: Complementary mechanisms of circadian disruption and related diseases. Chronobiology International, 32(8), 1029–1048. http://doi.org/10.3109/07420528.2015.1072002
Düzgün, G., & Akyol, A. D. (2017). Effect of Natural Sunlight on Sleep Problems and Sleep Quality of the Elderly Staying in the Nursing Home. Holistic Nursing Practice, 31(5), 295–302. http://doi.org/10.1097/hnp.0000000000000206
Valham, F., Sahlin, C., Stenlund, H., & Franklin, K. A. (2012). Ambient Temperature and Obstructive Sleep Apnea: Effects on Sleep, Sleep Apnea, and Morning Alertness. Sleep, 35(4), 513–517. http://doi.org/10.5665/sleep.1736
Okamoto-Mizuno, K., Tsuzuki, K., & Mizuno, K. (2004). Effects of mild heat exposure on sleep stages and body temperature in older men. International Journal of Biometeorology, 49(1). http://doi.org/10.1007/s00484-004-0209-3
St-Onge, M.-P., & Shechter, A. (2014). Sleep disturbances, body fat distribution, food intake and/or energy expenditure: pathophysiological aspects. Hormone Molecular Biology and Clinical Investigation, 17(1). http://doi.org/10.1515/hmbci-2013-0066
Chaput, J.-P., Després, J.-P., Bouchard, C., & Tremblay, A. (2008). The Association Between Sleep Duration and Weight Gain in Adults: A 6-Year Prospective Study from the Quebec Family Study. Sleep, 31(4), 517–523. http://doi.org/10.1093/sleep/31.4.517
Dekker, S. A., Noordam, R., Biermasz, N. R., Roos, A., Lamb, H. J., Rosendaal, F. R., … Mutsert, R. (2018). Habitual Sleep Measures are Associated with Overall Body Fat, and not Specifically with Visceral Fat, in Men and Women. Obesity, 26(10), 1651–1658. http://doi.org/10.1002/oby.22289
Tunnicliffe, J. M., Erdman, K. A., Reimer, R. A., Lun, V., & Shearer, J. (2008). Consumption of dietary caffeine and coffee in physically active populations: physiological interactions. Applied Physiology, Nutrition, and Metabolism, 33(6), 1301–1310. http://doi.org/10.1139/h08-124
Mahoney, C. R., Giles, G. E., Marriott, B. P., Judelson, D. A., Glickman, E. L., Geiselman, P. J., & Lieberman, H. R. (2019). Intake of caffeine from all sources and reasons for use by college students. Clinical Nutrition, 38(2), 668–675. http://doi.org/10.1016/j.clnu.2018.04.004
Binks, H., Vincent, G. E., Gupta, C., Irwin, C., & Khalesi, S. (2020). Effects of Diet on Sleep: A Narrative Review. Nutrients, 12(4), 936. http://doi.org/10.3390/nu12040936
Rao, T. P., Ozeki, M., & Juneja, L. R. (2015). In Search of a Safe Natural Sleep Aid. Journal of the American College of Nutrition, 34(5), 436–447. http://doi.org/10.1080/07315724.2014.926153
Abbasi B, Kimiagar M, Sadeghniiat K, Shirazi MM, Hedayati M, Rashidkhani B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. J Res Med Sci. 2012 Dec;17(12):1161-9. https://pubmed.ncbi.nlm.nih.gov/23853635/
Aspy, D. J., Madden, N. A., & Delfabbro, P. (2018). Effects of Vitamin B6 (Pyridoxine) and a B Complex Preparation on Dreaming and Sleep. Perceptual and Motor Skills, 003151251877032. http://doi.org/10.1177/0031512518770326
Parazzini F. Resveratrol, tryptophanum, glycine and vitamin E: a nutraceutical approach to sleep disturbance and irritability in peri- and post-menopause. Minerva Ginecol. 2015;67(1):1-5. https://pubmed.ncbi.nlm.nih.gov/25660429/
Siegel JM. The neurotransmitters of sleep. J Clin Psychiatry. 2004;65 Suppl 16:4-7. https://pubmed.ncbi.nlm.nih.gov/15575797/
Djeridane, Y., Touitou, Y. Chronic diazepam administration differentially affects melatonin synthesis in rat pineal and Harderian glands. Psychopharmacology154, 403–407 (2001). https://doi.org/10.1007/s002130000631
Betti L, Palego L, Demontis GC, Miraglia F, Giannaccini G. Hydroxyindole-O-methyltransferase (HIOMT) activity in the retina of melatonin-proficient mice. Heliyon. 2019;5(9):e02417. Published 2019 Sep 14. doi:10.1016/j.heliyon.2019.e02417
Haduch, A., Bromek, E., Wójcikowski, J., Gołembiowska, K., Daniel, W.. Melatonin Supports Serotonin Formation by Brain CYP2D. Drug Metabolism and DispositionMarch 1, 2016, 44 (3) 445-452; DOI: https://doi.org/10.1124/dmd.115.067413
Morton, D. J. (1987). Mechanism of Inhibition of Bovine Pineal Gland Hydroxyindole-O-Methyltransferase (EC 2.1.1.4) by Divalent Cations. Journal of Pineal Research, 4(3), 295–303. http://doi.org/10.1111/j.1600-079x.1987.tb00867.x
Markova-Car, E. P., Jurišić, D., Ilić, N., & Pavelić, S. K. (2014). Running for time: circadian rhythms and melanoma. Tumor Biology, 35(9), 8359–8368. http://doi.org/10.1007/s13277-014-1904-2
Slominski AT, Zmijewski MA, Skobowiat C, Zbytek B, Slominski RM, Steketee JD. Sensing the environment: regulation of local and global homeostasis by the skin’s neuroendocrine system. Adv Anat Embryol Cell Biol. 2012;212:v-115. doi:10.1007/978-3-642-19683-6_1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3422784/
Chalupsky, K., Kračun, D., Kanchev, I., Bertram, K., & Görlach, A. (2015). Folic Acid Promotes Recycling of Tetrahydrobiopterin and Protects Against Hypoxia-Induced Pulmonary Hypertension by Recoupling Endothelial Nitric Oxide Synthase. Antioxidants & Redox Signaling, 23(14), 1076–1091. http://doi.org/10.1089/ars.2015.6329
Dianzani, I., Sanctis, L. D., Smooker, P. M., Gough, T. J., Alliaudi, C., Brusco, A., … Cotton, R. G. H. (1998). Dihydropteridine reductase deficiency: Physical structure of the QDPR gene, identification of two new mutations and genotype–phenotype correlations. Human Mutation, 12(4), 267–273. http://doi.org/10.1002/(sici)1098-1004(1998)12:4<267::aid-humu8>3.0.co;2-c
Nichol, C. A., Lee, C. L., Edelstein, M. P., Chao, J. Y., & Duch, D. S. (1983). Biosynthesis of tetrahydrobiopterin by de novo and salvage pathways in adrenal medulla extracts, mammalian cell cultures, and rat brain in vivo. Proceedings of the National Academy of Sciences, 80(6), 1546–1550. http://doi.org/10.1073/pnas.80.6.1546
Titus, F., Dávalos, A., Alom, J., & Codina, A. (1986). 5-Hydroxytryptophan versus Methysergide in the Prophylaxis of Migraine. European Neurology, 25(5), 327–329. http://doi.org/10.1159/000116030
Birdsall TC. 5-Hydroxytryptophan: a clinically-effective serotonin precursor. Altern Med Rev. 1998;3(4):271-280. https://pubmed.ncbi.nlm.nih.gov/9727088/
Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J. 2013;13(4):533-540. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865832/
Valadas, J. S., Esposito, G., Vandekerkhove, D., Miskiewicz, K., Deaulmerie, L., Raitano, S., … Verstreken, P. (2018). ER Lipid Defects in Neuropeptidergic Neurons Impair Sleep Patterns in Parkinson’s Disease. Neuron, 98(6). http://doi.org/10.1016/j.neuron.2018.05.022
Chung SY, Moriyama T, Uezu E, et al. Administration of phosphatidylcholine increases brain acetylcholine concentration and improves memory in mice with dementia. J Nutr. 1995;125(6):1484-1489. doi:10.1093/jn/125.6.1484 https://pubmed.ncbi.nlm.nih.gov/7782901/
Montgomery, P., Burton, J. R., Sewell, R. P., Spreckelsen, T. F., & Richardson, A. J. (2014). Fatty acids and sleep in UK children: subjective and pilot objective sleep results from the DOLAB study – a randomized controlled trial. Journal of Sleep Research, 23(4), 364–388. http://doi.org/10.1111/jsr.12135
Alzoubi, K. H., Mayyas, F., & Zamzam, H. I. A. (2019). Omega-3 fatty acids protects against chronic sleep-deprivation induced memory impairment. Life Sciences, 227, 1–7. http://doi.org/10.1016/j.lfs.2019.04.028
Nasehi, M., Mosavi-Nezhad, S.-M., Khakpai, F., & Zarrindast, M.-R. (2018). The role of omega-3 on modulation of cognitive deficiency induced by REM sleep deprivation in rats. Behavioural Brain Research, 351, 152–160. http://doi.org/10.1016/j.bbr.2018.06.002
Jahangard, L., Sadeghi, A., Ahmadpanah, M., Holsboer-Trachsler, E., Bahmani, D. S., Haghighi, M., & Brand, S. (2018). Influence of adjuvant omega-3-polyunsaturated fatty acids on depression, sleep, and emotion regulation among outpatients with major depressive disorders – Results from a double-blind, randomized and placebo-controlled clinical trial. Journal of Psychiatric Research, 107, 48–56. http://doi.org/10.1016/j.jpsychires.2018.09.016
Scorza, F. A., Cavalheiro, E. A., Scorza, C. A., Galduróz, J. C. F., Tufik, S., & Andersen, M. L. (2013). Sleep Apnea and Inflammation – Getting a Good Night’s Sleep with Omega-3 Supplementation. Frontiers in Neurology, 4. http://doi.org/10.3389/fneur.2013.00193
Hansen, A. L., Dahl, L., Olson, G., Thornton, D., Graff, I. E., Frøyland, L., … Pallesen, S. (2014). Fish Consumption, Sleep, Daily Functioning, and Heart Rate Variability. Journal of Clinical Sleep Medicine, 10(05), 567–575. http://doi.org/10.5664/jcsm.3714
Xie, L., Kang, H., Xu, Q., Chen, M. J., Liao, Y., Thiyagarajan, M., … Nedergaard, M. (2013). Sleep Drives Metabolite Clearance from the Adult Brain. Science, 342(6156), 373–377. http://doi.org/10.1126/science.1241224
Varshavsky, A. (2012). Augmented generation of protein fragments during wakefulness as the molecular cause of sleep: a hypothesis. Protein Science, 21(11), 1634–1661. http://doi.org/10.1002/pro.2148
Mackiewicz, M., Shockley, K. R., Romer, M. A., Galante, R. J., Zimmerman, J. E., Naidoo, N., … Pack, A. I. (2007). Macromolecule biosynthesis: a key function of sleep. Physiological Genomics, 31(3), 441–457. http://doi.org/10.1152/physiolgenomics.00275.2006
Scharf, M. T., Naidoo, N., Zimmerman, J. E., & Pack, A. I. (2008). The energy hypothesis of sleep revisited. Progress in Neurobiology, 86(3), 264–280. http://doi.org/10.1016/j.pneurobio.2008.08.003
Horne, J. (2009). REM sleep, energy balance and ‘optimal foraging.’ Neuroscience & Biobehavioral Reviews, 33(3), 466–474. http://doi.org/10.1016/j.neubiorev.2008.12.002
Berger, R. J., & Phillips, N. H. (1995). Energy conservation and sleep. Behavioural Brain Research, 69(1-2), 65–73. http://doi.org/10.1016/0166-4328(95)00002-b
Benington, J. H., & Heller, H. C. (1995). Restoration of brain energy metabolism as the function of sleep. Progress in Neurobiology, 45(4), 347–360. http://doi.org/10.1016/0301-0082(94)00057-o
Abel, T., Havekes, R., Saletin, J. M., & Walker, M. P. (2013). Sleep, Plasticity and Memory from Molecules to Whole-Brain Networks. Current Biology, 23(17). http://doi.org/10.1016/j.cub.2013.07.025
Rasch, B., & Born, J. (2013). About Sleeps Role in Memory. Physiological Reviews, 93(2), 681–766. http://doi.org/10.1152/physrev.00032.2012
Cirelli, C., & Tononi, G. (2008). Is Sleep Essential? PLoS Biology, 6(8). http://doi.org/10.1371/journal.pbio.0060216
Siegel, J. M. (2005). Clues to the functions of mammalian sleep. Nature, 437(7063), 1264–1271. http://doi.org/10.1038/nature04285
Campbell, S. S., & Tobler, I. (1984). Animal sleep: A review of sleep duration across phylogeny. Neuroscience & Biobehavioral Reviews, 8(3), 269–300. http://doi.org/10.1016/0149-7634(84)90054-x
Tobler, I. (1995). Is sleep fundamentally different between mammalian species? Behavioural Brain Research, 69(1-2), 35–41. http://doi.org/10.1016/0166-4328(95)00025-o
Tononi, G., & Cirelli, C. (2006). Sleep function and synaptic homeostasis. Sleep Medicine Reviews, 10(1), 49–62. http://doi.org/10.1016/j.smrv.2005.05.002
Dongen, H. P. A. V., Vitellaro, K. M., & Dinges, D. F. (2005). Individual Differences in Adult Human Sleep and Wakefulness: Leitmotif for a Research Agenda. Sleep, 28(4), 479–498. http://doi.org/10.1093/sleep/28.4.479
Vyazovskiy, V. V., & Delogu, A. (2014). NREM and REM Sleep. The Neuroscientist, 20(3), 203–219. http://doi.org/10.1177/1073858413518152
Mignot, E. (2008). Why We Sleep: The Temporal Organization of Recovery. PLoS Biology, 6(4). http://doi.org/10.1371/journal.pbio.0060106
Siegel, J. M. (2009). Sleep viewed as a state of adaptive inactivity. Nature Reviews Neuroscience, 10(10), 747–753. http://doi.org/10.1038/nrn2697
Horne, J. (2000). REM sleep — by default? Neuroscience & Biobehavioral Reviews, 24(8), 777–797. http://doi.org/10.1016/s0149-7634(00)00037-3
Baran, B., Pace-Schott, E. F., Ericson, C., & Spencer, R. M. C. (2012). Processing of Emotional Reactivity and Emotional Memory over Sleep. Journal of Neuroscience, 32(3), 1035–1042. http://doi.org/10.1523/jneurosci.2532-11.2012
Tononi, G., & Cirelli, C. (2014). Sleep and the Price of Plasticity: From Synaptic and Cellular Homeostasis to Memory Consolidation and Integration. Neuron, 81(1), 12–34. http://doi.org/10.1016/j.neuron.2013.12.025
Li, J., Vitiello, M. V., & Gooneratne, N. S. (2018). Sleep in Normal Aging. Sleep Medicine Clinics, 13(1), 1–11. http://doi.org/10.1016/j.jsmc.2017.09.001
Murillo-Rodriguez, E., Arias-Carrion, O., Zavala-Garcia, A., Sarro-Ramirez, A., & Huitron-Resendiz, S. (2012). Basic Sleep Mechanisms: An Integrative Review. Central Nervous System Agents in Medicinal Chemistry, 12(1), 38–54. http://doi.org/10.2174/187152412800229107
Weber, F. D. (2018). Sleep: Eye-Opener Highlights Sleep’s Organization. Current Biology, 28(5). http://doi.org/10.1016/j.cub.2018.01.054
Yetton, B. D., Mcdevitt, E. A., Cellini, N., Shelton, C., & Mednick, S. C. (2018). Quantifying sleep architecture dynamics and individual differences using big data and Bayesian networks. Plos One, 13(4). http://doi.org/10.1371/journal.pone.0194604
Colrain, I. M., Nicholas, C. L., & Baker, F. C. (2014). Alcohol and the sleeping brain. Handbook of Clinical Neurology Alcohol and the Nervous System, 415–431. http://doi.org/10.1016/b978-0-444-62619-6.00024-0
Zisapel, N. (2018). New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British Journal of Pharmacology, 175(16), 3190–3199. http://doi.org/10.1111/bph.14116
Tosini, G., Baba, K., Hwang, C. K., & Iuvone, P. M. (2012). Melatonin: An underappreciated player in retinal physiology and pathophysiology. Experimental Eye Research, 103, 82–89. http://doi.org/10.1016/j.exer.2012.08.009
Blasiak, J., Reiter, R. J., & Kaarniranta, K. (2016). Melatonin in Retinal Physiology and Pathology: The Case of Age-Related Macular Degeneration. Oxidative Medicine and Cellular Longevity, 2016, 1–12. http://doi.org/10.1155/2016/6819736
Bellingham, J., Chaurasia, S. S., Melyan, Z., Liu, C., Cameron, M. A., Tarttelin, E. E., … Lucas, R. J. (2006). Evolution of Melanopsin Photoreceptors: Discovery and Characterization of a New Melanopsin in Nonmammalian Vertebrates. PLoS Biology, 4(8). http://doi.org/10.1371/journal.pbio.0040254
Zaidi, F. H., Hull, J. T., Peirson, S. N., Wulff, K., Aeschbach, D., Gooley, J. J., … Lockley, S. W. (2007). Short-Wavelength Light Sensitivity of Circadian, Pupillary, and Visual Awareness in Humans Lacking an Outer Retina. Current Biology, 17(24), 2122–2128. http://doi.org/10.1016/j.cub.2007.11.034
Legates, T. A., Altimus, C. M., Wang, H., Lee, H.-K., Yang, S., Zhao, H., … Hattar, S. (2012). Aberrant light directly impairs mood and learning through melanopsin-expressing neurons. Nature, 491(7425), 594–598. http://doi.org/10.1038/nature11673
Sikka, G., Hussmann, G. P., Pandey, D., Cao, S., Hori, D., Park, J. T., … Berkowitz, D. E. (2014). Melanopsin mediates light-dependent relaxation in blood vessels. Proceedings of the National Academy of Sciences, 111(50), 17977–17982. http://doi.org/10.1073/pnas.1420258111
Buhr, E. D., Yoo, S.-H., & Takahashi, J. S. (2010). Temperature as a Universal Resetting Cue for Mammalian Circadian Oscillators. Science, 330(6002), 379–385. http://doi.org/10.1126/science.1195262
Robbins, R., Grandner, M. A., Buxton, O. M., Hale, L., Buysse, D. J., Knutson, K. L., … Jean-Louis, G. (2019). Sleep myths: an expert-led study to identify false beliefs about sleep that impinge upon population sleep health practices. Sleep Health, 5(4), 409–417. http://doi.org/10.1016/j.sleh.2019.02.002
Damiola, F. (2000). Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Genes & Development, 14(23), 2950–2961. http://doi.org/10.1101/gad.183500
Abel, T., Havekes, R., Saletin, J. M., & Walker, M. P. (2013). Sleep, Plasticity and Memory from Molecules to Whole-Brain Networks. Current Biology, 23(17). http://doi.org/10.1016/j.cub.2013.07.025
Muzet, A., Ehrhart, J., Candas, V., Libert, J. P., & Vogt, J. J. (1983). Rem Sleep and Ambient Temperature in Man. International Journal of Neuroscience, 18(1-2), 117–125. http://doi.org/10.3109/00207458308985885
Saini, C., Morf, J., Stratmann, M., Gos, P., & Schibler, U. (2012). Simulated body temperature rhythms reveal the phase-shifting behavior and plasticity of mammalian circadian oscillators. Genes & Development, 26(6), 567–580. http://doi.org/10.1101/gad.183251.111
Franco P, Szliwowski H, Dramaix M, Kahn A. Influence of ambient temperature on sleep characteristics and autonomic nervous control in healthy infants. Sleep. 2000 May 1;23(3):401-7. https://pubmed.ncbi.nlm.nih.gov/10811384/
Libert JP, Candas V, Muzet A, Ehrhart J. Thermoregulatory adjustments to thermal transients during slow wave sleep and REM sleep in man. J Physiol (Paris). 1982;78(3):251-7 https://pubmed.ncbi.nlm.nih.gov/7166740/
Palca, J. W., Walker, J. M., & Berger, R. J. (1986). Thermoregulation, metabolism, and stages of sleep in cold-exposed men. Journal of Applied Physiology, 61(3), 940–947. http://doi.org/10.1152/jappl.1986.61.3.940
Lack. (2009). Chronotype differences in circadian rhythms of temperature, melatonin, and sleepiness as measured in a modified constant routine protocol. Nature and Science of Sleep, 1. http://doi.org/10.2147/nss.s6234
Samson, D. R., Crittenden, A. N., Mabulla, I. A., Mabulla, A. Z. P., & Nunn, C. L. (2017). Chronotype variation drives night-time sentinel-like behaviour in hunter–gatherers. Proceedings of the Royal Society B: Biological Sciences, 284(1858), 20170967. http://doi.org/10.1098/rspb.2017.0967
Walker, R. J., Kribs, Z. D., Christopher, A. N., Shewach, O. R., & Wieth, M. B. (2014). Age, the Big Five, and time-of-day preference: A mediational model. Personality and Individual Differences, 56, 170–174. http://doi.org/10.1016/j.paid.2013.09.003
Bjorness, T., & Greene, R. (2009). Adenosine and Sleep. Current Neuropharmacology, 7(3), 238–245. http://doi.org/10.2174/157015909789152182
Dworak, M., Diel, P., Voss, S., Hollmann, W., & Strüder, H. (2007). Intense exercise increases adenosine concentrations in rat brain: Implications for a homeostatic sleep drive. Neuroscience, 150(4), 789–795. http://doi.org/10.1016/j.neuroscience.2007.09.062
Rainnie, D., Grunze, H., Mccarley, R., & Greene, R. (1994). Adenosine inhibition of mesopontine cholinergic neurons: implications for EEG arousal. Science, 263(5147), 689–692. http://doi.org/10.1126/science.8303279
Daly, J. W., Shi, D., Nikodijevic, O., & Jacobson, K. A. (1994). The role of adenosine receptors in the central action of caffeine. Pharmacopsychoecologia, 7(2), 201–213. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4373791/