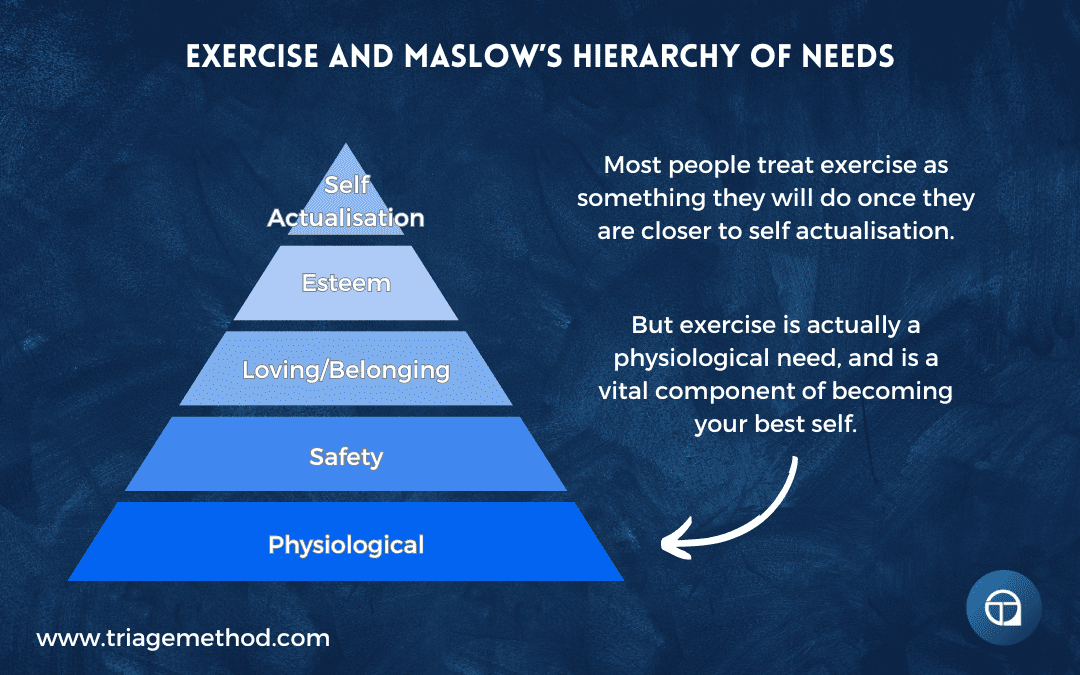
- Physiological Needs: At the foundational level, exercise directly addresses physiological needs such as health, vitality, and physical well-being. Engaging in exercise helps fulfil the body’s requirements for movement, energy expenditure, and maintenance of bodily functions.
- Safety Needs: Regular exercise contributes to personal safety by enhancing physical fitness, strength, and resilience. It reduces the risk of various health conditions, strengthens bones and muscles, and promotes overall well-being, thereby providing a sense of security and protection against illness and injury.
- Esteem Needs: Exercise can boost self-esteem and self-confidence by improving physical appearance, enhancing physical capabilities, and achieving personal fitness goals. Accomplishing milestones in exercise programs, such as lifting heavier weights or running longer distances, fosters feelings of competence and self-worth.
- Self-Actualisation: While physical exercise primarily addresses lower-level needs, it can also contribute to self-actualisation by providing opportunities for personal growth, self-expression, and fulfilment. Engaging in challenging workouts, pursuing athletic endeavours, or participating in sports can lead to experiences of flow, mastery, and peak performance, facilitating self-realisation and the fulfilment of one’s potential.
Table of Contents
- 1 Exercise And Health
- 2 Exercise and Nutrition
- 3 Exercise and Sleep
- 4 Stress
- 5 Why Is Exercise So Important
Exercise And Health
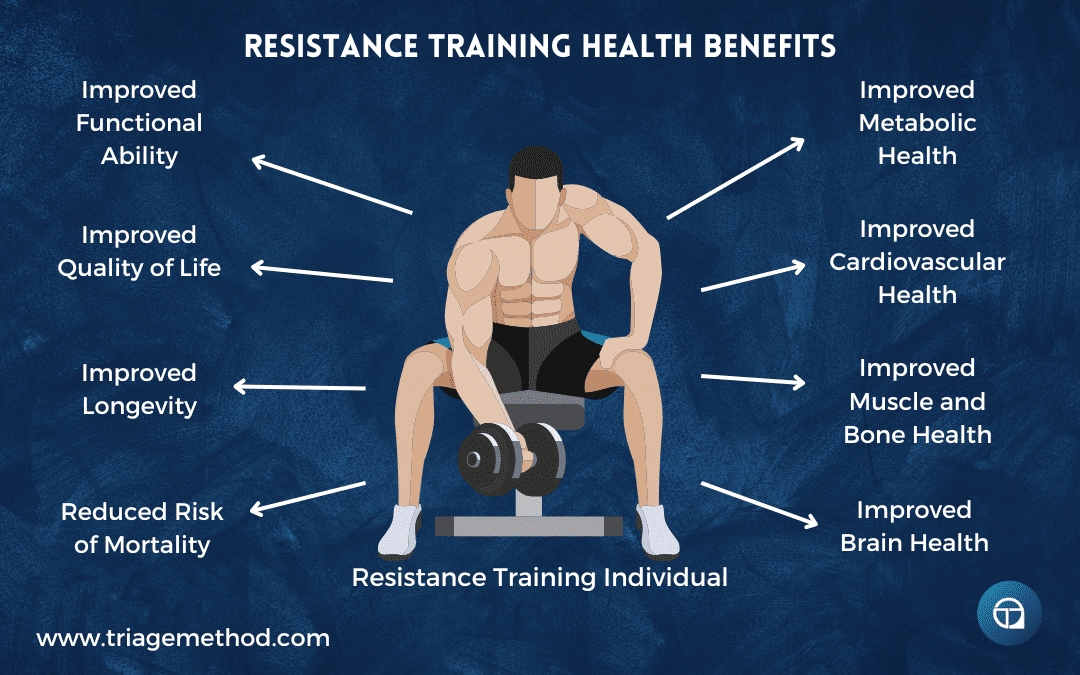
Resistance Training and Health
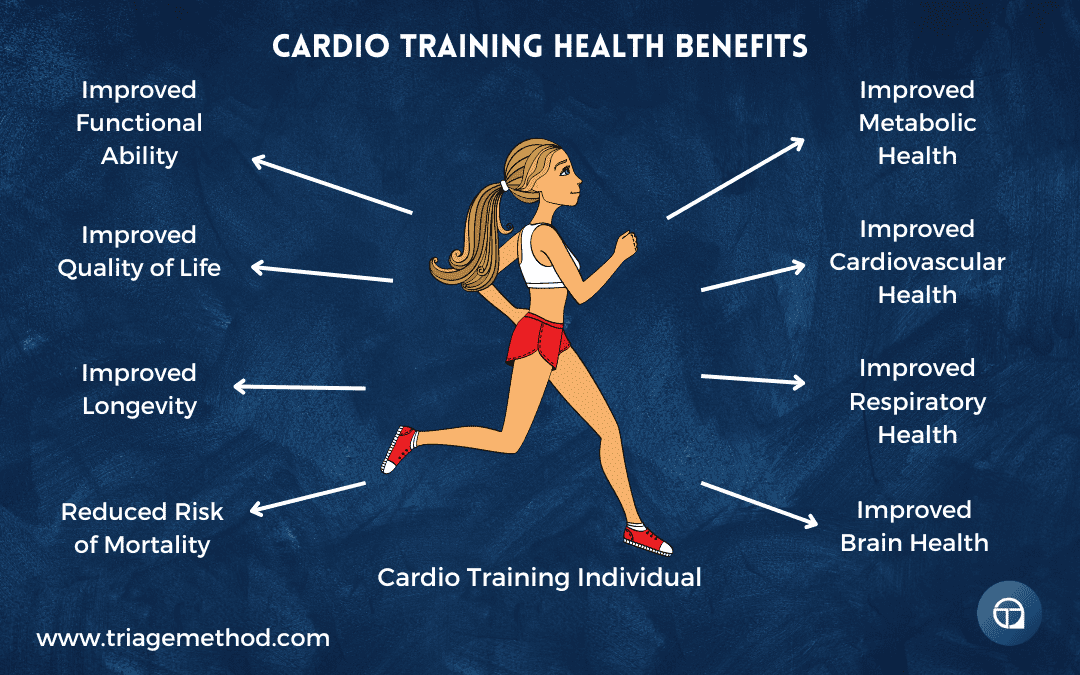
Cardiovascular Training and Health
Exercise and Health More Broadly
Exercise and Metabolic Health and Disease
Musculoskeletal Health and Disease
Cardiovascular Health and Disease
Respiratory Health and Disease
Immune System Health and Disease
Cancer
Hormonal Health and Fertility
Cognitive Health
Mental Health
Exercise and Quantity of Life
Exercise and Quality of Life
Health In The Non-Exercising Individual
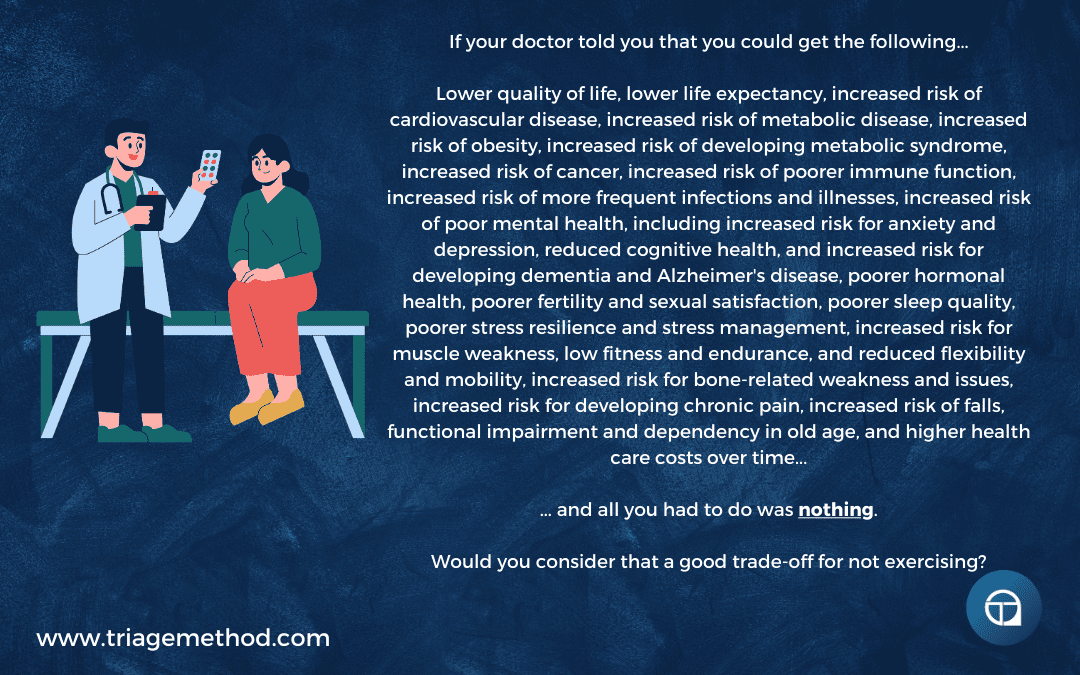
Pascal’s Exercise Wager
Exercise and Nutrition
How Exercise Affects The Diet
How The Diet Affects Exercise
Exercise and Sleep
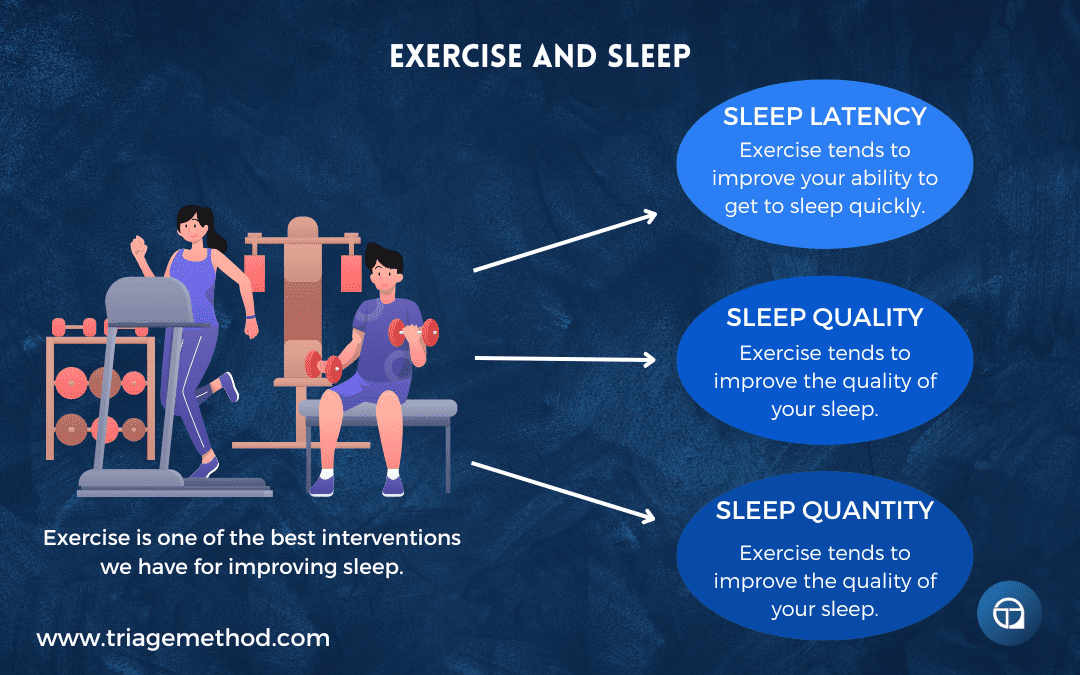
Exercise and Sleep
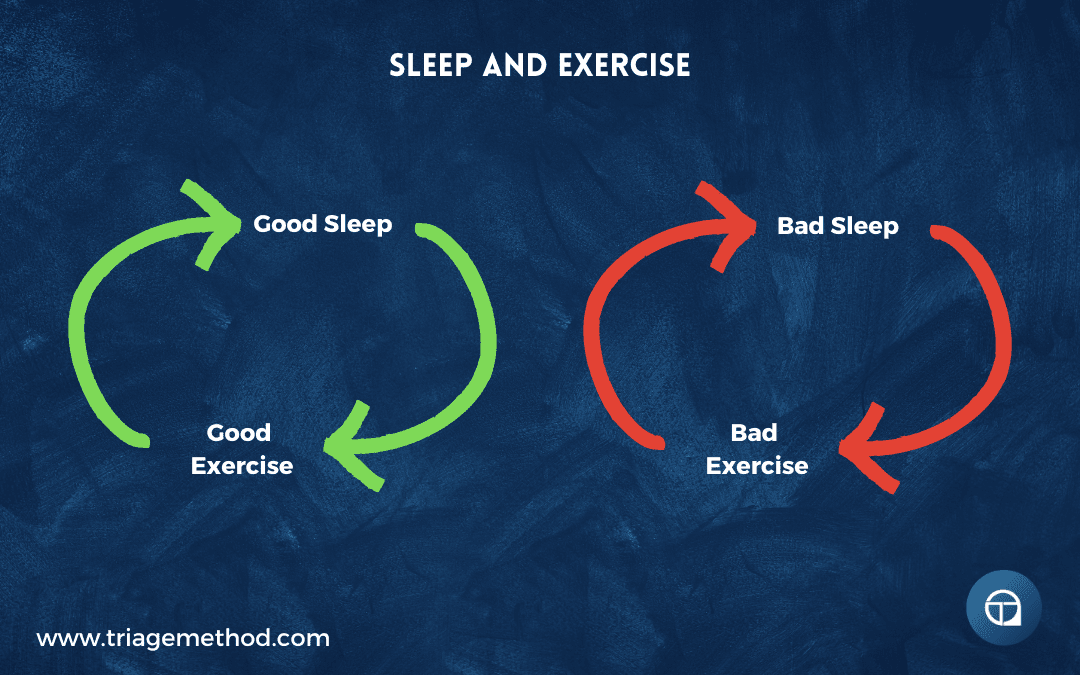
Sleep and Exercise
Stress
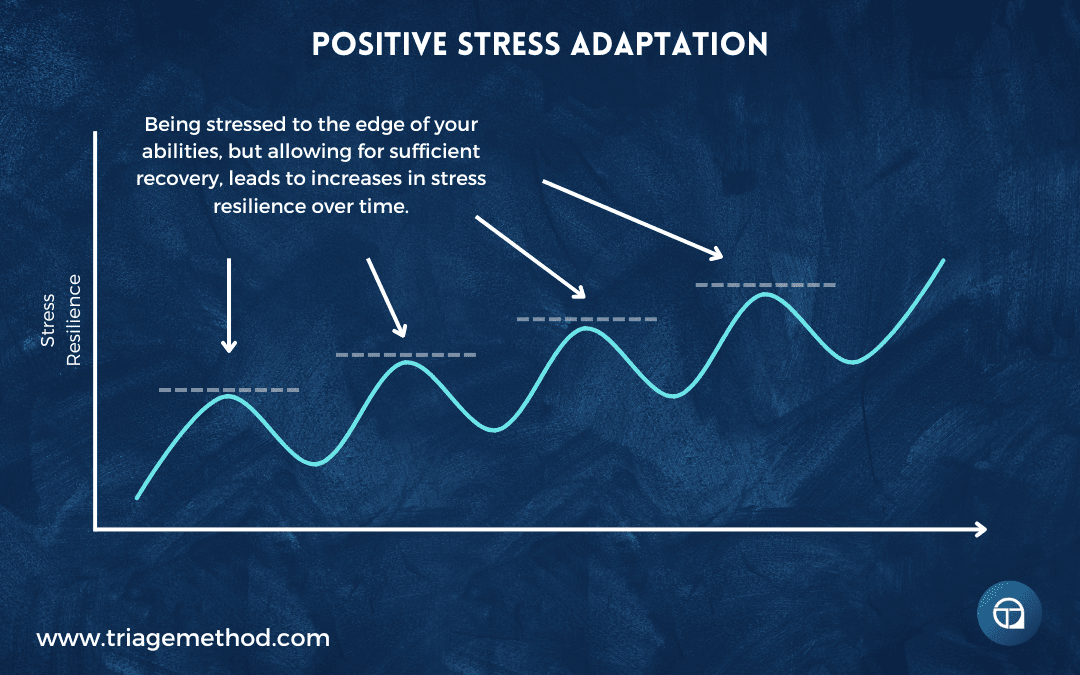
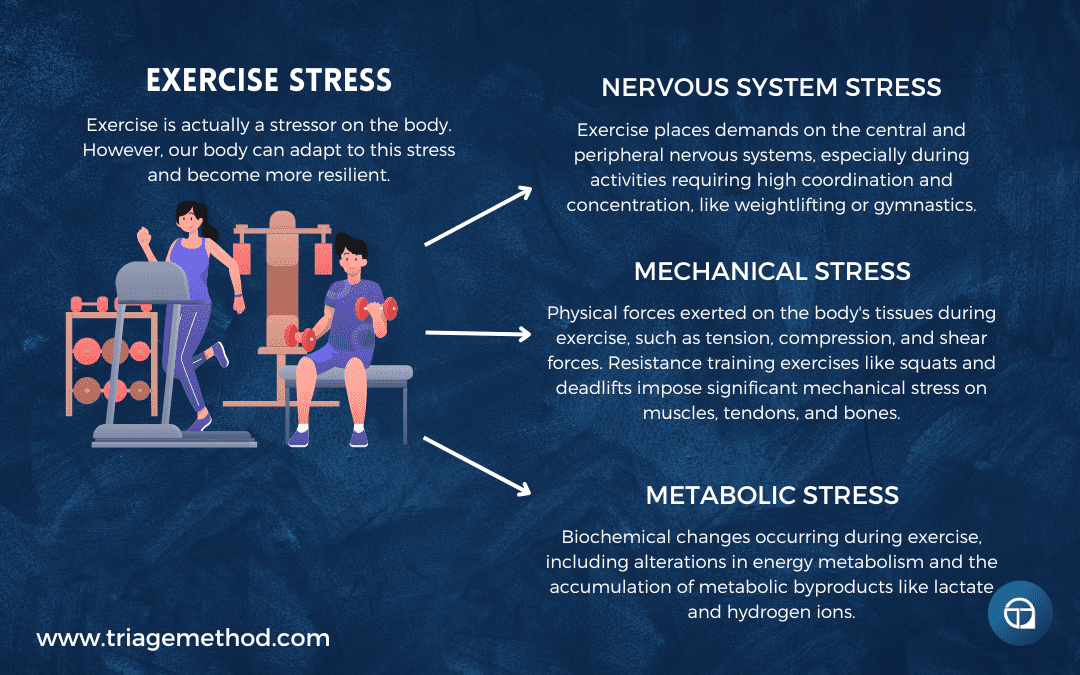
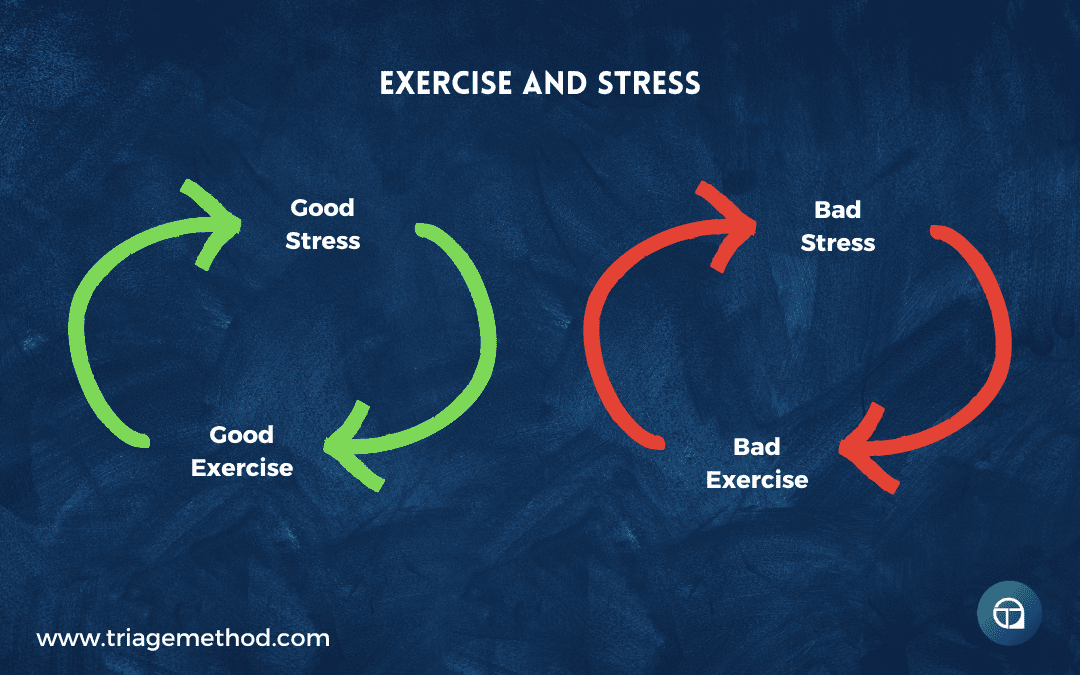
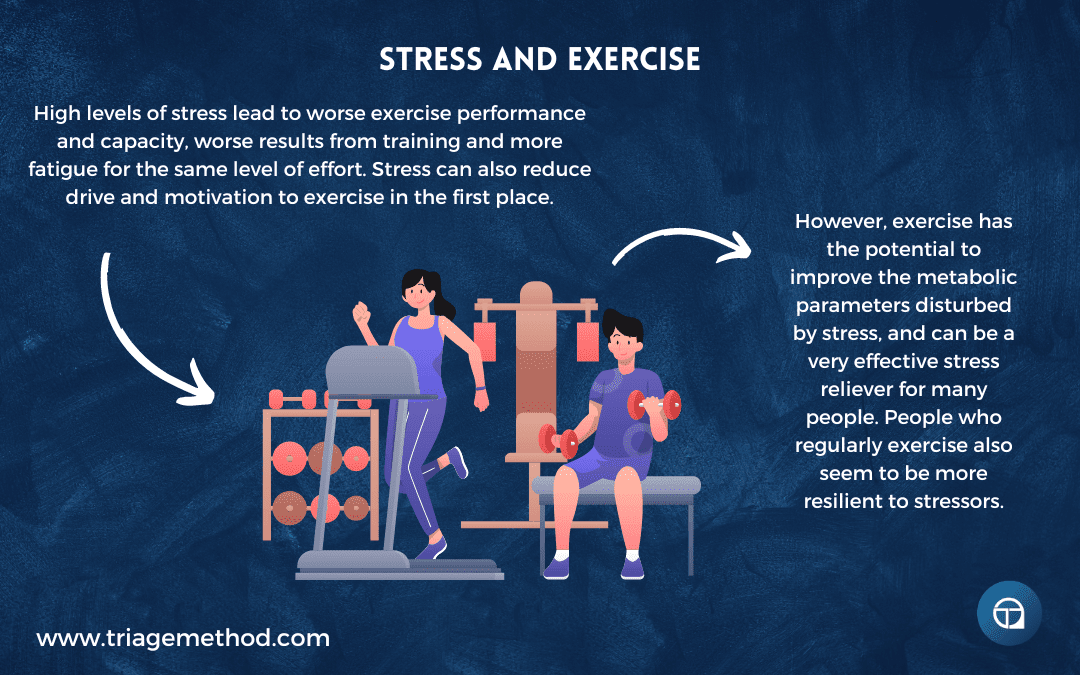
Exercise and Stress
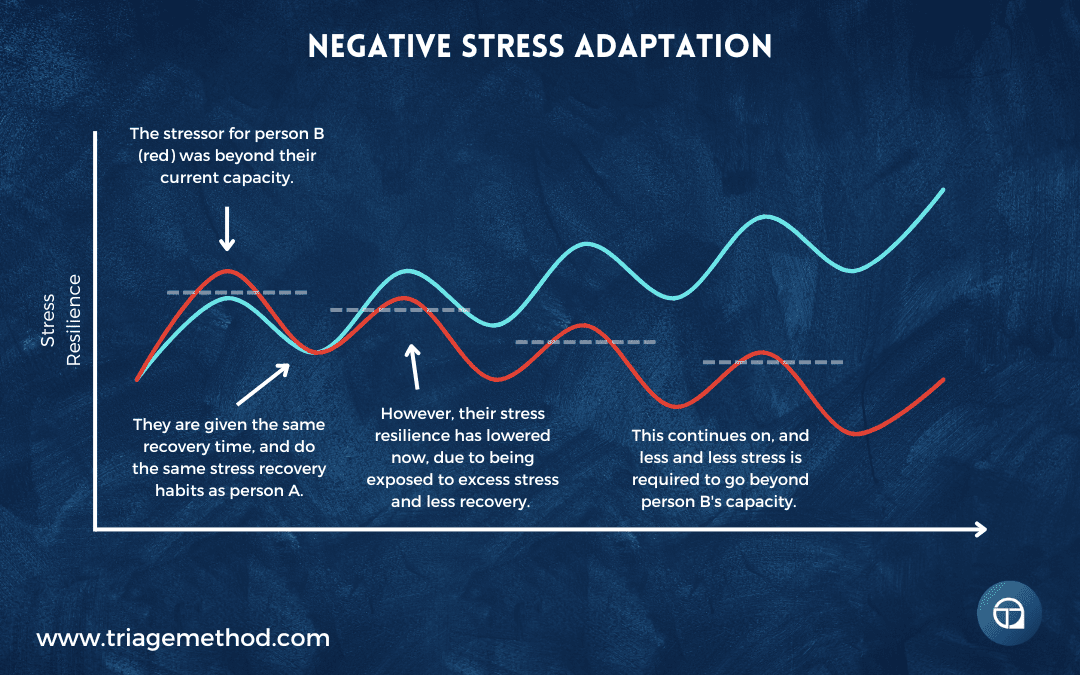
Stress and Exercise
Why Is Exercise So Important
Hopefully, you can now see just why exercise is so important. It really is one of the pillars of health. Unfortunately, it is also the pillar of health that gets neglected the most. However, those who do exercise are rewarded generously for their efforts. So it is a good idea to optimise your exercise programming. You can do this by reaching out to us and getting online coaching, or alternatively, by interacting with our free content. It would be especially helpful if you understood the goals of exercise, as that will really help you to create a more effective exercise program for your needs. If you want more free information on exercise, you can follow us on Instagram, YouTube or listen to the podcast, where we discuss all the little intricacies of exercise. You can always stay up to date with our latest content by subscribing to our newsletter. Finally, if you want to learn how to coach nutrition, then consider our Nutrition Coach Certification course. If you don’t understand something, or you just need clarification, you can always reach out to us on Instagram or via email.
References and Further Reading
Ruegsegger GN, Booth FW. Health Benefits of Exercise. Cold Spring Harb Perspect Med. 2018;8(7):a029694. Published 2018 Jul 2. doi:10.1101/cshperspect.a029694 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6027933/
Posadzki P, Pieper D, Bajpai R, et al. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health. 2020;20(1):1724. Published 2020 Nov 16. doi:10.1186/s12889-020-09855-3 https://pubmed.ncbi.nlm.nih.gov/33198717/
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541-556. doi:10.1097/HCO.0000000000000437 https://pubmed.ncbi.nlm.nih.gov/28708630/
Kramer A. An Overview of the Beneficial Effects of Exercise on Health and Performance. Adv Exp Med Biol. 2020;1228:3-22. doi:10.1007/978-981-15-1792-1_1 https://pubmed.ncbi.nlm.nih.gov/32342447/
Qiu Y, Fernández-García B, Lehmann HI, et al. Exercise sustains the hallmarks of health. J Sport Health Sci. 2023;12(1):8-35. doi:10.1016/j.jshs.2022.10.003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9923435/
Thompson WR, Sallis R, Joy E, Jaworski CA, Stuhr RM, Trilk JL. Exercise Is Medicine. Am J Lifestyle Med. 2020;14(5):511-523. Published 2020 Apr 22. doi:10.1177/1559827620912192 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7444006/
Pinckard K, Baskin KK, Stanford KI. Effects of Exercise to Improve Cardiovascular Health. Front Cardiovasc Med. 2019;6:69. Published 2019 Jun 4. doi:10.3389/fcvm.2019.00069 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6557987/
Nystoriak MA, Bhatnagar A. Cardiovascular Effects and Benefits of Exercise. Front Cardiovasc Med. 2018;5:135. Published 2018 Sep 28. doi:10.3389/fcvm.2018.00135 https://pubmed.ncbi.nlm.nih.gov/30324108/
Chen H, Chen C, Spanos M, et al. Exercise training maintains cardiovascular health: signaling pathways involved and potential therapeutics. Signal Transduct Target Ther. 2022;7(1):306. Published 2022 Sep 1. doi:10.1038/s41392-022-01153-1 https://pubmed.ncbi.nlm.nih.gov/36050310/
Valenzuela PL, Ruilope LM, Santos-Lozano A, et al. Exercise benefits in cardiovascular diseases: from mechanisms to clinical implementation. Eur Heart J. 2023;44(21):1874-1889. doi:10.1093/eurheartj/ehad170 https://pubmed.ncbi.nlm.nih.gov/37005351/
Fiuza-Luces C, Santos-Lozano A, Joyner M, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018;15(12):731-743. doi:10.1038/s41569-018-0065-1 https://pubmed.ncbi.nlm.nih.gov/30115967/
Isath A, Koziol KJ, Martinez MW, et al. Exercise and cardiovascular health: A state-of-the-art review. Prog Cardiovasc Dis. 2023;79:44-52. doi:10.1016/j.pcad.2023.04.008 https://pubmed.ncbi.nlm.nih.gov/37120119/
Buzzachera, C.F., Correale, L., Liberali, G. (2020). Physical Activity and Cardiovascular Health. In: Govoni, S., Politi, P., Vanoli, E. (eds) Brain and Heart Dynamics. Springer, Cham. https://doi.org/10.1007/978-3-319-90305-7_59-1
Gronek P, Wielinski D, Cyganski P, et al. A Review of Exercise as Medicine in Cardiovascular Disease: Pathology and Mechanism. Aging Dis. 2020;11(2):327-340. Published 2020 Mar 9. doi:10.14336/AD.2019.0516 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7069454/
Thyfault JP, Bergouignan A. Exercise and metabolic health: beyond skeletal muscle. Diabetologia. 2020;63(8):1464-1474. doi:10.1007/s00125-020-05177-6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7377236/
McGee SL, Hargreaves M. Exercise adaptations: molecular mechanisms and potential targets for therapeutic benefit. Nat Rev Endocrinol. 2020;16(9):495-505. doi:10.1038/s41574-020-0377-1 https://pubmed.ncbi.nlm.nih.gov/32632275/
Goodpaster BH, Sparks LM. Metabolic Flexibility in Health and Disease. Cell Metab. 2017;25(5):1027-1036. doi:10.1016/j.cmet.2017.04.015 https://pubmed.ncbi.nlm.nih.gov/28467922/
Liu, S., Niu, Y. & Fu, L. Metabolic Adaptations to Exercise Training. J. of SCI. IN SPORT AND EXERCISE 2, 1–6 (2020). https://doi.org/10.1007/s42978-019-0018-3
Philippou, A., Chryssanthopoulos, C., Maridaki, M., Dimitriadis, G., Koutsilieris, M. (2019). Exercise Metabolism in Health and Disease. In: Kokkinos, P., Narayan, P. (eds) Cardiorespiratory Fitness in Cardiometabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-04816-7_5
Hsu KJ, Liao CD, Tsai MW, Chen CN. Effects of Exercise and Nutritional Intervention on Body Composition, Metabolic Health, and Physical Performance in Adults with Sarcopenic Obesity: A Meta-Analysis. Nutrients. 2019;11(9):2163. Published 2019 Sep 9. doi:10.3390/nu11092163 https://pubmed.ncbi.nlm.nih.gov/31505890/
Richter EA, Sylow L, Hargreaves M. Interactions between insulin and exercise. Biochem J. 2021;478(21):3827-3846. doi:10.1042/BCJ20210185 https://pubmed.ncbi.nlm.nih.gov/34751700/
Way KL, Hackett DA, Baker MK, Johnson NA. The Effect of Regular Exercise on Insulin Sensitivity in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Diabetes Metab J. 2016;40(4):253-271. doi:10.4093/dmj.2016.40.4.253 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4995180/
Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2017;2(1):e000143. Published 2017 Mar 1. doi:10.1136/bmjsem-2016-000143 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569266/
Borhade MB, Singh S. Diabetes and Exercise. [Updated 2022 Sep 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.https://www.ncbi.nlm.nih.gov/books/NBK526095/
Harrington, D. and Henson, J. (2021), Physical activity and exercise in the management of type 2 diabetes: where to start?. Pract Diab, 38: 35-40b. https://wchh.onlinelibrary.wiley.com/doi/full/10.1002/pdi.2361
U.S. Afsheen Syeda, Daniel Battillo, Aayush Visaria, Steven K. Malin, The importance of exercise for glycemic control in type 2 diabetes, American Journal of Medicine Open, Volume 9, 2023, 100031, ISSN 2667-0364, https://doi.org/10.1016/j.ajmo.2023.100031.
Collins KA, Ross LM, Slentz CA, Huffman KM, Kraus WE. Differential Effects of Amount, Intensity, and Mode of Exercise Training on Insulin Sensitivity and Glucose Homeostasis: A Narrative Review. Sports Med Open. 2022;8(1):90. Published 2022 Jul 14. https://pubmed.ncbi.nlm.nih.gov/35834023/
Borghouts LB, Keizer HA. Exercise and insulin sensitivity: a review. Int J Sports Med. 2000;21(1):1-12. doi:10.1055/s-2000-8847 https://pubmed.ncbi.nlm.nih.gov/10683091/
Keating SE, Hackett DA, George J, Johnson NA. Exercise and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol. 2012;57(1):157-166. doi:10.1016/j.jhep.2012.02.023 https://pubmed.ncbi.nlm.nih.gov/22414768/
Xue Y, Peng Y, Zhang L, Ba Y, Jin G, Liu G. Effect of different exercise modalities on nonalcoholic fatty liver disease: a systematic review and network meta-analysis. Sci Rep. 2024;14(1):6212. Published 2024 Mar 14. doi:10.1038/s41598-024-51470-4 https://pubmed.ncbi.nlm.nih.gov/38485714/
Farzanegi P, Dana A, Ebrahimpoor Z, Asadi M, Azarbayjani MA. Mechanisms of beneficial effects of exercise training on non-alcoholic fatty liver disease (NAFLD): Roles of oxidative stress and inflammation. Eur J Sport Sci. 2019;19(7):994-1003. doi:10.1080/17461391.2019.1571114 https://pubmed.ncbi.nlm.nih.gov/30732555/
Patten RK, Boyle RA, Moholdt T, et al. Exercise Interventions in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Physiol. 2020;11:606. Published 2020 Jul 7. doi:10.3389/fphys.2020.00606 https://pubmed.ncbi.nlm.nih.gov/32733258/
Harrison CL, Lombard CB, Moran LJ, Teede HJ. Exercise therapy in polycystic ovary syndrome: a systematic review. Hum Reprod Update. 2011;17(2):171-183. doi:10.1093/humupd/dmq045 https://pubmed.ncbi.nlm.nih.gov/20833639/
Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ Res. 2019;124(5):799-815. doi:10.1161/CIRCRESAHA.118.312669 https://pubmed.ncbi.nlm.nih.gov/30817262/
Ghodeshwar GK, Dube A, Khobragade D. Impact of Lifestyle Modifications on Cardiovascular Health: A Narrative Review. Cureus. 2023;15(7):e42616. Published 2023 Jul 28. doi:10.7759/cureus.42616 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10460604/
Tian D, Meng J. Exercise for Prevention and Relief of Cardiovascular Disease: Prognoses, Mechanisms, and Approaches. Oxid Med Cell Longev. 2019;2019:3756750. Published 2019 Apr 9. doi:10.1155/2019/3756750 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6481017/
Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789-795. doi:10.1161/CIRCULATIONAHA.110.010710 https://pubmed.ncbi.nlm.nih.gov/21810663/
Carpio-Rivera E, Moncada-Jiménez J, Salazar-Rojas W, Solera-Herrera A. Acute Effects of Exercise on Blood Pressure: A Meta-Analytic Investigation. Arq Bras Cardiol. 2016;106(5):422-433. doi:10.5935/abc.20160064 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914008/
Alpsoy Ş. Exercise and Hypertension. Adv Exp Med Biol. 2020;1228:153-167. doi:10.1007/978-981-15-1792-1_10 https://pubmed.ncbi.nlm.nih.gov/32342456/
Lopes S, Mesquita-Bastos J, Alves AJ, Ribeiro F. Exercise as a tool for hypertension and resistant hypertension management: current insights. Integr Blood Press Control. 2018;11:65-71. Published 2018 Sep 20. doi:10.2147/IBPC.S136028 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6159802/
Börjesson M, Onerup A, Lundqvist S, Dahlöf B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016;50(6):356-361. doi:10.1136/bjsports-2015-095786 https://pubmed.ncbi.nlm.nih.gov/26787705/
Cox CE. Role of Physical Activity for Weight Loss and Weight Maintenance. Diabetes Spectr. 2017;30(3):157-160. doi:10.2337/ds17-0013 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5556592/
Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441-447. doi:10.1016/j.pcad.2013.09.012 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3925973/
Bellicha A, van Baak MA, Battista F, et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: An overview of 12 systematic reviews and 149 studies. Obes Rev. 2021;22 Suppl 4(Suppl 4):e13256. doi:10.1111/obr.13256 https://pubmed.ncbi.nlm.nih.gov/33955140/
Rijal A, Adhikari TB, Dhakal S, et al. Effect of exercise on functional capacity and body weight for people with hypertension, type 2 diabetes, or cardiovascular disease: a systematic review with meta-analysis and trial sequential analysis. BMC Sports Sci Med Rehabil. 2024;16(1):38. Published 2024 Feb 7. doi:10.1186/s13102-024-00829-1 https://pubmed.ncbi.nlm.nih.gov/38321506/
Wiklund P. The role of physical activity and exercise in obesity and weight management: Time for critical appraisal. J Sport Health Sci. 2016;5(2):151-154. doi:10.1016/j.jshs.2016.04.001 https://pubmed.ncbi.nlm.nih.gov/30356545/
King NA, Horner K, Hills AP, et al. Exercise, appetite and weight management: understanding the compensatory responses in eating behaviour and how they contribute to variability in exercise-induced weight loss. Br J Sports Med. 2012;46(5):315-322. doi:10.1136/bjsm.2010.082495 https://pubmed.ncbi.nlm.nih.gov/21596715/
Metsios GS, Moe RH, Kitas GD. Exercise and inflammation. Best Pract Res Clin Rheumatol. 2020;34(2):101504. doi:10.1016/j.berh.2020.101504 https://pubmed.ncbi.nlm.nih.gov/32249021/
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607-615. Published 2011 Aug 5. doi:10.1038/nri3041 https://pubmed.ncbi.nlm.nih.gov/21818123/
Woods JA, Wilund KR, Martin SA, Kistler BM. Exercise, inflammation and aging. Aging Dis. 2012;3(1):130-140. https://pubmed.ncbi.nlm.nih.gov/22500274/
Cerqueira É, Marinho DA, Neiva HP, Lourenço O. Inflammatory Effects of High and Moderate Intensity Exercise-A Systematic Review. Front Physiol. 2020;10:1550. Published 2020 Jan 9. doi:10.3389/fphys.2019.01550 https://pubmed.ncbi.nlm.nih.gov/31992987/
Clarke J. Exercise exerts anti-inflammatory effects on muscle via the JAK-STAT pathway. Nat Rev Rheumatol. 2021;17(3):127. doi:10.1038/s41584-021-00581-7 https://pubmed.ncbi.nlm.nih.gov/33558742/
Peake JM, Neubauer O, Della Gatta PA, Nosaka K. Muscle damage and inflammation during recovery from exercise. J Appl Physiol (1985). 2017;122(3):559-570. doi:10.1152/japplphysiol.00971.2016 https://pubmed.ncbi.nlm.nih.gov/28035017/
Ballantyne CM, Davis JW. Exercise and Mortality in Heart Disease Cohorts: Meta-Analysis to Augment Available Evidence. J Am Coll Cardiol. 2022;79(17):1701-1703. doi:10.1016/j.jacc.2022.02.037 https://pubmed.ncbi.nlm.nih.gov/35483758/
Cattadori G, Segurini C, Picozzi A, Padeletti L, Anzà C. Exercise and heart failure: an update. ESC Heart Fail. 2018;5(2):222-232. doi:10.1002/ehf2.12225 https://pubmed.ncbi.nlm.nih.gov/29235244/
Edwards J, Shanmugam N, Ray R, et al. Exercise Mode in Heart Failure: A Systematic Review and Meta-Analysis. Sports Med Open. 2023;9(1):3. Published 2023 Jan 9. doi:10.1186/s40798-022-00549-1 https://pubmed.ncbi.nlm.nih.gov/36622511/
Aune D, Schlesinger S, Leitzmann MF, et al. Physical activity and the risk of heart failure: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2021;36(4):367-381. doi:10.1007/s10654-020-00693-6 https://pubmed.ncbi.nlm.nih.gov/33331992/
Alvarez P, Hannawi B, Guha A. Exercise And Heart Failure: Advancing Knowledge And Improving Care. Methodist Debakey Cardiovasc J. 2016;12(2):110-115. doi:10.14797/mdcj-12-2-110 https://pubmed.ncbi.nlm.nih.gov/27486494/
Nijholt KT, Sánchez-Aguilera PI, Voorrips SN, de Boer RA, Westenbrink BD. Exercise: a molecular tool to boost muscle growth and mitochondrial performance in heart failure?. Eur J Heart Fail. 2022;24(2):287-298. doi:10.1002/ejhf.2407 https://pubmed.ncbi.nlm.nih.gov/34957643/
Nayor M, Vasan RS. Preventing heart failure: the role of physical activity. Curr Opin Cardiol. 2015;30(5):543-550. doi:10.1097/HCO.0000000000000206 https://pubmed.ncbi.nlm.nih.gov/26154074/
Han P, Zhang W, Kang L, et al. Clinical Evidence of Exercise Benefits for Stroke. Adv Exp Med Biol. 2017;1000:131-151. doi:10.1007/978-981-10-4304-8_9 https://pubmed.ncbi.nlm.nih.gov/29098620/
García-Cabo C, López-Cancio E. Exercise and Stroke. Adv Exp Med Biol. 2020;1228:195-203. doi:10.1007/978-981-15-1792-1_13 https://pubmed.ncbi.nlm.nih.gov/32342459/
Prior PL, Suskin N. Exercise for stroke prevention. Stroke Vasc Neurol. 2018;3(2):59-68. Published 2018 Jun 26. doi:10.1136/svn-2018-000155 https://pubmed.ncbi.nlm.nih.gov/30191075/
Hou L, Li M, Wang J, et al. Association between physical exercise and stroke recurrence among first-ever ischemic stroke survivors. Sci Rep. 2021;11(1):13372. Published 2021 Jun 28. doi:10.1038/s41598-021-92736-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8238988/
Edward JA, Cornwell WK 3rd. Impact of Exercise on Cerebrovascular Physiology and Risk of Stroke. Stroke. 2022;53(7):2404-2410. doi:10.1161/STROKEAHA.121.037343 https://pubmed.ncbi.nlm.nih.gov/35506387/
Kramer SF, Hung SH, Brodtmann A. The Impact of Physical Activity Before and After Stroke on Stroke Risk and Recovery: a Narrative Review. Curr Neurol Neurosci Rep. 2019;19(6):28. Published 2019 Apr 22. doi:10.1007/s11910-019-0949-4 https://pubmed.ncbi.nlm.nih.gov/31011851/
Ali A, Tabassum D, Baig SS, et al. Effect of Exercise Interventions on Health-Related Quality of Life After Stroke and Transient Ischemic Attack: A Systematic Review and Meta-Analysis. Stroke. 2021;52(7):2445-2455. doi:10.1161/STROKEAHA.120.032979 https://pubmed.ncbi.nlm.nih.gov/34039033/
Akyuz A. Exercise and Coronary Heart Disease. Adv Exp Med Biol. 2020;1228:169-179. doi:10.1007/978-981-15-1792-1_11 https://pubmed.ncbi.nlm.nih.gov/32342457/
Aengevaeren VL, Mosterd A, Sharma S, et al. Exercise and Coronary Atherosclerosis: Observations, Explanations, Relevance, and Clinical Management. Circulation. 2020;141(16):1338-1350. doi:10.1161/CIRCULATIONAHA.119.044467 https://pubmed.ncbi.nlm.nih.gov/32310695/
Winzer EB, Woitek F, Linke A. Physical Activity in the Prevention and Treatment of Coronary Artery Disease. J Am Heart Assoc. 2018;7(4):e007725. Published 2018 Feb 8. doi:10.1161/JAHA.117.007725 https://pubmed.ncbi.nlm.nih.gov/29437600/
Hambrecht R, Wolf A, Gielen S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342(7):454-460. doi:10.1056/NEJM200002173420702 https://pubmed.ncbi.nlm.nih.gov/10675425/
Moreira JBN, Wohlwend M, Wisløff U. Exercise and cardiac health: physiological and molecular insights. Nat Metab. 2020;2(9):829-839. doi:10.1038/s42255-020-0262-1 https://pubmed.ncbi.nlm.nih.gov/32807982/
Gerbild H, Larsen CM, Graugaard C, Areskoug Josefsson K. Physical Activity to Improve Erectile Function: A Systematic Review of Intervention Studies. Sex Med. 2018;6(2):75-89. doi:10.1016/j.esxm.2018.02.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5960035/
Duca Y, Calogero AE, Cannarella R, et al. Erectile dysfunction, physical activity and physical exercise: Recommendations for clinical practice. Andrologia. 2019;51(5):e13264. doi:10.1111/and.13264 https://pubmed.ncbi.nlm.nih.gov/30873650/
Khera M, Bhattacharyya S, Miller LE. Effect of aerobic exercise on erectile function: systematic review and meta-analysis of randomized controlled trials. J Sex Med. 2023;20(12):1369-1375. doi:10.1093/jsxmed/qdad130 https://pubmed.ncbi.nlm.nih.gov/37814532/
Kałka D, Domagała Z, Dworak J, et al. Association between physical exercise and quality of erection in men with ischaemic heart disease and erectile dysfunction subjected to physical training. Kardiol Pol. 2013;71(6):573-580. doi:10.5603/KP.2013.0120 https://pubmed.ncbi.nlm.nih.gov/23797429/
Allen MS. Physical activity as an adjunct treatment for erectile dysfunction. Nat Rev Urol. 2019;16(9):553-562. doi:10.1038/s41585-019-0210-6 https://pubmed.ncbi.nlm.nih.gov/31239541/
Xiong T, Bai X, Wei X, et al. Exercise Rehabilitation and Chronic Respiratory Diseases: Effects, Mechanisms, and Therapeutic Benefits. Int J Chron Obstruct Pulmon Dis. 2023;18:1251-1266. Published 2023 Jun 19. doi:10.2147/COPD.S408325 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10289097/
Price OJ, Simpson AJ. Exercise and asthma – trigger or treatment?. Respir Med. 2023;213:107247. doi:10.1016/j.rmed.2023.107247 https://pubmed.ncbi.nlm.nih.gov/37086818/
Wu X, Gao S, Lian Y. Effects of continuous aerobic exercise on lung function and quality of life with asthma: a systematic review and meta-analysis. J Thorac Dis. 2020;12(9):4781-4795. doi:10.21037/jtd-19-2813 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7578506/
Romer LM. Respiratory influences on oxygen transport and exercise performance in health and disease. Exp Physiol. 2020;105(12):1977-1978. doi:10.1113/EP089199 https://pubmed.ncbi.nlm.nih.gov/33372725/
Xiang X, Huang L, Fang Y, Cai S, Zhang M. Physical activity and chronic obstructive pulmonary disease: a scoping review. BMC Pulm Med. 2022;22(1):301. Published 2022 Aug 5. doi:10.1186/s12890-022-02099-4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9354440/
Shu CC, Lee JH, Tsai MK, Su TC, Wen CP. The ability of physical activity in reducing mortality risks and cardiovascular loading and in extending life expectancy in patients with COPD. Sci Rep. 2021;11(1):21674. Published 2021 Nov 4. doi:10.1038/s41598-021-00728-2 https://pubmed.ncbi.nlm.nih.gov/34737308/
Kuder MM, Clark M, Cooley C, et al. A Systematic Review of the Effect of Physical Activity on Asthma Outcomes. J Allergy Clin Immunol Pract. 2021;9(9):3407-3421.e8. doi:10.1016/j.jaip.2021.04.048 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8434961/
Nieman DC, Sakaguchi CA. Physical activity lowers the risk for acute respiratory infections: Time for recognition. J Sport Health Sci. 2022;11(6):648-655. doi:10.1016/j.jshs.2022.08.002 https://pubmed.ncbi.nlm.nih.gov/35995362/
Wang J, Liu S, Li G, Xiao J. Exercise Regulates the Immune System. Adv Exp Med Biol. 2020;1228:395-408. doi:10.1007/978-981-15-1792-1_27 https://pubmed.ncbi.nlm.nih.gov/32342473/
Brolinson PG, Elliott D. Exercise and the immune system. Clin Sports Med. 2007;26(3):311-319. doi:10.1016/j.csm.2007.04.011 https://pubmed.ncbi.nlm.nih.gov/17826186/
Pedersen BK, Hoffman-Goetz L. Exercise and the immune system: regulation, integration, and adaptation. Physiol Rev. 2000;80(3):1055-1081. doi:10.1152/physrev.2000.80.3.1055 https://pubmed.ncbi.nlm.nih.gov/10893431/
Thomas R, Kenfield SA, Yanagisawa Y, Newton RU. Why exercise has a crucial role in cancer prevention, risk reduction and improved outcomes. Br Med Bull. 2021;139(1):100-119. doi:10.1093/bmb/ldab019 https://pubmed.ncbi.nlm.nih.gov/34426823/
McTiernan A, Friedenreich CM, Katzmarzyk PT, et al. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med Sci Sports Exerc. 2019;51(6):1252-1261. doi:10.1249/MSS.0000000000001937 https://pubmed.ncbi.nlm.nih.gov/31095082/
Fiuza-Luces C, Valenzuela PL, Gálvez BG, et al. The effect of physical exercise on anticancer immunity [published correction appears in Nat Rev Immunol. 2024 Feb 1;:]. Nat Rev Immunol. 2024;24(4):282-293. doi:10.1038/s41577-023-00943-0 https://pubmed.ncbi.nlm.nih.gov/37794239/
Malveiro C, Correia IR, Cargaleiro C, et al. Effects of exercise training on cancer patients undergoing neoadjuvant treatment: A systematic review. J Sci Med Sport. 2023;26(11):586-592. doi:10.1016/j.jsams.2023.08.178 https://pubmed.ncbi.nlm.nih.gov/37696693/
Yang L, Morielli AR, Heer E, et al. Effects of Exercise on Cancer Treatment Efficacy: A Systematic Review of Preclinical and Clinical Studies. Cancer Res. 2021;81(19):4889-4895. doi:10.1158/0008-5472.CAN-21-1258 https://pubmed.ncbi.nlm.nih.gov/34215623/
Koelwyn GJ, Zhuang X, Tammela T, Schietinger A, Jones LW. Exercise and immunometabolic regulation in cancer. Nat Metab. 2020;2(9):849-857. doi:10.1038/s42255-020-00277-4 https://pubmed.ncbi.nlm.nih.gov/32929232/
Zhang YB, Zhong XM, Han N, Tang H, Wang SY, Lin WX. Effectiveness of exercise interventions in the management of cancer-related fatigue: a systematic review of systematic reviews. Support Care Cancer. 2023;31(3):153. Published 2023 Feb 7. doi:10.1007/s00520-023-07619-4 https://pubmed.ncbi.nlm.nih.gov/36746815/
Spanoudaki M, Giaginis C, Karafyllaki D, et al. Exercise as a Promising Agent against Cancer: Evaluating Its Anti-Cancer Molecular Mechanisms. Cancers (Basel). 2023;15(21):5135. Published 2023 Oct 25. doi:10.3390/cancers15215135 https://pubmed.ncbi.nlm.nih.gov/37958310/
Cormie P, Zopf EM, Zhang X, Schmitz KH. The Impact of Exercise on Cancer Mortality, Recurrence, and Treatment-Related Adverse Effects. Epidemiol Rev. 2017;39(1):71-92. doi:10.1093/epirev/mxx007 https://pubmed.ncbi.nlm.nih.gov/28453622/
Hackney AC, Lane AR. Exercise and the Regulation of Endocrine Hormones. Prog Mol Biol Transl Sci. 2015;135:293-311. doi:10.1016/bs.pmbts.2015.07.001 https://pubmed.ncbi.nlm.nih.gov/26477919/
Spiegelman B, editor. Hormones, Metabolism and the Benefits of Exercise [Internet]. Cham (CH): Springer; 2017. doi: 10.1007/978-3-319-72790-5 https://www.ncbi.nlm.nih.gov/books/NBK543781/
Hackney AC, Walz EA. Hormonal adaptation and the stress of exercise training: the role of glucocorticoids. Trends Sport Sci. 2013;20(4):165-171. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5988244/
Shele G, Genkil J, Speelman D. A Systematic Review of the Effects of Exercise on Hormones in Women with Polycystic Ovary Syndrome. J Funct Morphol Kinesiol. 2020;5(2):35. Published 2020 May 31. doi:10.3390/jfmk5020035 https://pubmed.ncbi.nlm.nih.gov/33467251/
Zouhal H, Jayavel A, Parasuraman K, et al. Effects of Exercise Training on Anabolic and Catabolic Hormones with Advanced Age: A Systematic Review. Sports Med. 2022;52(6):1353-1368. doi:10.1007/s40279-021-01612-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9124654/
Ennour-Idrissi K, Maunsell E, Diorio C. Effect of physical activity on sex hormones in women: a systematic review and meta-analysis of randomized controlled trials. Breast Cancer Res. 2015;17(1):139. Published 2015 Nov 5. doi:10.1186/s13058-015-0647-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4635995/
Butt MS, Saleem J, Zakar R, Aiman S, Khan MZ, Fischer F. Benefits of physical activity on reproductive health functions among polycystic ovarian syndrome women: a systematic review. BMC Public Health. 2023;23(1):882. Published 2023 May 12. doi:10.1186/s12889-023-15730-8 https://pubmed.ncbi.nlm.nih.gov/37173672/
Hackney, A., Kraemer, W., Hooper, D. (2016). Hormonal Changes Associated with Physical Activity and Exercise Training. In: Vaamonde, D., du Plessis, S., Agarwal, A. (eds) Exercise and Human Reproduction. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3402-7_8
Mena GP, Mielke GI, Brown WJ. The effect of physical activity on reproductive health outcomes in young women: a systematic review and meta-analysis. Hum Reprod Update. 2019;25(5):541-563. doi:10.1093/humupd/dmz013 https://pubmed.ncbi.nlm.nih.gov/31304974/
Xie F, You Y, Guan C, Gu Y, Yao F, Xu J. Association between physical activity and infertility: a comprehensive systematic review and meta-analysis. J Transl Med. 2022;20(1):237. Published 2022 May 23. doi:10.1186/s12967-022-03426-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9125843/
Brinson AK, da Silva SG, Hesketh KR, Evenson KR. Impact of Physical Activity and Sedentary Behavior on Spontaneous Female and Male Fertility: A Systematic Review. J Phys Act Health. 2023;20(7):600-615. Published 2023 May 5. doi:10.1123/jpah.2022-0487 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7614776/
Mussawar M, Balsom AA, Totosy de Zepetnek JO, Gordon JL. The effect of physical activity on fertility: a mini-review. F S Rep. 2023;4(2):150-158. Published 2023 Apr 14. doi:10.1016/j.xfre.2023.04.005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10310950/
Butt MS, Saleem J, Zakar R, Aiman S, Khan MZ, Fischer F. Benefits of physical activity on reproductive health functions among polycystic ovarian syndrome women: a systematic review. BMC Public Health. 2023;23(1):882. Published 2023 May 12. doi:10.1186/s12889-023-15730-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10176874/
Harrison CL, Brown WJ, Hayman M, Moran LJ, Redman LM. The Role of Physical Activity in Preconception, Pregnancy and Postpartum Health. Semin Reprod Med. 2016;34(2):e28-e37. doi:10.1055/s-0036-1583530 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6986386/
Ahrens KA, Vladutiu CJ, Mumford SL, et al. The effect of physical activity across the menstrual cycle on reproductive function. Ann Epidemiol. 2014;24(2):127-134. doi:10.1016/j.annepidem.2013.11.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3946734/
Redman LM. Physical activity and its effects on reproduction. Reprod Biomed Online. 2006;12(5):579-586. doi:10.1016/s1472-6483(10)61183-2 https://pubmed.ncbi.nlm.nih.gov/16790101/
Orio F, Muscogiuri G, Ascione A, et al. Effects of physical exercise on the female reproductive system. Minerva Endocrinol. 2013;38(3):305-319. https://pubmed.ncbi.nlm.nih.gov/24126551/
Kakargia E, Mamalakis E, Frountzas M, Anagnostou E, Siristatidis C. The role of maternal physical activity on in vitro fertilization outcomes: a systematic review and meta-analysis. Arch Gynecol Obstet. 2023;307(6):1667-1676. doi:10.1007/s00404-022-06606-0 https://pubmed.ncbi.nlm.nih.gov/35596747/
Sun B, Messerlian C, Sun ZH, et al. Physical activity and sedentary time in relation to semen quality in healthy men screened as potential sperm donors. Hum Reprod. 2019;34(12):2330-2339. doi:10.1093/humrep/dez226 https://pubmed.ncbi.nlm.nih.gov/31858122/
Evenson KR, Hesketh KR. Studying the Complex Relationships Between Physical Activity and Infertility. Am J Lifestyle Med. 2016;10(4):232-234. doi:10.1177/1559827616641379 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5123562/
Belladelli F, Basran S, Eisenberg ML. Male Fertility and Physical Exercise. World J Mens Health. 2023;41(3):482-488. doi:10.5534/wjmh.220199 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10307666/
Wise LA, Rothman KJ, Mikkelsen EM, Sørensen HT, Riis AH, Hatch EE. A prospective cohort study of physical activity and time to pregnancy. Fertil Steril. 2012;97(5):1136-42.e424. doi:10.1016/j.fertnstert.2012.02.025 https://pubmed.ncbi.nlm.nih.gov/22425198/
Fergus KB, Gaither TW, Baradaran N, Glidden DV, Cohen AJ, Breyer BN. Exercise Improves Self-Reported Sexual Function Among Physically Active Adults. J Sex Med. 2019;16(8):1236-1245. doi:10.1016/j.jsxm.2019.04.020 https://pubmed.ncbi.nlm.nih.gov/31155388/
Simon RM, Howard L, Zapata D, Frank J, Freedland SJ, Vidal AC. The association of exercise with both erectile and sexual function in black and white men. J Sex Med. 2015;12(5):1202-1210. doi:10.1111/jsm.12869 https://pubmed.ncbi.nlm.nih.gov/25801073/
Jiannine LM. An investigation of the relationship between physical fitness, self-concept, and sexual functioning. J Educ Health Promot. 2018;7:57. Published 2018 May 3. doi:10.4103/jehp.jehp_157_17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963213/
Kumagai H, Myoenzono K, Yoshikawa T, Tsujimoto T, Shimomura K, Maeda S. Regular aerobic exercise improves sexual function assessed by the Aging Males’ Symptoms questionnaire in adult men. Aging Male. 2020;23(5):1194-1201. doi:10.1080/13685538.2020.1724940 https://pubmed.ncbi.nlm.nih.gov/32048543/
Stanton AM, Handy AB, Meston CM. The Effects of Exercise on Sexual Function in Women. Sex Med Rev. 2018;6(4):548-557. doi:10.1016/j.sxmr.2018.02.004 https://pubmed.ncbi.nlm.nih.gov/29606554/
Almuqahwi A, Alabdrabulridha H, Aljumaiah RM, et al. A Systematic Review on the Relationship Between Physical Activity and Sexual Function in Adults. Cureus. 2023;15(12):e51307. Published 2023 Dec 29. doi:10.7759/cureus.51307 https://pubmed.ncbi.nlm.nih.gov/38288234/
Lorenz TA, Meston CM. Exercise improves sexual function in women taking antidepressants: results from a randomized crossover trial. Depress Anxiety. 2014;31(3):188-195. doi:10.1002/da.22208 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4039497/
Carcelén-Fraile MDC, Aibar-Almazán A, Martínez-Amat A, et al. Effects of Physical Exercise on Sexual Function and Quality of Sexual Life Related to Menopausal Symptoms in Peri- and Postmenopausal Women: A Systematic Review. Int J Environ Res Public Health. 2020;17(8):2680. Published 2020 Apr 14. doi:10.3390/ijerph17082680 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7215442/
Lara LA, Montenegro ML, Franco MM, Abreu DC, Rosa e Silva AC, Ferreira CH. Is the sexual satisfaction of postmenopausal women enhanced by physical exercise and pelvic floor muscle training?. J Sex Med. 2012;9(1):218-223. doi:10.1111/j.1743-6109.2011.02516.x https://pubmed.ncbi.nlm.nih.gov/22023812/
Hackney AC, Lane AR, Register-Mihalik J, Oʼleary CB. Endurance Exercise Training and Male Sexual Libido. Med Sci Sports Exerc. 2017;49(7):1383-1388. doi:10.1249/MSS.0000000000001235 https://pubmed.ncbi.nlm.nih.gov/28195945/
Levin S. Does Exercise Enhance Sexuality?. Phys Sportsmed. 1993;21(3):199-203. doi:10.1080/00913847.1993.11710346 https://pubmed.ncbi.nlm.nih.gov/27439052/
Mandolesi L, Polverino A, Montuori S, et al. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front Psychol. 2018;9:509. Published 2018 Apr 27. doi:10.3389/fpsyg.2018.00509 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5934999/
Chen C, Nakagawa S. Physical activity for cognitive health promotion: An overview of the underlying neurobiological mechanisms. Ageing Res Rev. 2023;86:101868. doi:10.1016/j.arr.2023.101868 https://pubmed.ncbi.nlm.nih.gov/36736379/
Hillman CH, McDonald KM, Logan NE. A Review of the Effects of Physical Activity on Cognition and Brain Health across Children and Adolescence. Nestle Nutr Inst Workshop Ser. 2020;95:116-126. doi:10.1159/000511508 https://pubmed.ncbi.nlm.nih.gov/33161407/
Erickson KI, Hillman C, Stillman CM, et al. Physical Activity, Cognition, and Brain Outcomes: A Review of the 2018 Physical Activity Guidelines. Med Sci Sports Exerc. 2019;51(6):1242-1251. doi:10.1249/MSS.0000000000001936 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527141/
Gomez-Pinilla F, Hillman C. The influence of exercise on cognitive abilities. Compr Physiol. 2013;3(1):403-428. doi:10.1002/cphy.c110063 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951958/
Hernández-Mendo A, Reigal RE, López-Walle JM, et al. Physical Activity, Sports Practice, and Cognitive Functioning: The Current Research Status. Front Psychol. 2019;10:2658. Published 2019 Dec 6. doi:10.3389/fpsyg.2019.02658 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6908518/
Dastamooz S, Sadeghi-Bahmani D, Farahani MHD, et al. The efficacy of physical exercise interventions on mental health, cognitive function, and ADHD symptoms in children and adolescents with ADHD: an umbrella review. EClinicalMedicine. 2023;62:102137. Published 2023 Aug 10. doi:10.1016/j.eclinm.2023.102137 https://pubmed.ncbi.nlm.nih.gov/37599910/
Bidzan-Bluma I, Lipowska M. Physical Activity and Cognitive Functioning of Children: A Systematic Review. Int J Environ Res Public Health. 2018;15(4):800. Published 2018 Apr 19. doi:10.3390/ijerph15040800 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5923842/
Falck RS, Davis JC, Best JR, Crockett RA, Liu-Ambrose T. Impact of exercise training on physical and cognitive function among older adults: a systematic review and meta-analysis. Neurobiol Aging. 2019;79:119-130. doi:10.1016/j.neurobiolaging.2019.03.007 https://pubmed.ncbi.nlm.nih.gov/31051329/
Huang X, Zhao X, Li B, et al. Comparative efficacy of various exercise interventions on cognitive function in patients with mild cognitive impairment or dementia: A systematic review and network meta-analysis. J Sport Health Sci. 2022;11(2):212-223. doi:10.1016/j.jshs.2021.05.003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9068743/
Stillman CM, Esteban-Cornejo I, Brown B, Bender CM, Erickson KI. Effects of Exercise on Brain and Cognition Across Age Groups and Health States. Trends Neurosci. 2020;43(7):533-543. doi:10.1016/j.tins.2020.04.010 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9068803/
Gomes-Osman J, Cabral DF, Morris TP, et al. Exercise for cognitive brain health in aging: A systematic review for an evaluation of dose. Neurol Clin Pract. 2018;8(3):257-265. doi:10.1212/CPJ.0000000000000460 https://pubmed.ncbi.nlm.nih.gov/30105166/
Schuch FB, Vancampfort D. Physical activity, exercise, and mental disorders: it is time to move on. Trends Psychiatry Psychother. 2021;43(3):177-184. doi:10.47626/2237-6089-2021-0237 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8638711/
Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. 2017;106:48-56. doi:10.1016/j.maturitas.2017.09.003 https://pubmed.ncbi.nlm.nih.gov/29150166/
Smith PJ, Merwin RM. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu Rev Med. 2021;72:45-62. doi:10.1146/annurev-med-060619-022943 https://pubmed.ncbi.nlm.nih.gov/33256493/
Hu MX, Turner D, Generaal E, et al. Exercise interventions for the prevention of depression: a systematic review of meta-analyses. BMC Public Health. 2020;20(1):1255. Published 2020 Aug 18. doi:10.1186/s12889-020-09323-y https://pubmed.ncbi.nlm.nih.gov/32811468/
Noetel M, Sanders T, Gallardo-Gómez D, et al. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2024;384:e075847. Published 2024 Feb 14. doi:10.1136/bmj-2023-075847 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10870815/
Chekroud SR, Gueorguieva R, Zheutlin AB, et al. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5(9):739-746. doi:10.1016/S2215-0366(18)30227-X https://pubmed.ncbi.nlm.nih.gov/30099000/
Cooney G. Exercise and mental health: a complex and challenging relationship. Lancet Psychiatry. 2018;5(9):692-693. doi:10.1016/S2215-0366(18)30291-8 https://pubmed.ncbi.nlm.nih.gov/30099001/
Yu Q, Wong KK, Lei OK, et al. Comparative Effectiveness of Multiple Exercise Interventions in the Treatment of Mental Health Disorders: A Systematic Review and Network Meta-Analysis. Sports Med Open. 2022;8(1):135. Published 2022 Oct 29. doi:10.1186/s40798-022-00529-5 https://pubmed.ncbi.nlm.nih.gov/36308622/
Faulkner G, Biddle S. Exercise and mental health: it’s just not psychology!. J Sports Sci. 2001;19(6):433-444. doi:10.1080/026404101300149384 https://pubmed.ncbi.nlm.nih.gov/11411779/
Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;2013(9):CD004366. Published 2013 Sep 12. doi:10.1002/14651858.CD004366.pub6 https://pubmed.ncbi.nlm.nih.gov/24026850/
Xie Y, Wu Z, Sun L, et al. The Effects and Mechanisms of Exercise on the Treatment of Depression. Front Psychiatry. 2021;12:705559. Published 2021 Nov 5. doi:10.3389/fpsyt.2021.705559 https://pubmed.ncbi.nlm.nih.gov/34803752/
Kandola A, Stubbs B. Exercise and Anxiety. Adv Exp Med Biol. 2020;1228:345-352. doi:10.1007/978-981-15-1792-1_23 https://pubmed.ncbi.nlm.nih.gov/32342469/
Aylett E, Small N, Bower P. Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Serv Res. 2018;18(1):559. Published 2018 Jul 16. doi:10.1186/s12913-018-3313-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048763/
Jayakody K, Gunadasa S, Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48(3):187-196. doi:10.1136/bjsports-2012-091287 https://pubmed.ncbi.nlm.nih.gov/23299048/
Stonerock GL, Hoffman BM, Smith PJ, Blumenthal JA. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann Behav Med. 2015;49(4):542-556. doi:10.1007/s12160-014-9685-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4498975/
Connor M, Hargreaves EA, Scanlon OK, Harrison OK. The Effect of Acute Exercise on State Anxiety: A Systematic Review. Sports (Basel). 2023;11(8):145. Published 2023 Aug 1. doi:10.3390/sports11080145 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10459808/
Ben-Zeev T, Shoenfeld Y, Hoffman JR. The Effect of Exercise on Neurogenesis in the Brain. Isr Med Assoc J. 2022;24(8):533-538. https://pubmed.ncbi.nlm.nih.gov/35971998/
Saraulli D, Costanzi M, Mastrorilli V, Farioli-Vecchioli S. The Long Run: Neuroprotective Effects of Physical Exercise on Adult Neurogenesis from Youth to Old Age. Curr Neuropharmacol. 2017;15(4):519-533. doi:10.2174/1570159X14666160412150223 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5543673/
Augusto-Oliveira M, Arrifano GP, Leal-Nazaré CG, et al. Exercise Reshapes the Brain: Molecular, Cellular, and Structural Changes Associated with Cognitive Improvements. Mol Neurobiol. 2023;60(12):6950-6974. doi:10.1007/s12035-023-03492-8 https://pubmed.ncbi.nlm.nih.gov/37518829/
Tikac G, Unal A, Altug F. Regular exercise improves the levels of self-efficacy, self-esteem and body awareness of young adults. J Sports Med Phys Fitness. 2022;62(1):157-161. doi:10.23736/S0022-4707.21.12143-7 https://pubmed.ncbi.nlm.nih.gov/33555673/
Zamani Sani SH, Fathirezaie Z, Brand S, et al. Physical activity and self-esteem: testing direct and indirect relationships associated with psychological and physical mechanisms. Neuropsychiatr Dis Treat. 2016;12:2617-2625. Published 2016 Oct 12. doi:10.2147/NDT.S116811 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5068479/
Toros T, Ogras EB, Toy AB, et al. The Impact of Regular Exercise on Life Satisfaction, Self-Esteem, and Self-Efficacy in Older Adults. Behav Sci (Basel). 2023;13(9):714. Published 2023 Aug 28. doi:10.3390/bs13090714 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10525489/
Mahindru A, Patil P, Agrawal V. Role of Physical Activity on Mental Health and Well-Being: A Review. Cureus. 2023;15(1):e33475. Published 2023 Jan 7. doi:10.7759/cureus.33475 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9902068/
Sonstroem RJ. Exercise and self-esteem. Exerc Sport Sci Rev. 1984;12:123-155. https://pubmed.ncbi.nlm.nih.gov/6376132/
Campbell A, Hausenblas HA. Effects of exercise interventions on body image: a meta-analysis. J Health Psychol. 2009;14(6):780-793. doi:10.1177/1359105309338977 https://pubmed.ncbi.nlm.nih.gov/19687115/
Björkman F, Ekblom Ö. Physical Exercise as Treatment for PTSD: A Systematic Review and Meta-Analysis. Mil Med. 2022;187(9-10):e1103-e1113. doi:10.1093/milmed/usab497 https://pubmed.ncbi.nlm.nih.gov/34850063/
Jadhakhan F, Lambert N, Middlebrook N, Evans DW, Falla D. Is exercise/physical activity effective at reducing symptoms of post-traumatic stress disorder in adults – A systematic review. Front Psychol. 2022;13:943479. Published 2022 Aug 12. doi:10.3389/fpsyg.2022.943479 https://pubmed.ncbi.nlm.nih.gov/36033016/
Oppizzi LM, Umberger R. The Effect of Physical Activity on PTSD. Issues Ment Health Nurs. 2018;39(2):179-187. doi:10.1080/01612840.2017.1391903 https://pubmed.ncbi.nlm.nih.gov/29319376/
Hegberg NJ, Hayes JP, Hayes SM. Exercise Intervention in PTSD: A Narrative Review and Rationale for Implementation. Front Psychiatry. 2019;10:133. Published 2019 Mar 21. doi:10.3389/fpsyt.2019.00133 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6437073/
Martinez-Calderon J, Villar-Alises O, García-Muñoz C, Pineda-Escobar S, Matias-Soto J. Multimodal exercise programs may improve posttraumatic stress disorders symptoms and quality of life in adults with PTSD: An overview of systematic reviews with meta-analysis. Clin Rehabil. 2024;38(5):573-588. doi:10.1177/02692155231225466 https://pubmed.ncbi.nlm.nih.gov/38258461/
Fetzner MG, Asmundson GJ. Aerobic Exercise Reduces Symptoms of Posttraumatic Stress Disorder: A Randomized Controlled Trial. Cogn Behav Ther. 2015;44(4):301-313. doi:10.1080/16506073.2014.916745 https://pubmed.ncbi.nlm.nih.gov/24911173/
Patterson MS, Spadine MN, Graves Boswell T, et al. Exercise in the Treatment of Addiction: A Systematic Literature Review. Health Educ Behav. Published online April 29, 2022. doi:10.1177/10901981221090155 https://pubmed.ncbi.nlm.nih.gov/35484950/
Linke SE, Ussher M. Exercise-based treatments for substance use disorders: evidence, theory, and practicality. Am J Drug Alcohol Abuse. 2015;41(1):7-15. doi:10.3109/00952990.2014.976708 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4831948/
Wang D, Wang Y, Wang Y, Li R, Zhou C. Impact of physical exercise on substance use disorders: a meta-analysis. PLoS One. 2014;9(10):e110728. Published 2014 Oct 16. doi:10.1371/journal.pone.0110728 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199732/
Zhang Z, Liu X. A Systematic Review of Exercise Intervention Program for People With Substance Use Disorder. Front Psychiatry. 2022;13:817927. Published 2022 Mar 11. doi:10.3389/fpsyt.2022.817927 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8962945/
Thompson TP, Horrell J, Taylor AH, et al. Physical activity and the prevention, reduction, and treatment of alcohol and other drug use across the lifespan (The PHASE review): A systematic review. Ment Health Phys Act. 2020;19:100360. doi:10.1016/j.mhpa.2020.100360 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7527800/
Chen, YT., Fredericson, M., Matheson, G. et al. Exercise is Medicine. Curr Phys Med Rehabil Rep 1, 48–56 (2013). https://link.springer.com/article/10.1007/s40141-013-0006-1
Sallis RE. Exercise is medicine and physicians need to prescribe it!. Br J Sports Med. 2009;43(1):3-4. doi:10.1136/bjsm.2008.054825 https://pubmed.ncbi.nlm.nih.gov/18971243/
Sallis R. Exercise is medicine: a call to action for physicians to assess and prescribe exercise. Phys Sportsmed. 2015;43(1):22-26. doi:10.1080/00913847.2015.1001938 https://pubmed.ncbi.nlm.nih.gov/25684558/
Li J, Qiu H, Li J. Exercise is medicine. Front Aging Neurosci. 2023;15:1129221. Published 2023 Jan 30. doi:10.3389/fnagi.2023.1129221 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9922893/
Langan SP, Grosicki GJ. Exercise Is Medicine…and the Dose Matters. Front Physiol. 2021;12:660818. Published 2021 May 12. doi:10.3389/fphys.2021.660818 https://pubmed.ncbi.nlm.nih.gov/34054576/
Anderson E, Durstine JL. Physical activity, exercise, and chronic diseases: A brief review. Sports Med Health Sci. 2019;1(1):3-10. Published 2019 Sep 10. doi:10.1016/j.smhs.2019.08.006 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9219321/
Hamer M, Endrighi R, Poole L. Physical activity, stress reduction, and mood: insight into immunological mechanisms. Methods Mol Biol. 2012;934:89-102. doi:10.1007/978-1-62703-071-7_5 https://pubmed.ncbi.nlm.nih.gov/22933142/
El-Kotob R, Ponzano M, Chaput JP, et al. Resistance training and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S165-S179. doi:10.1139/apnm-2020-0245 https://pubmed.ncbi.nlm.nih.gov/33054335/
Shailendra P, Baldock KL, Li LSK, Bennie JA, Boyle T. Resistance Training and Mortality Risk: A Systematic Review and Meta-Analysis. Am J Prev Med. 2022;63(2):277-285. doi:10.1016/j.amepre.2022.03.020 https://pubmed.ncbi.nlm.nih.gov/35599175/
Paluch AE, Boyer WR, Franklin BA, et al. Resistance Exercise Training in Individuals With and Without Cardiovascular Disease: 2023 Update: A Scientific Statement From the American Heart Association. Circulation. 2024;149(3):e217-e231. doi:10.1161/CIR.0000000000001189 https://pubmed.ncbi.nlm.nih.gov/38059362/
Kraemer WJ, Ratamess NA, French DN. Resistance training for health and performance. Curr Sports Med Rep. 2002;1(3):165-171. doi:10.1249/00149619-200206000-00007 https://pubmed.ncbi.nlm.nih.gov/12831709/
Strasser B, Volaklis K, Fuchs D, Burtscher M. Role of Dietary Protein and Muscular Fitness on Longevity and Aging. Aging Dis. 2018;9(1):119-132. Published 2018 Feb 1. doi:10.14336/AD.2017.0202 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5772850/
McLeod M, Breen L, Hamilton DL, Philp A. Live strong and prosper: the importance of skeletal muscle strength for healthy ageing. Biogerontology. 2016;17(3):497-510. doi:10.1007/s10522-015-9631-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4889643/
Witard OC, McGlory C, Hamilton DL, Phillips SM. Growing older with health and vitality: a nexus of physical activity, exercise and nutrition. Biogerontology. 2016;17(3):529-546. doi:10.1007/s10522-016-9637-9 https://pubmed.ncbi.nlm.nih.gov/26878863/
Chen L, Nelson DR, Zhao Y, Cui Z, Johnston JA. Relationship between muscle mass and muscle strength, and the impact of comorbidities: a population-based, cross-sectional study of older adults in the United States. BMC Geriatr. 2013;13:74. Published 2013 Jul 16. doi:10.1186/1471-2318-13-74 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3765109/
Srikanthan P, Karlamangla AS. Muscle mass index as a predictor of longevity in older adults. Am J Med. 2014;127(6):547-553. doi:10.1016/j.amjmed.2014.02.007 https://pubmed.ncbi.nlm.nih.gov/24561114/
Moghetti P, Bacchi E, Brangani C, Donà S, Negri C. Metabolic Effects of Exercise. Front Horm Res. 2016;47:44-57. doi:10.1159/000445156 https://pubmed.ncbi.nlm.nih.gov/27348753/
Hong AR, Kim SW. Effects of Resistance Exercise on Bone Health. Endocrinol Metab (Seoul). 2018;33(4):435-444. doi:10.3803/EnM.2018.33.4.435 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279907/
Manaye S, Cheran K, Murthy C, et al. The Role of High-intensity and High-impact Exercises in Improving Bone Health in Postmenopausal Women: A Systematic Review. Cureus. 2023;15(2):e34644. Published 2023 Feb 5. doi:10.7759/cureus.34644 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9990535/
Liu Y, Lee DC, Li Y, et al. Associations of Resistance Exercise with Cardiovascular Disease Morbidity and Mortality. Med Sci Sports Exerc. 2019;51(3):499-508. doi:10.1249/MSS.0000000000001822 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385554/
Lee DC, Brellenthin AG, Lanningham-Foster LM, Kohut ML, Li Y. Aerobic, resistance, or combined exercise training and cardiovascular risk profile in overweight or obese adults: the CardioRACE trial. Eur Heart J. 2024;45(13):1127-1142. doi:10.1093/eurheartj/ehad827 https://pubmed.ncbi.nlm.nih.gov/38233024/
Halle M, Papadakis M. A new dawn of managing cardiovascular risk in obesity: the importance of combining lifestyle intervention and medication. Eur Heart J. 2024;45(13):1143-1145. doi:10.1093/eurheartj/ehae091 https://pubmed.ncbi.nlm.nih.gov/38366823/
Kirkman DL, Lee DC, Carbone S. Resistance exercise for cardiac rehabilitation. Prog Cardiovasc Dis. 2022;70:66-72. doi:10.1016/j.pcad.2022.01.004 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8930531/
Westcott WL. Resistance training is medicine: effects of strength training on health. Curr Sports Med Rep. 2012;11(4):209-216. doi:10.1249/JSR.0b013e31825dabb8 https://pubmed.ncbi.nlm.nih.gov/22777332/
Lavie CJ, Lee DC, Sui X, et al. Effects of Running on Chronic Diseases and Cardiovascular and All-Cause Mortality. Mayo Clin Proc. 2015;90(11):1541-1552. doi:10.1016/j.mayocp.2015.08.001 https://pubmed.ncbi.nlm.nih.gov/26362561/
Hackett DA. Lung Function and Respiratory Muscle Adaptations of Endurance- and Strength-Trained Males. Sports (Basel). 2020;8(12):160. Published 2020 Dec 10. doi:10.3390/sports8120160 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7764033/
Hellsten Y, Nyberg M. Cardiovascular Adaptations to Exercise Training. Compr Physiol. 2015;6(1):1-32. Published 2015 Dec 15. doi:10.1002/cphy.c140080 https://pubmed.ncbi.nlm.nih.gov/26756625/
Lässing J, Maudrich T, Kenville R, et al. Intensity-dependent cardiopulmonary response during and after strength training. Sci Rep. 2023;13(1):6632. Published 2023 Apr 24. doi:10.1038/s41598-023-33873-x https://pubmed.ncbi.nlm.nih.gov/37095279/
Benck LR, Cuttica MJ, Colangelo LA, et al. Association between Cardiorespiratory Fitness and Lung Health from Young Adulthood to Middle Age. Am J Respir Crit Care Med. 2017;195(9):1236-1243. doi:10.1164/rccm.201610-2089OC https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5439017/
Reimers AK, Knapp G, Reimers CD. Effects of Exercise on the Resting Heart Rate: A Systematic Review and Meta-Analysis of Interventional Studies. J Clin Med. 2018;7(12):503. Published 2018 Dec 1. doi:10.3390/jcm7120503 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306777/
Gielen S, Schuler G, Adams V. Cardiovascular effects of exercise training: molecular mechanisms. Circulation. 2010;122(12):1221-1238. doi:10.1161/CIRCULATIONAHA.110.939959 https://pubmed.ncbi.nlm.nih.gov/20855669/
Muscella A, Stefàno E, Marsigliante S. The effects of exercise training on lipid metabolism and coronary heart disease. Am J Physiol Heart Circ Physiol. 2020;319(1):H76-H88. doi:10.1152/ajpheart.00708.2019 https://pubmed.ncbi.nlm.nih.gov/32442027/
Wilson MG, Ellison GM, Cable NT. Basic science behind the cardiovascular benefits of exercise. Heart. 2015;101(10):758-765. doi:10.1136/heartjnl-2014-306596 https://pubmed.ncbi.nlm.nih.gov/25911667/
Franklin BA, Eijsvogels TMH, Pandey A, Quindry J, Toth PP. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the ASPC Part I: Bioenergetics, contemporary physical activity recommendations, benefits, risks, extreme exercise regimens, potential maladaptations. Am J Prev Cardiol. 2022;12:100424. Published 2022 Oct 13. doi:10.1016/j.ajpc.2022.100424 https://pubmed.ncbi.nlm.nih.gov/36281324/
Rao P, Belanger MJ, Robbins JM. Exercise, Physical Activity, and Cardiometabolic Health: Insights into the Prevention and Treatment of Cardiometabolic Diseases. Cardiol Rev. 2022;30(4):167-178. doi:10.1097/CRD.0000000000000416 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8920940/
Myers J, Kokkinos P, Nyelin E. Physical Activity, Cardiorespiratory Fitness, and the Metabolic Syndrome. Nutrients. 2019;11(7):1652. Published 2019 Jul 19. doi:10.3390/nu11071652 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6683051/
Giallauria F, Strisciuglio T, Cuomo G, et al. Exercise Training: The Holistic Approach in Cardiovascular Prevention. High Blood Press Cardiovasc Prev. 2021;28(6):561-577. doi:10.1007/s40292-021-00482-6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8590648/
Franklin BA, Wedig IJ, Sallis RE, Lavie CJ, Elmer SJ. Physical Activity and Cardiorespiratory Fitness as Modulators of Health Outcomes: A Compelling Research-Based Case Presented to the Medical Community. Mayo Clin Proc. 2023;98(2):316-331. doi:10.1016/j.mayocp.2022.09.011 https://pubmed.ncbi.nlm.nih.gov/36737120/
Reimers CD, Knapp G, Reimers AK. Does physical activity increase life expectancy? A review of the literature. J Aging Res. 2012;2012:243958. doi:10.1155/2012/243958 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3395188/
Santos AC, Willumsen J, Meheus F, Ilbawi A, Bull FC. The cost of inaction on physical inactivity to public health-care systems: a population-attributable fraction analysis. Lancet Glob Health. 2023;11(1):e32-e39. doi:10.1016/S2214-109X(22)00464-8 https://pubmed.ncbi.nlm.nih.gov/36480931/
Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219-229. doi:10.1016/S0140-6736(12)61031-9 https://pubmed.ncbi.nlm.nih.gov/22818936/
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants [published correction appears in Lancet Glob Health. 2019 Jan;7(1):e36]. Lancet Glob Health. 2018;6(10):e1077-e1086. doi:10.1016/S2214-109X(18)30357-7 https://pubmed.ncbi.nlm.nih.gov/30193830/
Duggal NA, Niemiro G, Harridge SDR, Simpson RJ, Lord JM. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity?. Nat Rev Immunol. 2019;19(9):563-572. doi:10.1038/s41577-019-0177-9 https://pubmed.ncbi.nlm.nih.gov/31175337/
Nusselder WJ, Franco OH, Peeters A, Mackenbach JP. Living healthier for longer: comparative effects of three heart-healthy behaviors on life expectancy with and without cardiovascular disease. BMC Public Health. 2009;9:487. Published 2009 Dec 24. doi:10.1186/1471-2458-9-487 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813239/
Gremeaux V, Gayda M, Lepers R, Sosner P, Juneau M, Nigam A. Exercise and longevity. Maturitas. 2012;73(4):312-317. doi:10.1016/j.maturitas.2012.09.012 https://pubmed.ncbi.nlm.nih.gov/23063021/
Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378(9798):1244-1253. doi:10.1016/S0140-6736(11)60749-6 https://pubmed.ncbi.nlm.nih.gov/21846575/
Kopp M, Burtscher M. Aiming at Optimal Physical Activity for Longevity (OPAL). Sports Med Open. 2021;7(1):70. Published 2021 Oct 9. doi:10.1186/s40798-021-00360-4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8502188/
Lee IM, Paffenbarger RS Jr, Hennekens CH. Physical activity, physical fitness and longevity. Aging (Milano). 1997;9(1-2):2-11. doi:10.1007/BF03340123 https://pubmed.ncbi.nlm.nih.gov/9177581/
Sheehan CM, Li L. Associations of Exercise Types with All-Cause Mortality among U.S. Adults. Med Sci Sports Exerc. 2020;52(12):2554-2562. doi:10.1249/MSS.0000000000002406 https://pubmed.ncbi.nlm.nih.gov/32520868/
Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study [published correction appears in Lancet. 2017 Dec 16;390(10113):2626]. Lancet. 2017;390(10113):2643-2654. doi:10.1016/S0140-6736(17)31634-3 https://pubmed.ncbi.nlm.nih.gov/28943267/
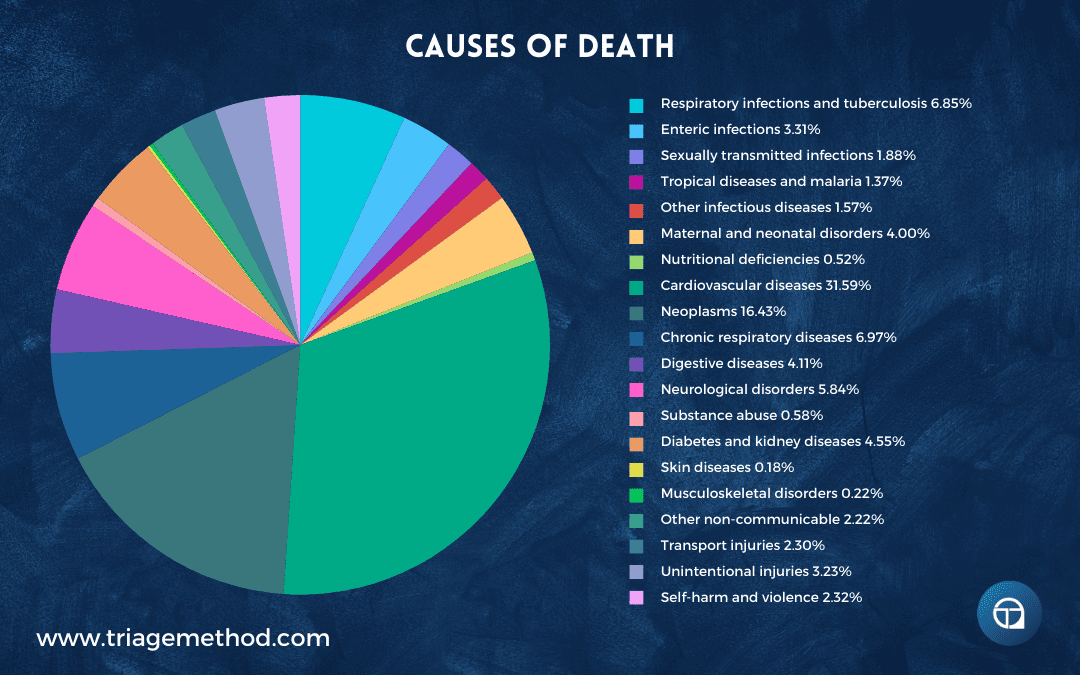
https://ourworldindata.org/causes-of-death
https://ourworldindata.org/grapher/leading-cause-of-death
https://ourworldindata.org/causes-of-death-treemap
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736-1788. doi:10.1016/S0140-6736(18)32203-7 https://pubmed.ncbi.nlm.nih.gov/30496103/
Ahmad FB, Anderson RN. The Leading Causes of Death in the US for 2020. JAMA. 2021;325(18):1829-1830. doi:10.1001/jama.2021.5469 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8145781/
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study [published correction appears in J Am Coll Cardiol. 2021 Apr 20;77(15):1958-1959]. J Am Coll Cardiol. 2020;76(25):2982-3021. doi:10.1016/j.jacc.2020.11.010 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7755038/
https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Khushalani JS, Song S, Calhoun BH, Puddy RW, Kucik JE. Preventing Leading Causes of Death: Systematic Review of Cost-Utility Literature. Am J Prev Med. 2022;62(2):275-284. doi:10.1016/j.amepre.2021.07.019 https://pubmed.ncbi.nlm.nih.gov/34736801/
https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
Marquez DX, Aguiñaga S, Vásquez PM, et al. A systematic review of physical activity and quality of life and well-being. Transl Behav Med. 2020;10(5):1098-1109. doi:10.1093/tbm/ibz198 https://pubmed.ncbi.nlm.nih.gov/33044541/
Campbell E, Petermann-Rocha F, Welsh P, et al. The effect of exercise on quality of life and activities of daily life in frail older adults: A systematic review of randomised control trials. Exp Gerontol. 2021;147:111287. doi:10.1016/j.exger.2021.111287 https://pubmed.ncbi.nlm.nih.gov/33609689/
Gill DL, Hammond CC, Reifsteck EJ, et al. Physical activity and quality of life. J Prev Med Public Health. 2013;46 Suppl 1(Suppl 1):S28-S34. doi:10.3961/jpmph.2013.46.S.S28 https://pubmed.ncbi.nlm.nih.gov/23412703/
Pucci GC, Rech CR, Fermino RC, Reis RS. Association between physical activity and quality of life in adults. Rev Saude Publica. 2012;46(1):166-179. doi:10.1590/s0034-89102012000100021 https://pubmed.ncbi.nlm.nih.gov/22249758/
Lima LV, Abner TSS, Sluka KA. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J Physiol. 2017;595(13):4141-4150. doi:10.1113/JP273355 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5491894/
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4(4):CD011279. Published 2017 Apr 24. doi:10.1002/14651858.CD011279.pub3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5461882/
Niederstrasser NG, Attridge N. Associations between pain and physical activity among older adults. PLoS One. 2022;17(1):e0263356. Published 2022 Jan 28. doi:10.1371/journal.pone.0263356 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8797193/
Søgaard K, Sjøgaard G. Physical Activity as Cause and Cure of Muscular Pain: Evidence of Underlying Mechanisms. Exerc Sport Sci Rev. 2017;45(3):136-145. doi:10.1249/JES.0000000000000112 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5473374/
Law LF, Sluka KA. How does physical activity modulate pain?. Pain. 2017;158(3):369-370. doi:10.1097/j.pain.0000000000000792 https://pubmed.ncbi.nlm.nih.gov/28135214/
Skou ST, Bricca A, Roos EM. The impact of physical activity level on the short- and long-term pain relief from supervised exercise therapy and education: a study of 12,796 Danish patients with knee osteoarthritis. Osteoarthritis Cartilage. 2018;26(11):1474-1478. doi:10.1016/j.joca.2018.07.010 https://pubmed.ncbi.nlm.nih.gov/30076884/
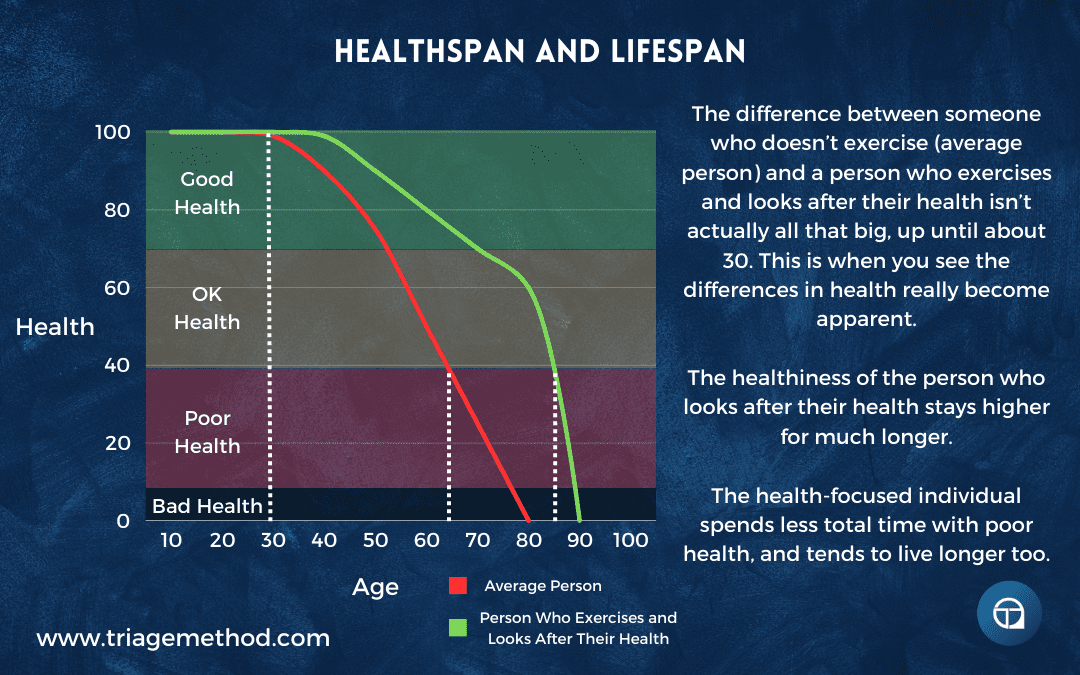
Guan Y, Yan Z. Molecular Mechanisms of Exercise and Healthspan. Cells. 2022;11(5):872. Published 2022 Mar 3. doi:10.3390/cells11050872 https://pubmed.ncbi.nlm.nih.gov/35269492/
Broskey NT, Marlatt KL, Most J, Erickson ML, Irving BA, Redman LM. The Panacea of Human Aging: Calorie Restriction Versus Exercise. Exerc Sport Sci Rev. 2019;47(3):169-175. doi:10.1249/JES.0000000000000193 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6579613/
Crimmins EM. Lifespan and Healthspan: Past, Present, and Promise. Gerontologist. 2015;55(6):901-911. doi:10.1093/geront/gnv130 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4861644/
Kaeberlein M. How healthy is the healthspan concept?. Geroscience. 2018;40(4):361-364. doi:10.1007/s11357-018-0036-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6136295/
Tchkonia T, Palmer AK, Kirkland JL. New Horizons: Novel Approaches to Enhance Healthspan Through Targeting Cellular Senescence and Related Aging Mechanisms. J Clin Endocrinol Metab. 2021;106(3):e1481-e1487. doi:10.1210/clinem/dgaa728 https://pubmed.ncbi.nlm.nih.gov/33155651/
Garmany A, Yamada S, Terzic A. Longevity leap: mind the healthspan gap. NPJ Regen Med. 2021;6(1):57. Published 2021 Sep 23. doi:10.1038/s41536-021-00169-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8460831/
Leyk D, Rüther T, Wunderlich M, et al. Physical performance in middle age and old age: good news for our sedentary and aging society. Dtsch Arztebl Int. 2010;107(46):809-816. doi:10.3238/arztebl.2010.0809 https://pubmed.ncbi.nlm.nih.gov/21151416/
Lepers R, Cattagni T. Do older athletes reach limits in their performance during marathon running?. Age (Dordr). 2012;34(3):773-781. doi:10.1007/s11357-011-9271-z https://pubmed.ncbi.nlm.nih.gov/21617894/
Lepers R, Stapley PJ. Master Athletes Are Extending the Limits of Human Endurance. Front Physiol. 2016;7:613. Published 2016 Dec 12. doi:10.3389/fphys.2016.00613 https://pubmed.ncbi.nlm.nih.gov/28018241/
Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2014;3(4):346-350. Published 2014 Feb 24. https://pubmed.ncbi.nlm.nih.gov/24596700/
Wilkinson DJ, Piasecki M, Atherton PJ. The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res Rev. 2018;47:123-132. doi:10.1016/j.arr.2018.07.005 https://pubmed.ncbi.nlm.nih.gov/30048806/
Trombetti A, Reid KF, Hars M, et al. Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporos Int. 2016;27(2):463-471. doi:10.1007/s00198-015-3236-5 https://pubmed.ncbi.nlm.nih.gov/26194491/
Larsson L, Degens H, Li M, et al. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol Rev. 2019;99(1):427-511. doi:10.1152/physrev.00061.2017 https://pubmed.ncbi.nlm.nih.gov/30427277/
Moradell A, Casajús JA, Moreno LA, Vicente-Rodríguez G, Gómez-Cabello A. Effects of Diet-Exercise Interaction on Human Health across a Lifespan. Nutrients. 2023;15(11):2520. Published 2023 May 29. doi:10.3390/nu15112520 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10255595/
Malsagova KA, Kopylov AT, Sinitsyna AA, et al. Sports Nutrition: Diets, Selection Factors, Recommendations. Nutrients. 2021;13(11):3771. Published 2021 Oct 25. doi:10.3390/nu13113771 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8619485/
Koehler K, Drenowatz C. Integrated Role of Nutrition and Physical Activity for Lifelong Health. Nutrients. 2019;11(7):1437. Published 2019 Jun 26. doi:10.3390/nu11071437 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6682932/
Nitschke E, Gottesman K, Hamlett P, et al. Impact of Nutrition and Physical Activity Interventions Provided by Nutrition and Exercise Practitioners for the Adult General Population: A Systematic Review and Meta-Analysis. Nutrients. 2022;14(9):1729. Published 2022 Apr 21. doi:10.3390/nu14091729 https://pubmed.ncbi.nlm.nih.gov/35565696/
Denison HJ, Cooper C, Sayer AA, Robinson SM. Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Interv Aging. 2015;10:859-869. Published 2015 May 11. doi:10.2147/CIA.S55842 https://pubmed.ncbi.nlm.nih.gov/25999704/
Kerksick CM, Wilborn CD, Roberts MD, et al. ISSN exercise & sports nutrition review update: research & recommendations. J Int Soc Sports Nutr. 2018;15(1):38. Published 2018 Aug 1. doi:10.1186/s12970-018-0242-y https://pubmed.ncbi.nlm.nih.gov/30068354/
Alexander L, Christensen SM, Richardson L, et al. Nutrition and physical activity: An Obesity Medicine Association (OMA) Clinical Practice Statement 2022. Obes Pillars. 2022;1:100005. Published 2022 Jan 10. doi:10.1016/j.obpill.2021.100005 https://pubmed.ncbi.nlm.nih.gov/38085928/
Willis LH, Slentz CA, Bateman LA, et al. Effects of aerobic and/or resistance training on body mass and fat mass in overweight or obese adults. J Appl Physiol (1985). 2012;113(12):1831-1837. doi:10.1152/japplphysiol.01370.2011 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3544497/
MacKenzie-Shalders K, Kelly JT, So D, Coffey VG, Byrne NM. The effect of exercise interventions on resting metabolic rate: A systematic review and meta-analysis. J Sports Sci. 2020;38(14):1635-1649. doi:10.1080/02640414.2020.1754716 https://pubmed.ncbi.nlm.nih.gov/32397898/
Trexler ET, Smith-Ryan AE, Norton LE. Metabolic adaptation to weight loss: implications for the athlete. J Int Soc Sports Nutr. 2014;11(1):7. Published 2014 Feb 27. doi:10.1186/1550-2783-11-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3943438/
Bingham SA, Goldberg GR, Coward WA, Prentice AM, Cummings JH. The effect of exercise and improved physical fitness on basal metabolic rate. Br J Nutr. 1989;61(2):155-173. doi:10.1079/bjn19890106 https://pubmed.ncbi.nlm.nih.gov/2706222/
Yu WW, Lee S, Arslanian S, Tamim H, Kuk JL. Effects of Exercise on Resting Metabolic Rate in Adolescents with Overweight and Obesity. Child Obes. 2021;17(4):249-256. doi:10.1089/chi.2020.0280 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8147485/
Speakman JR, Selman C. Physical activity and resting metabolic rate. Proc Nutr Soc. 2003;62(3):621-634. doi:10.1079/PNS2003282 https://pubmed.ncbi.nlm.nih.gov/14692598/
Oikawa SY, Brisbois TD, van Loon LJC, Rollo I. Eat like an athlete: insights of sports nutrition science to support active aging in healthy older adults. Geroscience. 2021;43(5):2485-2495. doi:10.1007/s11357-021-00419-w https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8599603/
Ritson AJ, Hearris MA, Bannock LG. Bridging the gap: Evidence-based practice guidelines for sports nutritionists. Front Nutr. 2023;10:1118547. Published 2023 Mar 29. doi:10.3389/fnut.2023.1118547 https://pubmed.ncbi.nlm.nih.gov/37063331/
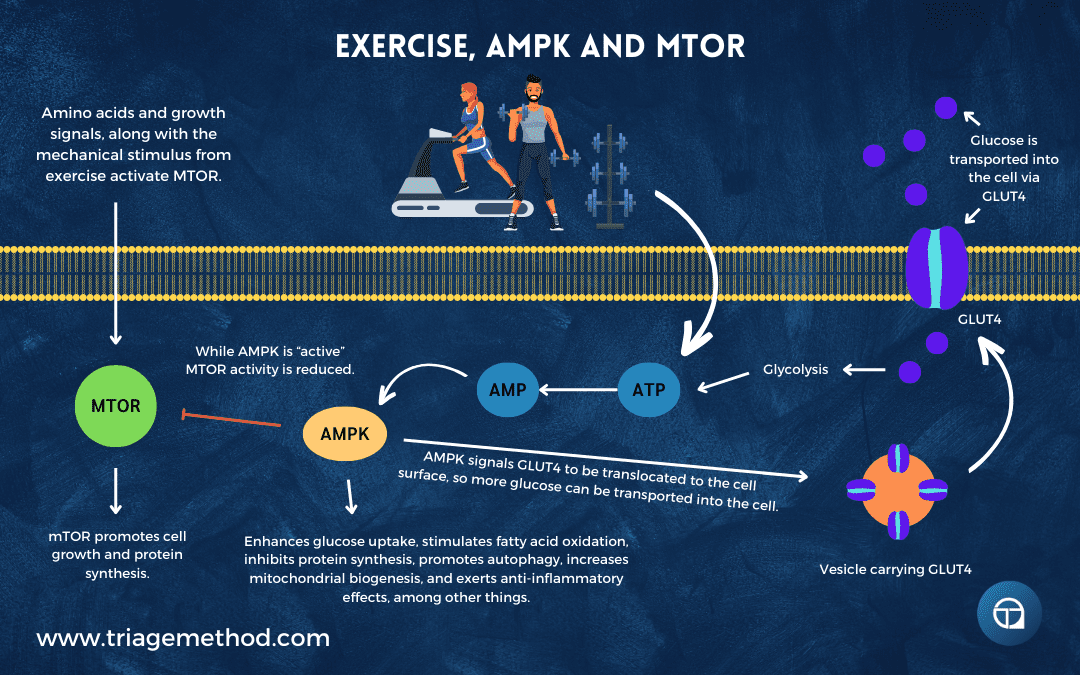
Richter EA, Ruderman NB. AMPK and the biochemistry of exercise: implications for human health and disease. Biochem J. 2009;418(2):261-275. doi:10.1042/BJ20082055 https://pubmed.ncbi.nlm.nih.gov/19196246/
Lantier L, Fentz J, Mounier R, et al. AMPK controls exercise endurance, mitochondrial oxidative capacity, and skeletal muscle integrity. FASEB J. 2014;28(7):3211-3224. doi:10.1096/fj.14-250449 https://pubmed.ncbi.nlm.nih.gov/24652947/
McConell GK. It’s well and truly time to stop stating that AMPK regulates glucose uptake and fat oxidation during exercise. Am J Physiol Endocrinol Metab. 2020;318(4):E564-E567. doi:10.1152/ajpendo.00511.2019 https://pubmed.ncbi.nlm.nih.gov/32017593/
Niederberger E, King TS, Russe OQ, Geisslinger G. Activation of AMPK and its Impact on Exercise Capacity. Sports Med. 2015;45(11):1497-1509. doi:10.1007/s40279-015-0366-z https://pubmed.ncbi.nlm.nih.gov/26186961/
Jorgensen SB, Rose AJ. How is AMPK activity regulated in skeletal muscles during exercise?. Front Biosci. 2008;13:5589-5604. Published 2008 May 1. doi:10.2741/3102 https://pubmed.ncbi.nlm.nih.gov/18508608/
Watson K, Baar K. mTOR and the health benefits of exercise. Semin Cell Dev Biol. 2014;36:130-139. doi:10.1016/j.semcdb.2014.08.013 https://pubmed.ncbi.nlm.nih.gov/25218794/
Yoon MS. mTOR as a Key Regulator in Maintaining Skeletal Muscle Mass. Front Physiol. 2017;8:788. Published 2017 Oct 17. doi:10.3389/fphys.2017.00788 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5650960/
Jones TW, Eddens L, Kupusarevic J, et al. Aerobic exercise intensity does not affect the anabolic signaling following resistance exercise in endurance athletes. Sci Rep. 2021;11(1):10785. Published 2021 May 24. doi:10.1038/s41598-021-90274-8 https://pubmed.ncbi.nlm.nih.gov/34031501/
Ogasawara R, Kobayashi K, Tsutaki A, et al. mTOR signaling response to resistance exercise is altered by chronic resistance training and detraining in skeletal muscle. J Appl Physiol (1985). 2013;114(7):934-940. doi:10.1152/japplphysiol.01161.2012 https://pubmed.ncbi.nlm.nih.gov/23372143/
Song Z, Moore DR, Hodson N, et al. Resistance exercise initiates mechanistic target of rapamycin (mTOR) translocation and protein complex co-localisation in human skeletal muscle. Sci Rep. 2017;7(1):5028. Published 2017 Jul 10. doi:10.1038/s41598-017-05483-x https://pubmed.ncbi.nlm.nih.gov/28694500/
Chen J, Zhou R, Feng Y, Cheng L. Molecular mechanisms of exercise contributing to tissue regeneration. Signal Transduct Target Ther. 2022;7(1):383. Published 2022 Nov 30. doi:10.1038/s41392-022-01233-2 https://pubmed.ncbi.nlm.nih.gov/36446784/
Burd NA, Tang JE, Moore DR, Phillips SM. Exercise training and protein metabolism: influences of contraction, protein intake, and sex-based differences. J Appl Physiol (1985). 2009;106(5):1692-1701. doi:10.1152/japplphysiol.91351.2008 https://pubmed.ncbi.nlm.nih.gov/19036897/
Ogasawara R, Sato K, Matsutani K, Nakazato K, Fujita S. The order of concurrent endurance and resistance exercise modifies mTOR signaling and protein synthesis in rat skeletal muscle. Am J Physiol Endocrinol Metab. 2014;306(10):E1155-E1162. doi:10.1152/ajpendo.00647.2013 https://pubmed.ncbi.nlm.nih.gov/24691029/
Thackray AE, Stensel DJ. The impact of acute exercise on appetite control: Current insights and future perspectives. Appetite. 2023;186:106557. doi:10.1016/j.appet.2023.106557 https://pubmed.ncbi.nlm.nih.gov/37044176/
Panissa VLG, Cardoso LK, Rossi PAQ, Fukuda DH, Rossi FE. The impact of acute and chronic resistance training on appetite and energy intake: A scoping review examining resistance exercise and comparisons with other exercise modalities. Appetite. 2024;193:107155. doi:10.1016/j.appet.2023.107155 https://pubmed.ncbi.nlm.nih.gov/38081545/
Hubner S, Boron JB, Koehler K. The Effects of Exercise on Appetite in Older Adults: A Systematic Review and Meta-Analysis. Front Nutr. 2021;8:734267. Published 2021 Nov 18. doi:10.3389/fnut.2021.734267 https://pubmed.ncbi.nlm.nih.gov/34869516/
Dorling J, Broom DR, Burns SF, et al. Acute and Chronic Effects of Exercise on Appetite, Energy Intake, and Appetite-Related Hormones: The Modulating Effect of Adiposity, Sex, and Habitual Physical Activity. Nutrients. 2018;10(9):1140. Published 2018 Aug 22. doi:10.3390/nu10091140 https://pubmed.ncbi.nlm.nih.gov/30131457/
Douglas JA, King JA, Clayton DJ, et al. Acute effects of exercise on appetite, ad libitum energy intake and appetite-regulatory hormones in lean and overweight/obese men and women. Int J Obes (Lond). 2017;41(12):1737-1744. doi:10.1038/ijo.2017.181 https://pubmed.ncbi.nlm.nih.gov/28769121/
Stensel D. Exercise, appetite and appetite-regulating hormones: implications for food intake and weight control. Ann Nutr Metab. 2010;57 Suppl 2:36-42. doi:10.1159/000322702 https://pubmed.ncbi.nlm.nih.gov/21346335/
Thackray AE, Deighton K, King JA, Stensel DJ. Exercise, Appetite and Weight Control: Are There Differences between Men and Women?. Nutrients. 2016;8(9):583. Published 2016 Sep 21. doi:10.3390/nu8090583 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037567/
Caruso L, Zauli E, Vaccarezza M. Physical Exercise and Appetite Regulation: New Insights. Biomolecules. 2023;13(8):1170. Published 2023 Jul 27. doi:10.3390/biom13081170 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10452291/
Martins C, Morgan L, Truby H. A review of the effects of exercise on appetite regulation: an obesity perspective. Int J Obes (Lond). 2008;32(9):1337-1347. doi:10.1038/ijo.2008.98 https://pubmed.ncbi.nlm.nih.gov/18607378/
Hargreaves M, Spriet LL. Exercise Metabolism: Fuels for the Fire. Cold Spring Harb Perspect Med. 2018;8(8):a029744. Published 2018 Aug 1. doi:10.1101/cshperspect.a029744 https://pubmed.ncbi.nlm.nih.gov/28533314/
Hargreaves M, Spriet LL. Skeletal muscle energy metabolism during exercise [published correction appears in Nat Metab. 2020 Sep 10;:]. Nat Metab. 2020;2(9):817-828. doi:10.1038/s42255-020-0251-4 https://pubmed.ncbi.nlm.nih.gov/32747792/
Spriet LL, Peters SJ. Influence of diet on the metabolic responses to exercise. Proc Nutr Soc. 1998;57(1):25-33. doi:10.1079/pns19980006 https://pubmed.ncbi.nlm.nih.gov/9571705/
Beck KL, Thomson JS, Swift RJ, von Hurst PR. Role of nutrition in performance enhancement and postexercise recovery. Open Access J Sports Med. 2015;6:259-267. Published 2015 Aug 11. doi:10.2147/OAJSM.S33605 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4540168/
Mata F, Valenzuela PL, Gimenez J, et al. Carbohydrate Availability and Physical Performance: Physiological Overview and Practical Recommendations. Nutrients. 2019;11(5):1084. Published 2019 May 16. doi:10.3390/nu11051084 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6566225/
Erlenbusch M, Haub M, Munoz K, MacConnie S, Stillwell B. Effect of high-fat or high-carbohydrate diets on endurance exercise: a meta-analysis. Int J Sport Nutr Exerc Metab. 2005;15(1):1-14. doi:10.1123/ijsnem.15.1.1 https://pubmed.ncbi.nlm.nih.gov/15902985/
Maughan RJ, Greenhaff PL, Leiper JB, Ball D, Lambert CP, Gleeson M. Diet composition and the performance of high-intensity exercise. J Sports Sci. 1997;15(3):265-275. doi:10.1080/026404197367272 https://pubmed.ncbi.nlm.nih.gov/9232552/
Kanter M. High-Quality Carbohydrates and Physical Performance: Expert Panel Report. Nutr Today. 2018;53(1):35-39. doi:10.1097/NT.0000000000000238 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5794245/
Rothschild JA, Kilding AE, Plews DJ. What Should I Eat before Exercise? Pre-Exercise Nutrition and the Response to Endurance Exercise: Current Prospective and Future Directions. Nutrients. 2020;12(11):3473. Published 2020 Nov 12. doi:10.3390/nu12113473 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7696145/
Neufer PD, Costill DL, Flynn MG, Kirwan JP, Mitchell JB, Houmard J. Improvements in exercise performance: effects of carbohydrate feedings and diet. J Appl Physiol (1985). 1987;62(3):983-988. doi:10.1152/jappl.1987.62.3.983 https://pubmed.ncbi.nlm.nih.gov/3571097/
Fleming J, Sharman MJ, Avery NG, et al. Endurance capacity and high-intensity exercise performance responses to a high fat diet. Int J Sport Nutr Exerc Metab. 2003;13(4):466-478. doi:10.1123/ijsnem.13.4.466 https://pubmed.ncbi.nlm.nih.gov/14967870/
Ribeiro AS, Nunes JP, Schoenfeld BJ, Aguiar AF, Cyrino ES. Effects of Different Dietary Energy Intake Following Resistance Training on Muscle Mass and Body Fat in Bodybuilders: A Pilot Study. J Hum Kinet. 2019;70:125-134. Published 2019 Nov 30. doi:10.2478/hukin-2019-0038 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6942464/
Cholewa JM, Newmire DE, Zanchi NE. Carbohydrate restriction: Friend or foe of resistance-based exercise performance?. Nutrition. 2019;60:136-146. doi:10.1016/j.nut.2018.09.026 https://pubmed.ncbi.nlm.nih.gov/30586657/
Ellerbroek A, Peacock CA, Orris S, et al. The effects of heavy resistance training and a high protein diet (3.4g/kg/d) on body composition, exercise performance and indices of health in resistance-trained individuals – a follow-up investigation. J Int Soc Sports Nutr. 2015;12(Suppl 1):P37. Published 2015 Sep 21. doi:10.1186/1550-2783-12-S1-P37 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4594935/
Bosse JD, Dixon BM. Dietary protein to maximize resistance training: a review and examination of protein spread and change theories. J Int Soc Sports Nutr. 2012;9(1):42. Published 2012 Sep 8. doi:10.1186/1550-2783-9-42 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3518828/
Helms ER, Zinn C, Rowlands DS, Brown SR. A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: a case for higher intakes. Int J Sport Nutr Exerc Metab. 2014;24(2):127-138. doi:10.1123/ijsnem.2013-0054 https://pubmed.ncbi.nlm.nih.gov/24092765/
Parr EB, Heilbronn LK, Hawley JA. A Time to Eat and a Time to Exercise. Exerc Sport Sci Rev. 2020;48(1):4-10. doi:10.1249/JES.0000000000000207 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6948807/
Matsumoto M, Narumi-Hyakutake A, Kakutani Y, et al. Evaluation of protein requirements using the indicator amino acid oxidation method: a scoping review. J Nutr. 2023;153(12):3472-3489. doi:10.1016/j.tjnut.2023.07.015 https://pubmed.ncbi.nlm.nih.gov/37573015/
Ruiz-Castellano C, Espinar S, Contreras C, Mata F, Aragon AA, Martínez-Sanz JM. Achieving an Optimal Fat Loss Phase in Resistance-Trained Athletes: A Narrative Review. Nutrients. 2021;13(9):3255. Published 2021 Sep 18. doi:10.3390/nu13093255 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8471721/
Bandegan A, Courtney-Martin G, Rafii M, Pencharz PB, Lemon PWR. Indicator amino acid oxidation protein requirement estimate in endurance-trained men 24 h postexercise exceeds both the EAR and current athlete guidelines. Am J Physiol Endocrinol Metab. 2019;316(5):E741-E748. doi:10.1152/ajpendo.00174.2018 https://pubmed.ncbi.nlm.nih.gov/30779631/
Mazzulla M, Abou Sawan S, Williamson E, et al. Protein Intake to Maximize Whole-Body Anabolism during Postexercise Recovery in Resistance-Trained Men with High Habitual Intakes is Severalfold Greater than the Current Recommended Dietary Allowance. J Nutr. 2020;150(3):505-511. doi:10.1093/jn/nxz249 https://pubmed.ncbi.nlm.nih.gov/31618421/
Wolfe RR, Kim IY, Park S, Ferrando A. Tracing metabolic flux to assess optimal dietary protein and amino acid consumption. Exp Mol Med. 2022;54(9):1323-1331. doi:10.1038/s12276-022-00817-w https://pubmed.ncbi.nlm.nih.gov/36075948/
Dolezal BA, Neufeld EV, Boland DM, Martin JL, Cooper CB. Interrelationship between Sleep and Exercise: A Systematic Review [published correction appears in Adv Prev Med. 2017;2017:5979510]. Adv Prev Med. 2017;2017:1364387. doi:10.1155/2017/1364387 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5385214/
Banno M, Harada Y, Taniguchi M, et al. Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ. 2018;6:e5172. Published 2018 Jul 11. doi:10.7717/peerj.5172 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6045928/
Alnawwar MA, Alraddadi MI, Algethmi RA, Salem GA, Salem MA, Alharbi AA. The Effect of Physical Activity on Sleep Quality and Sleep Disorder: A Systematic Review. Cureus. 2023;15(8):e43595. Published 2023 Aug 16. doi:10.7759/cureus.43595 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10503965/
Xie Y, Liu S, Chen XJ, Yu HH, Yang Y, Wang W. Effects of Exercise on Sleep Quality and Insomnia in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Psychiatry. 2021;12:664499. Published 2021 Jun 7. doi:10.3389/fpsyt.2021.664499 https://pubmed.ncbi.nlm.nih.gov/34163383/
Park I, Díaz J, Matsumoto S, et al. Exercise improves the quality of slow-wave sleep by increasing slow-wave stability. Sci Rep. 2021;11(1):4410. Published 2021 Feb 24. doi:10.1038/s41598-021-83817-6 https://pubmed.ncbi.nlm.nih.gov/33627708/
Bjornsdottir E, Thorarinsdottir EH, Lindberg E, et al. Association between physical activity over a 10-year period and current insomnia symptoms, sleep duration and daytime sleepiness: a European population-based study. BMJ Open. 2024;14(3):e067197. Published 2024 Mar 26. doi:10.1136/bmjopen-2022-067197 https://pubmed.ncbi.nlm.nih.gov/38531588/
Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427-449. doi:10.1007/s10865-015-9617-6 https://pubmed.ncbi.nlm.nih.gov/25596964/
Lins-Filho, O., Lyra, M.J., Kline, C.E. (2022). Exercise and Sleep. In: Frange, C., Coelho, F.M.S. (eds) Sleep Medicine and Physical Therapy. Springer, Cham. https://doi.org/10.1007/978-3-030-85074-6_29
Yue T, Liu X, Gao Q, Wang Y. Different Intensities of Evening Exercise on Sleep in Healthy Adults: A Systematic Review and Network Meta-Analysis. Nat Sci Sleep. 2022;14:2157-2177. Published 2022 Dec 14. doi:10.2147/NSS.S388863 https://pubmed.ncbi.nlm.nih.gov/36540196/
Abd El-Kader SM, Al-Jiffri OH. Aerobic exercise affects sleep, psychological wellbeing and immune system parameters among subjects with chronic primary insomnia. Afr Health Sci. 2020;20(4):1761-1769. doi:10.4314/ahs.v20i4.29 https://pubmed.ncbi.nlm.nih.gov/34394237/
Uchida S, Shioda K, Morita Y, Kubota C, Ganeko M, Takeda N. Exercise effects on sleep physiology. Front Neurol. 2012;3:48. Published 2012 Apr 2. doi:10.3389/fneur.2012.00048 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3317043/
Brand S, Gerber M, Beck J, Hatzinger M, Pühse U, Holsboer-Trachsler E. High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: a comparison of athletes and controls. J Adolesc Health. 2010;46(2):133-141. doi:10.1016/j.jadohealth.2009.06.018 https://pubmed.ncbi.nlm.nih.gov/20113919/
Zapalac K, Miller M, Champagne FA, Schnyer DM, Baird B. The effects of physical activity on sleep architecture and mood in naturalistic environments. Sci Rep. 2024;14(1):5637. Published 2024 Mar 7. doi:10.1038/s41598-024-56332-7 https://pubmed.ncbi.nlm.nih.gov/38454070/
Burgess VN, Antonio J, Bland HW, Wagner R, Tartar JL, Melton BF. The Effect of Timing and Type of Exercise on the Quality of Sleep in Trained Individuals. Int J Exerc Sci. 2020;13(7):837-858. Published 2020 Aug 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7449340/
Fullagar HH, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161-186. doi:10.1007/s40279-014-0260-0 https://pubmed.ncbi.nlm.nih.gov/25315456/
Charest J, Grandner MA. Sleep and Athletic Performance: Impacts on Physical Performance, Mental Performance, Injury Risk and Recovery, and Mental Health. Sleep Med Clin. 2020;15(1):41-57. doi:10.1016/j.jsmc.2019.11.005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9960533/
Cunha LA, Costa JA, Marques EA, Brito J, Lastella M, Figueiredo P. The Impact of Sleep Interventions on Athletic Performance: A Systematic Review. Sports Med Open. 2023;9(1):58. Published 2023 Jul 18. doi:10.1186/s40798-023-00599-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10354314/
Craven J, McCartney D, Desbrow B, et al. Effects of Acute Sleep Loss on Physical Performance: A Systematic and Meta-Analytical Review. Sports Med. 2022;52(11):2669-2690. doi:10.1007/s40279-022-01706-y https://pubmed.ncbi.nlm.nih.gov/35708888/
Saidi O, Colin E, Rance M, Doré E, Pereira B, Duché P. Effect of morning versus evening exercise training on sleep, physical activity, fitness, fatigue and quality of life in overweight and obese adults. Chronobiol Int. 2021;38(11):1537-1548. doi:10.1080/07420528.2021.1935988 https://pubmed.ncbi.nlm.nih.gov/34128447/
Kirschen GW, Jones JJ, Hale L. The Impact of Sleep Duration on Performance Among Competitive Athletes: A Systematic Literature Review. Clin J Sport Med. 2020;30(5):503-512. doi:10.1097/JSM.0000000000000622 https://pubmed.ncbi.nlm.nih.gov/29944513/
Coleman EA, Goodwin JA, Kennedy R, et al. Effects of exercise on fatigue, sleep, and performance: a randomized trial. Oncol Nurs Forum. 2012;39(5):468-477. doi:10.1188/12.ONF.468-477 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6417884/
Fullagar HHK, Vincent GE, McCullough M, Halson S, Fowler P. Sleep and Sport Performance. J Clin Neurophysiol. 2023;40(5):408-416. doi:10.1097/WNP.0000000000000638 https://pubmed.ncbi.nlm.nih.gov/36930212/
Halson SL, Juliff LE. Sleep, sport, and the brain. Prog Brain Res. 2017;234:13-31. doi:10.1016/bs.pbr.2017.06.006 https://pubmed.ncbi.nlm.nih.gov/29031461/
Knufinke M, Nieuwenhuys A, Maase K, et al. Effects of Natural Between-Days Variation in Sleep on Elite Athletes’ Psychomotor Vigilance and Sport-Specific Measures of Performance. J Sports Sci Med. 2018;17(4):515-524. Published 2018 Nov 20. https://pubmed.ncbi.nlm.nih.gov/30479518/
Fullagar HH, Duffield R, Skorski S, Coutts AJ, Julian R, Meyer T. Sleep and Recovery in Team Sport: Current Sleep-Related Issues Facing Professional Team-Sport Athletes. Int J Sports Physiol Perform. 2015;10(8):950-957. doi:10.1123/ijspp.2014-0565 https://pubmed.ncbi.nlm.nih.gov/25756787/
Nowacka-Chmielewska M, Grabowska K, Grabowski M, Meybohm P, Burek M, Małecki A. Running from Stress: Neurobiological Mechanisms of Exercise-Induced Stress Resilience. Int J Mol Sci. 2022;23(21):13348. Published 2022 Nov 1. doi:10.3390/ijms232113348 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9654650/
Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81-121. doi:10.1007/s40279-013-0090-5 https://pubmed.ncbi.nlm.nih.gov/24030837/
Childs E, de Wit H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front Physiol. 2014;5:161. Published 2014 May 1. doi:10.3389/fphys.2014.00161 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4013452/
Schultchen D, Reichenberger J, Mittl T, et al. Bidirectional relationship of stress and affect with physical activity and healthy eating. Br J Health Psychol. 2019;24(2):315-333. doi:10.1111/bjhp.12355 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6767465/
Leuchter RK, Stuber ML, McDonald AL, Croymans DM. Relationship between exercise intensity and stress levels among U.S. medical students. Med Educ Online. 2022;27(1):2027651. doi:10.1080/10872981.2022.2027651 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8786247/
Elliott LD, Wilson OWA, Holland KE, Bopp M. Using Exercise as a Stress Management Technique During the COVID-19 Pandemic: The Differences Between Men and Women in College. Int J Exerc Sci. 2021;14(5):1234-1246. Published 2021 Oct 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8758158/
Worthen M, Cash E. Stress Management. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 14, 2023. https://pubmed.ncbi.nlm.nih.gov/30020672/
Churchill R, Teo K, Kervin L, Riadi I, Cosco TD. Exercise interventions for stress reduction in older adult populations: a systematic review of randomized controlled trials. Health Psychol Behav Med. 2022;10(1):913-934. Published 2022 Sep 25. doi:10.1080/21642850.2022.2125874 https://pubmed.ncbi.nlm.nih.gov/36186892/
Blumenthal JA, Sherwood A, Babyak MA, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease: a randomized controlled trial. JAMA. 2005;293(13):1626-1634. doi:10.1001/jama.293.13.1626 https://pubmed.ncbi.nlm.nih.gov/15811982/
Caplin A, Chen FS, Beauchamp MR, Puterman E. The effects of exercise intensity on the cortisol response to a subsequent acute psychosocial stressor. Psychoneuroendocrinology. 2021;131:105336. doi:10.1016/j.psyneuen.2021.105336 https://pubmed.ncbi.nlm.nih.gov/34175558/
Basso JC, Suzuki WA. The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review. Brain Plast. 2017;2(2):127-152. Published 2017 Mar 28. doi:10.3233/BPL-160040 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5928534/
Koo KM, Kim CJ. The effect of the type of physical activity on the perceived stress level in people with activity limitations. J Exerc Rehabil. 2018;14(3):361-366. Published 2018 Jun 30. doi:10.12965/jer.1836164.082 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6028212/
Furrer R, Hawley JA, Handschin C. The molecular athlete: exercise physiology from mechanisms to medals. Physiol Rev. 2023;103(3):1693-1787. doi:10.1152/physrev.00017.2022 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10110736/
Noto RE, Leavitt L, Edens MA. Physiology, Muscle. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 1, 2023. https://pubmed.ncbi.nlm.nih.gov/30335291/
Knuttgen HG. Strength training and aerobic exercise: comparison and contrast. J Strength Cond Res. 2007;21(3):973-978. doi:10.1519/R-505011.1 https://pubmed.ncbi.nlm.nih.gov/17685726/
Hughes DC, Ellefsen S, Baar K. Adaptations to Endurance and Strength Training. Cold Spring Harb Perspect Med. 2018;8(6):a029769. Published 2018 Jun 1. doi:10.1101/cshperspect.a029769 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5983157/
Stone MH, Hornsby WG, Suarez DG, Duca M, Pierce KC. Training Specificity for Athletes: Emphasis on Strength-Power Training: A Narrative Review. J Funct Morphol Kinesiol. 2022;7(4):102. Published 2022 Nov 16. doi:10.3390/jfmk7040102 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9680266/
Suchomel TJ, Nimphius S, Bellon CR, Stone MH. The Importance of Muscular Strength: Training Considerations. Sports Med. 2018;48(4):765-785. doi:10.1007/s40279-018-0862-z https://pubmed.ncbi.nlm.nih.gov/29372481/
Reggiani C, Schiaffino S. Muscle hypertrophy and muscle strength: dependent or independent variables? A provocative review. Eur J Transl Myol. 2020;30(3):9311. Published 2020 Sep 9. doi:10.4081/ejtm.2020.9311 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7582410/
Wilson JM, Loenneke JP, Jo E, Wilson GJ, Zourdos MC, Kim JS. The effects of endurance, strength, and power training on muscle fiber type shifting. J Strength Cond Res. 2012;26(6):1724-1729. doi:10.1519/JSC.0b013e318234eb6f https://pubmed.ncbi.nlm.nih.gov/21912291/
Buckner SL, Jessee MB, Mouser JG, et al. The Basics of Training for Muscle Size and Strength: A Brief Review on the Theory. Med Sci Sports Exerc. 2020;52(3):645-653. doi:10.1249/MSS.0000000000002171 https://pubmed.ncbi.nlm.nih.gov/31652235/
Krzysztofik M, Wilk M, Wojdała G, Gołaś A. Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods. Int J Environ Res Public Health. 2019;16(24):4897. Published 2019 Dec 4. doi:10.3390/ijerph16244897 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950543/
Chen HT, Chung YC, Chen YJ, Ho SY, Wu HJ. Effects of Different Types of Exercise on Body Composition, Muscle Strength, and IGF-1 in the Elderly with Sarcopenic Obesity. J Am Geriatr Soc. 2017;65(4):827-832. doi:10.1111/jgs.14722 https://pubmed.ncbi.nlm.nih.gov/28205203/
van Baak MA, Pramono A, Battista F, et al. Effect of different types of regular exercise on physical fitness in adults with overweight or obesity: Systematic review and meta-analyses. Obes Rev. 2021;22 Suppl 4(Suppl 4):e13239. doi:10.1111/obr.13239 https://pubmed.ncbi.nlm.nih.gov/33939229/
Plotkin DL, Roberts MD, Haun CT, Schoenfeld BJ. Muscle Fiber Type Transitions with Exercise Training: Shifting Perspectives. Sports (Basel). 2021;9(9):127. Published 2021 Sep 10. doi:10.3390/sports9090127 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8473039/
Schoenfeld BJ, Grgic J, Van Every DW, Plotkin DL. Loading Recommendations for Muscle Strength, Hypertrophy, and Local Endurance: A Re-Examination of the Repetition Continuum. Sports (Basel). 2021;9(2):32. Published 2021 Feb 22. doi:10.3390/sports9020032 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7927075/
Ralston GW, Kilgore L, Wyatt FB, Buchan D, Baker JS. Weekly Training Frequency Effects on Strength Gain: A Meta-Analysis. Sports Med Open. 2018;4(1):36. Published 2018 Aug 3. doi:10.1186/s40798-018-0149-9 https://pubmed.ncbi.nlm.nih.gov/30076500/
Behm DG, Young JD, Whitten JHD, et al. Effectiveness of Traditional Strength vs. Power Training on Muscle Strength, Power and Speed with Youth: A Systematic Review and Meta-Analysis. Front Physiol. 2017;8:423. Published 2017 Jun 30. doi:10.3389/fphys.2017.00423 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5491841/
Maestroni L, Read P, Bishop C, et al. The Benefits of Strength Training on Musculoskeletal System Health: Practical Applications for Interdisciplinary Care. Sports Med. 2020;50(8):1431-1450. doi:10.1007/s40279-020-01309-5 https://pubmed.ncbi.nlm.nih.gov/32564299/
Folland JP, Williams AG. The adaptations to strength training : morphological and neurological contributions to increased strength. Sports Med. 2007;37(2):145-168. doi:10.2165/00007256-200737020-00004 https://pubmed.ncbi.nlm.nih.gov/17241104/
Iversen VM, Norum M, Schoenfeld BJ, Fimland MS. No Time to Lift? Designing Time-Efficient Training Programs for Strength and Hypertrophy: A Narrative Review. Sports Med. 2021;51(10):2079-2095. doi:10.1007/s40279-021-01490-1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449772/
Calatayud J, Vinstrup J, Jakobsen MD, et al. Importance of mind-muscle connection during progressive resistance training. Eur J Appl Physiol. 2016;116(3):527-533. doi:10.1007/s00421-015-3305-7 https://pubmed.ncbi.nlm.nih.gov/26700744/
Colquhoun RJ, Gai CM, Aguilar D, et al. Training Volume, Not Frequency, Indicative of Maximal Strength Adaptations to Resistance Training. J Strength Cond Res. 2018;32(5):1207-1213. doi:10.1519/JSC.0000000000002414 https://pubmed.ncbi.nlm.nih.gov/29324578/
Thomas MH, Burns SP. Increasing Lean Mass and Strength: A Comparison of High Frequency Strength Training to Lower Frequency Strength Training. Int J Exerc Sci. 2016;9(2):159-167. Published 2016 Apr 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836564/
Schumann M, Feuerbacher JF, Sünkeler M, et al. Compatibility of Concurrent Aerobic and Strength Training for Skeletal Muscle Size and Function: An Updated Systematic Review and Meta-Analysis. Sports Med. 2022;52(3):601-612. doi:10.1007/s40279-021-01587-7 https://pubmed.ncbi.nlm.nih.gov/34757594/
de Santana DA, Castro A, Cavaglieri CR. Strength Training Volume to Increase Muscle Mass Responsiveness in Older Individuals: Weekly Sets Based Approach. Front Physiol. 2021;12:759677. Published 2021 Sep 30. doi:10.3389/fphys.2021.759677 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8514686/
Balshaw TG, Maden-Wilkinson TM, Massey GJ, Folland JP. The Human Muscle Size and Strength Relationship: Effects of Architecture, Muscle Force, and Measurement Location. Med Sci Sports Exerc. 2021;53(10):2140-2151. doi:10.1249/MSS.0000000000002691 https://pubmed.ncbi.nlm.nih.gov/33935234/
Bernárdez-Vázquez R, Raya-González J, Castillo D, Beato M. Resistance Training Variables for Optimization of Muscle Hypertrophy: An Umbrella Review. Front Sports Act Living. 2022;4:949021. Published 2022 Jul 4. doi:10.3389/fspor.2022.949021 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9302196/
Heidel KA, Novak ZJ, Dankel SJ. Machines and free weight exercises: a systematic review and meta-analysis comparing changes in muscle size, strength, and power. J Sports Med Phys Fitness. 2022;62(8):1061-1070. doi:10.23736/S0022-4707.21.12929-9 https://pubmed.ncbi.nlm.nih.gov/34609100/
Ralston GW, Kilgore L, Wyatt FB, Baker JS. The Effect of Weekly Set Volume on Strength Gain: A Meta-Analysis. Sports Med. 2017;47(12):2585-2601. doi:10.1007/s40279-017-0762-7 https://pubmed.ncbi.nlm.nih.gov/28755103/
Suchomel TJ, Nimphius S, Bellon CR, Hornsby WG, Stone MH. Training for Muscular Strength: Methods for Monitoring and Adjusting Training Intensity. Sports Med. 2021;51(10):2051-2066. doi:10.1007/s40279-021-01488-9 https://pubmed.ncbi.nlm.nih.gov/34101157/
Androulakis-Korakakis P, Michalopoulos N, Fisher JP, et al. The Minimum Effective Training Dose Required for 1RM Strength in Powerlifters. Front Sports Act Living. 2021;3:713655. Published 2021 Aug 30. doi:10.3389/fspor.2021.713655 https://pubmed.ncbi.nlm.nih.gov/34527944/
Helms ER, Kwan K, Sousa CA, Cronin JB, Storey AG, Zourdos MC. Methods for Regulating and Monitoring Resistance Training. J Hum Kinet. 2020;74:23-42. Published 2020 Aug 31. doi:10.2478/hukin-2020-0011 https://pubmed.ncbi.nlm.nih.gov/33312273/
Ruple BA, Plotkin DL, Smith MA, et al. The effects of resistance training to near failure on strength, hypertrophy, and motor unit adaptations in previously trained adults. Physiol Rep. 2023;11(9):e15679. doi:10.14814/phy2.15679 https://pubmed.ncbi.nlm.nih.gov/37144554/
Zourdos MC, Klemp A, Dolan C, et al. Novel Resistance Training-Specific Rating of Perceived Exertion Scale Measuring Repetitions in Reserve. J Strength Cond Res. 2016;30(1):267-275. doi:10.1519/JSC.0000000000001049 https://pubmed.ncbi.nlm.nih.gov/26049792/
Mangine GT, Serafini PR, Stratton MT, Olmos AA, VanDusseldorp TA, Feito Y. Effect of the Repetitions-In-Reserve Resistance Training Strategy on Bench Press Performance, Perceived Effort, and Recovery in Trained Men. J Strength Cond Res. 2022;36(1):1-9. doi:10.1519/JSC.0000000000004158 https://pubmed.ncbi.nlm.nih.gov/34941608/
Mansfield SK, Peiffer JJ, Hughes LJ, Scott BR. Estimating Repetitions in Reserve for Resistance Exercise: An Analysis of Factors Which Impact on Prediction Accuracy. J Strength Cond Res. Published online August 31, 2020. doi:10.1519/JSC.0000000000003779 https://pubmed.ncbi.nlm.nih.gov/32881842/
Schoenfeld BJ. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. 2010;24(10):2857-2872. doi:10.1519/JSC.0b013e3181e840f3 https://pubmed.ncbi.nlm.nih.gov/20847704/
Baz-Valle E, Balsalobre-Fernández C, Alix-Fages C, Santos-Concejero J. A Systematic Review of The Effects of Different Resistance Training Volumes on Muscle Hypertrophy. J Hum Kinet. 2022;81:199-210. Published 2022 Feb 10. doi:10.2478/hukin-2022-0017 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8884877/
Warneke K, Lohmann LH, Lima CD, et al. Physiology of Stretch-Mediated Hypertrophy and Strength Increases: A Narrative Review. Sports Med. 2023;53(11):2055-2075. doi:10.1007/s40279-023-01898-x https://pubmed.ncbi.nlm.nih.gov/37556026/
Lawson D, Vann C, Schoenfeld BJ, Haun C. Beyond Mechanical Tension: A Review of Resistance Exercise-Induced Lactate Responses & Muscle Hypertrophy. J Funct Morphol Kinesiol. 2022;7(4):81. Published 2022 Oct 4. doi:10.3390/jfmk7040081 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9590033/
de Freitas MC, Gerosa-Neto J, Zanchi NE, Lira FS, Rossi FE. Role of metabolic stress for enhancing muscle adaptations: Practical applications. World J Methodol. 2017;7(2):46-54. Published 2017 Jun 26. doi:10.5662/wjm.v7.i2.46 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5489423/
Beattie K, Kenny IC, Lyons M, Carson BP. The effect of strength training on performance in endurance athletes. Sports Med. 2014;44(6):845-865. doi:10.1007/s40279-014-0157-y https://pubmed.ncbi.nlm.nih.gov/24532151/
Hottenrott K, Ludyga S, Schulze S. Effects of high intensity training and continuous endurance training on aerobic capacity and body composition in recreationally active runners. J Sports Sci Med. 2012;11(3):483-488. Published 2012 Sep 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737930/
Jamka M, Mądry E, Krzyżanowska-Jankowska P, et al. The effect of endurance and endurance-strength training on body composition and cardiometabolic markers in abdominally obese women: a randomised trial. Sci Rep. 2021;11(1):12339. Published 2021 Jun 11. doi:10.1038/s41598-021-90526-7 https://pubmed.ncbi.nlm.nih.gov/34117276/
Doma K, Deakin GB, Schumann M, Bentley DJ. Training Considerations for Optimising Endurance Development: An Alternate Concurrent Training Perspective. Sports Med. 2019;49(5):669-682. doi:10.1007/s40279-019-01072-2 https://pubmed.ncbi.nlm.nih.gov/30847824/
Düking P, Zinner C, Trabelsi K, et al. Monitoring and adapting endurance training on the basis of heart rate variability monitored by wearable technologies: A systematic review with meta-analysis. J Sci Med Sport. 2021;24(11):1180-1192. doi:10.1016/j.jsams.2021.04.012 https://pubmed.ncbi.nlm.nih.gov/34489178/
Milanović Z, Sporiš G, Weston M. Effectiveness of High-Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta-Analysis of Controlled Trials. Sports Med. 2015;45(10):1469-1481. doi:10.1007/s40279-015-0365-0 https://pubmed.ncbi.nlm.nih.gov/26243014/
Herzig D, Asatryan B, Brugger N, Eser P, Wilhelm M. The Association Between Endurance Training and Heart Rate Variability: The Confounding Role of Heart Rate. Front Physiol. 2018;9:756. Published 2018 Jun 19. doi:10.3389/fphys.2018.00756 https://pubmed.ncbi.nlm.nih.gov/29971016/
Laursen PB, Shing CM, Peake JM, Coombes JS, Jenkins DG. Interval training program optimization in highly trained endurance cyclists. Med Sci Sports Exerc. 2002;34(11):1801-1807. doi:10.1097/00005768-200211000-00017 https://pubmed.ncbi.nlm.nih.gov/12439086/
Mrówczyński W. Health Benefits of Endurance Training: Implications of the Brain-Derived Neurotrophic Factor-A Systematic Review. Neural Plast. 2019;2019:5413067. Published 2019 Jun 24. doi:10.1155/2019/5413067 https://pubmed.ncbi.nlm.nih.gov/31341469/
Cadore EL, Pinto RS, Bottaro M, Izquierdo M. Strength and endurance training prescription in healthy and frail elderly. Aging Dis. 2014;5(3):183-195. Published 2014 Jun 1. doi:10.14336/AD.2014.0500183 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4037310/
Baquet G, van Praagh E, Berthoin S. Endurance training and aerobic fitness in young people. Sports Med. 2003;33(15):1127-1143. doi:10.2165/00007256-200333150-00004 https://pubmed.ncbi.nlm.nih.gov/14719981/
Vesterinen V, Nummela A, Heikura I, et al. Individual Endurance Training Prescription with Heart Rate Variability. Med Sci Sports Exerc. 2016;48(7):1347-1354. doi:10.1249/MSS.0000000000000910 https://pubmed.ncbi.nlm.nih.gov/26909534/
Wilson JM, Marin PJ, Rhea MR, Wilson SM, Loenneke JP, Anderson JC. Concurrent training: a meta-analysis examining interference of aerobic and resistance exercises. J Strength Cond Res. 2012;26(8):2293-2307. doi:10.1519/JSC.0b013e31823a3e2d https://pubmed.ncbi.nlm.nih.gov/22002517/
Tanaka H, Swensen T. Impact of resistance training on endurance performance. A new form of cross-training?. Sports Med. 1998;25(3):191-200. doi:10.2165/00007256-199825030-00005 https://pubmed.ncbi.nlm.nih.gov/9554029/
Foster C, Farland CV, Guidotti F, et al. The Effects of High Intensity Interval Training vs Steady State Training on Aerobic and Anaerobic Capacity. J Sports Sci Med. 2015;14(4):747-755. Published 2015 Nov 24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4657417/
Khanfir MA, Awicha HB, Masmoudi L, et al. Effects of Different Low-Intensity Exercise Types on Duration, Energy Expenditure and Perceived Exertion in Obese Individuals. Int J Environ Res Public Health. 2022;19(8):4893. Published 2022 Apr 18. doi:10.3390/ijerph19084893 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9032643/
Bishop DJ, Botella J, Genders AJ, et al. High-Intensity Exercise and Mitochondrial Biogenesis: Current Controversies and Future Research Directions. Physiology (Bethesda). 2019;34(1):56-70. doi:10.1152/physiol.00038.2018 https://pubmed.ncbi.nlm.nih.gov/30540234/
Huertas JR, Casuso RA, Agustín PH, Cogliati S. Stay Fit, Stay Young: Mitochondria in Movement: The Role of Exercise in the New Mitochondrial Paradigm [published correction appears in Oxid Med Cell Longev. 2021 Jan 18;2021:9274841]. Oxid Med Cell Longev. 2019;2019:7058350. Published 2019 Jun 19. doi:10.1155/2019/7058350 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6607712/
Sorriento D, Di Vaia E, Iaccarino G. Physical Exercise: A Novel Tool to Protect Mitochondrial Health. Front Physiol. 2021;12:660068. Published 2021 Apr 27. doi:10.3389/fphys.2021.660068 https://pubmed.ncbi.nlm.nih.gov/33986694/
Oliveira AN, Richards BJ, Slavin M, Hood DA. Exercise Is Muscle Mitochondrial Medicine. Exerc Sport Sci Rev. 2021;49(2):67-76. doi:10.1249/JES.0000000000000250 https://pubmed.ncbi.nlm.nih.gov/33720909/
Memme JM, Erlich AT, Phukan G, Hood DA. Exercise and mitochondrial health. J Physiol. 2021;599(3):803-817. doi:10.1113/JP278853 https://pubmed.ncbi.nlm.nih.gov/31674658/
Roberts FL, Markby GR. New Insights into Molecular Mechanisms Mediating Adaptation to Exercise; A Review Focusing on Mitochondrial Biogenesis, Mitochondrial Function, Mitophagy and Autophagy. Cells. 2021;10(10):2639. Published 2021 Oct 2. doi:10.3390/cells10102639 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8533934/
Hood DA. Mechanisms of exercise-induced mitochondrial biogenesis in skeletal muscle. Appl Physiol Nutr Metab. 2009;34(3):465-472. doi:10.1139/H09-045 https://pubmed.ncbi.nlm.nih.gov/19448716/
Popov LD. Mitochondrial biogenesis: An update. J Cell Mol Med. 2020;24(9):4892-4899. doi:10.1111/jcmm.15194 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7205802/
Steiner JL, Murphy EA, McClellan JL, Carmichael MD, Davis JM. Exercise training increases mitochondrial biogenesis in the brain. J Appl Physiol (1985). 2011;111(4):1066-1071. doi:10.1152/japplphysiol.00343.2011 https://pubmed.ncbi.nlm.nih.gov/21817111/
Lee D, Son JY, Ju HM, Won JH, Park SB, Yang WH. Effects of Individualized Low-Intensity Exercise and Its Duration on Recovery Ability in Adults. Healthcare (Basel). 2021;9(3):249. Published 2021 Mar 1. doi:10.3390/healthcare9030249 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7999698/
Hua LP, Brown CA, Hains SJ, Godwin M, Parlow JL. Effects of low-intensity exercise conditioning on blood pressure, heart rate, and autonomic modulation of heart rate in men and women with hypertension. Biol Res Nurs. 2009;11(2):129-143. doi:10.1177/1099800408324853 https://pubmed.ncbi.nlm.nih.gov/19150992/
Robergs RA. A critical review of the history of low- to moderate-intensity steady-state VO2 kinetics. Sports Med. 2014;44(5):641-653. doi:10.1007/s40279-014-0161-2 https://pubmed.ncbi.nlm.nih.gov/24563157/
Steele J, Plotkin D, Van Every D, et al. Slow and Steady, or Hard and Fast? A Systematic Review and Meta-Analysis of Studies Comparing Body Composition Changes between Interval Training and Moderate Intensity Continuous Training. Sports (Basel). 2021;9(11):155. Published 2021 Nov 18. doi:10.3390/sports9110155 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8619923/
Stöggl TL, Sperlich B. The training intensity distribution among well-trained and elite endurance athletes. Front Physiol. 2015;6:295. Published 2015 Oct 27. doi:10.3389/fphys.2015.00295 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621419/
Gaesser GA, Angadi SS. High-intensity interval training for health and fitness: can less be more?. J Appl Physiol (1985). 2011;111(6):1540-1541. doi:10.1152/japplphysiol.01237.2011 https://pubmed.ncbi.nlm.nih.gov/21979806/
Tse AC, Wong TW, Lee PH. Effect of Low-intensity Exercise on Physical and Cognitive Health in Older Adults: a Systematic Review. Sports Med Open. 2015;1(1):37. doi:10.1186/s40798-015-0034-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612316/
Hackney AC, Hosick KP, Myer A, Rubin DA, Battaglini CL. Testosterone responses to intensive interval versus steady-state endurance exercise. J Endocrinol Invest. 2012;35(11):947-950. doi:10.1007/BF03346740 https://pubmed.ncbi.nlm.nih.gov/23310924/
Atakan MM, Li Y, Koşar ŞN, Turnagöl HH, Yan X. Evidence-Based Effects of High-Intensity Interval Training on Exercise Capacity and Health: A Review with Historical Perspective. Int J Environ Res Public Health. 2021;18(13):7201. Published 2021 Jul 5. doi:10.3390/ijerph18137201 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8294064/
Shepherd SO, Wilson OJ, Taylor AS, et al. Low-Volume High-Intensity Interval Training in a Gym Setting Improves Cardio-Metabolic and Psychological Health. PLoS One. 2015;10(9):e0139056. Published 2015 Sep 24. doi:10.1371/journal.pone.0139056 https://pubmed.ncbi.nlm.nih.gov/26402859/
Ito S. High-intensity interval training for health benefits and care of cardiac diseases – The key to an efficient exercise protocol. World J Cardiol. 2019;11(7):171-188. doi:10.4330/wjc.v11.i7.171 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6763680/
Wen D, Utesch T, Wu J, et al. Effects of different protocols of high intensity interval training for VO2max improvements in adults: A meta-analysis of randomised controlled trials. J Sci Med Sport. 2019;22(8):941-947. doi:10.1016/j.jsams.2019.01.013 https://pubmed.ncbi.nlm.nih.gov/30733142/
Gillen JB, Gibala MJ. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness?. Appl Physiol Nutr Metab. 2014;39(3):409-412. doi:10.1139/apnm-2013-0187 https://pubmed.ncbi.nlm.nih.gov/24552392/
Roy M, Williams SM, Brown RC, et al. High-Intensity Interval Training in the Real World: Outcomes from a 12-Month Intervention in Overweight Adults. Med Sci Sports Exerc. 2018;50(9):1818-1826. doi:10.1249/MSS.0000000000001642 https://pubmed.ncbi.nlm.nih.gov/29683919/
Vasconcelos BB, Protzen GV, Galliano LM, Kirk C, Del Vecchio FB. Effects of High-Intensity Interval Training in Combat Sports: A Systematic Review with Meta-Analysis. J Strength Cond Res. 2020;34(3):888-900. doi:10.1519/JSC.0000000000003255 https://pubmed.ncbi.nlm.nih.gov/31904713/
Karlsen T, Aamot IL, Haykowsky M, Rognmo Ø. High Intensity Interval Training for Maximizing Health Outcomes. Prog Cardiovasc Dis. 2017;60(1):67-77. doi:10.1016/j.pcad.2017.03.006 https://pubmed.ncbi.nlm.nih.gov/28385556/
Sousa AC, Neiva HP, Izquierdo M, Cadore EL, Alves AR, Marinho DA. Concurrent Training and Detraining: brief Review on the Effect of Exercise Intensities. Int J Sports Med. 2019;40(12):747-755. doi:10.1055/a-0975-9471 https://pubmed.ncbi.nlm.nih.gov/31476783/
Methenitis S. A Brief Review on Concurrent Training: From Laboratory to the Field. Sports (Basel). 2018;6(4):127. Published 2018 Oct 24. doi:10.3390/sports6040127 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6315763/
Berryman N, Mujika I, Bosquet L. Concurrent Training for Sports Performance: The 2 Sides of the Medal. Int J Sports Physiol Perform. 2019;14(3):279-285. doi:10.1123/ijspp.2018-0103 https://pubmed.ncbi.nlm.nih.gov/29809072/
Baar K. Using molecular biology to maximize concurrent training. Sports Med. 2014;44 Suppl 2(Suppl 2):S117-S125. doi:10.1007/s40279-014-0252-0 https://pubmed.ncbi.nlm.nih.gov/25355186/
Sousa AC, Neiva HP, Gil MH, et al. Concurrent Training and Detraining: The Influence of Different Aerobic Intensities. J Strength Cond Res. 2020;34(9):2565-2574. doi:10.1519/JSC.0000000000002874 https://pubmed.ncbi.nlm.nih.gov/30946274/
Gäbler M, Prieske O, Hortobágyi T, Granacher U. The Effects of Concurrent Strength and Endurance Training on Physical Fitness and Athletic Performance in Youth: A Systematic Review and Meta-Analysis. Front Physiol. 2018;9:1057. Published 2018 Aug 7. doi:10.3389/fphys.2018.01057 https://pubmed.ncbi.nlm.nih.gov/30131714/
Leveritt M, Abernethy PJ, Barry BK, Logan PA. Concurrent strength and endurance training. A review. Sports Med. 1999;28(6):413-427. doi:10.2165/00007256-199928060-00004 https://pubmed.ncbi.nlm.nih.gov/10623984/
Huiberts RO, Wüst RCI, van der Zwaard S. Concurrent Strength and Endurance Training: A Systematic Review and Meta-Analysis on the Impact of Sex and Training Status. Sports Med. 2024;54(2):485-503. doi:10.1007/s40279-023-01943-9 https://pubmed.ncbi.nlm.nih.gov/37847373/
Scribbans TD, Vecsey S, Hankinson PB, Foster WS, Gurd BJ. The Effect of Training Intensity on VO2max in Young Healthy Adults: A Meta-Regression and Meta-Analysis. Int J Exerc Sci. 2016;9(2):230-247. Published 2016 Apr 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836566/
Gim MN, Choi JH. The effects of weekly exercise time on VO2max and resting metabolic rate in normal adults. J Phys Ther Sci. 2016;28(4):1359-1363. doi:10.1589/jpts.28.1359 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4868243/
Gormley SE, Swain DP, High R, et al. Effect of intensity of aerobic training on VO2max. Med Sci Sports Exerc. 2008;40(7):1336-1343. doi:10.1249/MSS.0b013e31816c4839 https://pubmed.ncbi.nlm.nih.gov/18580415/
Yang Q, Li D, Xie H, et al. Effects of sprint interval training on maximal oxygen uptake in athletes: a meta-analysis. J Sports Med Phys Fitness. Published online October 5, 2021. doi:10.23736/S0022-4707.21.12815-4 https://pubmed.ncbi.nlm.nih.gov/34609099/
Bacon AP, Carter RE, Ogle EA, Joyner MJ. VO2max trainability and high intensity interval training in humans: a meta-analysis. PLoS One. 2013;8(9):e73182. Published 2013 Sep 16. doi:10.1371/journal.pone.0073182 https://pubmed.ncbi.nlm.nih.gov/24066036/
Lundby C, Montero D, Joyner M. Biology of VO2 max: looking under the physiology lamp. Acta Physiol (Oxf). 2017;220(2):218-228. doi:10.1111/apha.12827 https://pubmed.ncbi.nlm.nih.gov/27888580/
MacInnis MJ, Gibala MJ. Physiological adaptations to interval training and the role of exercise intensity. J Physiol. 2017;595(9):2915-2930. doi:10.1113/JP273196 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5407969/
Tanaka H. Effects of cross-training. Transfer of training effects on VO2max between cycling, running and swimming. Sports Med. 1994;18(5):330-339. doi:10.2165/00007256-199418050-00005 https://pubmed.ncbi.nlm.nih.gov/7871294/
Weltman A, Snead D, Seip R, et al. Percentages of maximal heart rate, heart rate reserve and VO2max for determining endurance training intensity in male runners. Int J Sports Med. 1990;11(3):218-222. doi:10.1055/s-2007-1024795 https://pubmed.ncbi.nlm.nih.gov/2373580/
Daniels JT, Yarbrough RA, Foster C. Changes in VO2 max and running performance with training. Eur J Appl Physiol Occup Physiol. 1978;39(4):249-254. doi:10.1007/BF00421448 https://pubmed.ncbi.nlm.nih.gov/710390/
Dolgener FA, Brooks WB. The effects of interval and continuous training on VO2 max and performance in the mile run. J Sports Med Phys Fitness. 1978;18(4):345-352. https://pubmed.ncbi.nlm.nih.gov/745381/
Seiler KS, Kjerland GØ. Quantifying training intensity distribution in elite endurance athletes: is there evidence for an “optimal” distribution?. Scand J Med Sci Sports. 2006;16(1):49-56. doi:10.1111/j.1600-0838.2004.00418.x https://pubmed.ncbi.nlm.nih.gov/16430681/
Ieno C, Baldassarre R, Pennacchi M, La Torre A, Bonifazi M, Piacentini MF. Monitoring Rating of Perceived Exertion Time in Zone: A Novel Method to Quantify Training Load in Elite Open-Water Swimmers?. Int J Sports Physiol Perform. 2021;16(10):1551-1555. doi:10.1123/ijspp.2020-0707 https://pubmed.ncbi.nlm.nih.gov/33761462/
Mujika I. Quantification of Training and Competition Loads in Endurance Sports: Methods and Applications. Int J Sports Physiol Perform. 2017;12(Suppl 2):S29-S217. doi:10.1123/ijspp.2016-0403 https://pubmed.ncbi.nlm.nih.gov/27918666/
Festa L, Tarperi C, Skroce K, La Torre A, Schena F. Effects of Different Training Intensity Distribution in Recreational Runners. Front Sports Act Living. 2020;1:70. Published 2020 Jan 15. doi:10.3389/fspor.2019.00070 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7739641/
Stöggl TL, Sperlich B. Editorial: Training Intensity, Volume and Recovery Distribution Among Elite and Recreational Endurance Athletes. Front Physiol. 2019;10:592. Published 2019 May 21. doi:10.3389/fphys.2019.00592 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6537749/
Casado A, González-Mohíno F, González-Ravé JM, Foster C. Training Periodization, Methods, Intensity Distribution, and Volume in Highly Trained and Elite Distance Runners: A Systematic Review. Int J Sports Physiol Perform. 2022;17(6):820-833. doi:10.1123/ijspp.2021-0435 https://pubmed.ncbi.nlm.nih.gov/35418513/
Kenneally M, Casado A, Santos-Concejero J. The Effect of Periodization and Training Intensity Distribution on Middle- and Long-Distance Running Performance: A Systematic Review. Int J Sports Physiol Perform. 2018;13(9):1114-1121. doi:10.1123/ijspp.2017-0327 https://pubmed.ncbi.nlm.nih.gov/29182410/
Kaura V, Hopkins PM. Recent advances in skeletal muscle physiology. BJA Educ. 2024;24(3):84-90. doi:10.1016/j.bjae.2023.12.003 https://pubmed.ncbi.nlm.nih.gov/38375493/
Sartori R, Romanello V, Sandri M. Mechanisms of muscle atrophy and hypertrophy: implications in health and disease. Nat Commun. 2021;12(1):330. Published 2021 Jan 12. doi:10.1038/s41467-020-20123-1 https://pubmed.ncbi.nlm.nih.gov/33436614/
Dave HD, Shook M, Varacallo M. Anatomy, Skeletal Muscle. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 28, 2023. https://pubmed.ncbi.nlm.nih.gov/30725921/
Enoka RM, Stuart DG. Neurobiology of muscle fatigue. J Appl Physiol (1985). 1992;72(5):1631-1648. doi:10.1152/jappl.1992.72.5.1631 https://pubmed.ncbi.nlm.nih.gov/1601767/
Pate RR, Durstine JL. Exercise physiology and its role in clinical sports medicine. South Med J. 2004;97(9):881-885. doi:10.1097/01.SMJ.0000140116.17258.F1 https://pubmed.ncbi.nlm.nih.gov/15455979/
Rivera-Brown AM, Frontera WR. Principles of exercise physiology: responses to acute exercise and long-term adaptations to training. PM R. 2012;4(11):797-804. doi:10.1016/j.pmrj.2012.10.007 https://pubmed.ncbi.nlm.nih.gov/23174541/
Kiens B, Richter EA, Wojtaszewski JF. Exercise physiology: from performance studies to muscle physiology and cardiovascular adaptations. J Appl Physiol (1985). 2014;117(9):943-944. doi:10.1152/japplphysiol.00874.2014 https://pubmed.ncbi.nlm.nih.gov/25277739/
Ferretti G, Fagoni N, Taboni A, Vinetti G, di Prampero PE. A century of exercise physiology: key concepts on coupling respiratory oxygen flow to muscle energy demand during exercise. Eur J Appl Physiol. 2022;122(6):1317-1365. doi:10.1007/s00421-022-04901-x https://pubmed.ncbi.nlm.nih.gov/35217911/
Pedersen BK. The Physiology of Optimizing Health with a Focus on Exercise as Medicine. Annu Rev Physiol. 2019;81:607-627. doi:10.1146/annurev-physiol-020518-114339 https://pubmed.ncbi.nlm.nih.gov/30526319/
Powers SK, Hogan MC. Advances in exercise physiology: exercise and health. J Physiol. 2021;599(3):769-770. doi:10.1113/JP281003 https://pubmed.ncbi.nlm.nih.gov/33521984/
Irvin CG. Exercise physiology. Allergy Asthma Proc. 1996;17(6):327-330. doi:10.2500/108854196778606356 https://pubmed.ncbi.nlm.nih.gov/8993725/
Wackerhage H, Schoenfeld BJ. Personalized, Evidence-Informed Training Plans and Exercise Prescriptions for Performance, Fitness and Health. Sports Med. 2021;51(9):1805-1813. doi:10.1007/s40279-021-01495-w https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8363526/
Baz-Valle E, Schoenfeld BJ, Torres-Unda J, Santos-Concejero J, Balsalobre-Fernández C. The effects of exercise variation in muscle thickness, maximal strength and motivation in resistance trained men. PLoS One. 2019;14(12):e0226989. Published 2019 Dec 27. doi:10.1371/journal.pone.0226989 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6934277/
Zabaleta-Korta A, Fernández-Peña E, Torres-Unda J, Garbisu-Hualde A, Santos-Concejero J. The role of exercise selection in regional Muscle Hypertrophy: A randomized controlled trial. J Sports Sci. 2021;39(20):2298-2304. doi:10.1080/02640414.2021.1929736 https://pubmed.ncbi.nlm.nih.gov/34743671/
Lopez P, Radaelli R, Taaffe DR, et al. Resistance Training Load Effects on Muscle Hypertrophy and Strength Gain: Systematic Review and Network Meta-analysis [published correction appears in Med Sci Sports Exerc. 2022 Feb 1;54(2):370]. Med Sci Sports Exerc. 2021;53(6):1206-1216. doi:10.1249/MSS.0000000000002585 https://pubmed.ncbi.nlm.nih.gov/33433148/
Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and Hypertrophy Adaptations Between Low- vs. High-Load Resistance Training: A Systematic Review and Meta-analysis. J Strength Cond Res. 2017;31(12):3508-3523. doi:10.1519/JSC.0000000000002200 https://pubmed.ncbi.nlm.nih.gov/28834797/
Schoenfeld BJ, Ogborn DI, Krieger JW. Effect of repetition duration during resistance training on muscle hypertrophy: a systematic review and meta-analysis. Sports Med. 2015;45(4):577-585. doi:10.1007/s40279-015-0304-0 https://pubmed.ncbi.nlm.nih.gov/25601394/
Mangine GT, Hoffman JR, Gonzalez AM, et al. The effect of training volume and intensity on improvements in muscular strength and size in resistance-trained men. Physiol Rep. 2015;3(8):e12472. doi:10.14814/phy2.12472 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4562558/
Schoenfeld BJ, Grgic J. Effects of range of motion on muscle development during resistance training interventions: A systematic review. SAGE Open Med. 2020;8:2050312120901559. Published 2020 Jan 21. doi:10.1177/2050312120901559 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6977096/
Androulakis-Korakakis P, Fisher JP, Steele J. The Minimum Effective Training Dose Required to Increase 1RM Strength in Resistance-Trained Men: A Systematic Review and Meta-Analysis. Sports Med. 2020;50(4):751-765. doi:10.1007/s40279-019-01236-0 https://pubmed.ncbi.nlm.nih.gov/31797219/
Schoenfeld BJ, Contreras B, Krieger J, et al. Resistance Training Volume Enhances Muscle Hypertrophy but Not Strength in Trained Men. Med Sci Sports Exerc. 2019;51(1):94-103. doi:10.1249/MSS.0000000000001764 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6303131/
Helms ER, Cronin J, Storey A, Zourdos MC. Application of the Repetitions in Reserve-Based Rating of Perceived Exertion Scale for Resistance Training. Strength Cond J. 2016;38(4):42-49. doi:10.1519/SSC.0000000000000218 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4961270/
Pelland JC, Robinson ZP, Remmert JF, et al. Methods for Controlling and Reporting Resistance Training Proximity to Failure: Current Issues and Future Directions. Sports Med. 2022;52(7):1461-1472. doi:10.1007/s40279-022-01667-2 https://pubmed.ncbi.nlm.nih.gov/35247203/
Campos GE, Luecke TJ, Wendeln HK, et al. Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol. 2002;88(1-2):50-60. doi:10.1007/s00421-002-0681-6 https://pubmed.ncbi.nlm.nih.gov/12436270/
Arede J, Vaz R, Gonzalo-Skok O, et al. Repetitions in reserve vs. maximum effort resistance training programs in youth female athletes. J Sports Med Phys Fitness. 2020;60(9):1231-1239. doi:10.23736/S0022-4707.20.10907-1 https://pubmed.ncbi.nlm.nih.gov/32586078/
Lovegrove S, Hughes LJ, Mansfield SK, Read PJ, Price P, Patterson SD. Repetitions in Reserve Is a Reliable Tool for Prescribing Resistance Training Load. J Strength Cond Res. 2022;36(10):2696-2700. doi:10.1519/JSC.0000000000003952 https://pubmed.ncbi.nlm.nih.gov/36135029/
Bastos V, Machado S, Teixeira DS. Feasibility and Usefulness of Repetitions-In-Reserve Scales for Selecting Exercise Intensity: A Scoping Review. Percept Mot Skills. Published online April 2, 2024. doi:10.1177/00315125241241785 https://pubmed.ncbi.nlm.nih.gov/38563729/
Morishita S, Tsubaki A, Takabayashi T, Fu JB. Relationship between the rating of perceived exertion scale and the load intensity of resistance training. Strength Cond J. 2018;40(2):94-109. doi:10.1519/SSC.0000000000000373 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5901652/
D Egan A, B Winchester J, Foster C, R McGuigan M. Using Session RPE to Monitor Different Methods of Resistance Exercise. J Sports Sci Med. 2006;5(2):289-295. Published 2006 Jun 1. https://pubmed.ncbi.nlm.nih.gov/24260002/
Day ML, McGuigan MR, Brice G, Foster C. Monitoring exercise intensity during resistance training using the session RPE scale. J Strength Cond Res. 2004;18(2):353-358. doi:10.1519/R-13113.1 https://pubmed.ncbi.nlm.nih.gov/15142026/
Morishita S, Tsubaki A, Nakamura M, Nashimoto S, Fu JB, Onishi H. Rating of perceived exertion on resistance training in elderly subjects. Expert Rev Cardiovasc Ther. 2019;17(2):135-142. doi:10.1080/14779072.2019.1561278 https://pubmed.ncbi.nlm.nih.gov/30569775/
Boxman-Zeevi Y, Schwartz H, Har-Nir I, Bordo N, Halperin I. Prescribing Intensity in Resistance Training Using Rating of Perceived Effort: A Randomized Controlled Trial. Front Physiol. 2022;13:891385. Published 2022 Apr 29. doi:10.3389/fphys.2022.891385 https://pubmed.ncbi.nlm.nih.gov/35574454/
Dias MRC, Simão R, Saavedra FJF, Buzzachera CF, Fleck S. Self-Selected Training Load and RPE During Resistance and Aerobic Training Among Recreational Exercisers. Percept Mot Skills. 2018;125(4):769-787. doi:10.1177/0031512518774461 https://pubmed.ncbi.nlm.nih.gov/29726740/
Halperin I, Emanuel A. Rating of Perceived Effort: Methodological Concerns and Future Directions. Sports Med. 2020;50(4):679-687. doi:10.1007/s40279-019-01229-z https://pubmed.ncbi.nlm.nih.gov/31745731/
Spiering BA, Clark BC, Schoenfeld BJ, Foulis SA, Pasiakos SM. Maximizing Strength: The Stimuli and Mediators of Strength Gains and Their Application to Training and Rehabilitation. J Strength Cond Res. 2023;37(4):919-929. doi:10.1519/JSC.0000000000004390 https://pubmed.ncbi.nlm.nih.gov/36580280/
Schoenfeld BJ, Pope ZK, Benik FM, et al. Longer Interset Rest Periods Enhance Muscle Strength and Hypertrophy in Resistance-Trained Men. J Strength Cond Res. 2016;30(7):1805-1812. doi:10.1519/JSC.0000000000001272 https://pubmed.ncbi.nlm.nih.gov/26605807/
Baz-Valle E, Fontes-Villalba M, Santos-Concejero J. Total Number of Sets as a Training Volume Quantification Method for Muscle Hypertrophy: A Systematic Review. J Strength Cond Res. 2021;35(3):870-878. doi:10.1519/JSC.0000000000002776 https://pubmed.ncbi.nlm.nih.gov/30063555/
Schoenfeld BJ, Ogborn DI, Vigotsky AD, Franchi MV, Krieger JW. Hypertrophic Effects of Concentric vs. Eccentric Muscle Actions: A Systematic Review and Meta-analysis. J Strength Cond Res. 2017;31(9):2599-2608. doi:10.1519/JSC.0000000000001983 https://pubmed.ncbi.nlm.nih.gov/28486337/
Schoenfeld BJ. Does exercise-induced muscle damage play a role in skeletal muscle hypertrophy?. J Strength Cond Res. 2012;26(5):1441-1453. doi:10.1519/JSC.0b013e31824f207e https://pubmed.ncbi.nlm.nih.gov/22344059/
Vaara JP, Kyröläinen H, Niemi J, et al. Associations of maximal strength and muscular endurance test scores with cardiorespiratory fitness and body composition. J Strength Cond Res. 2012;26(8):2078-2086. doi:10.1519/JSC.0b013e31823b06ff https://pubmed.ncbi.nlm.nih.gov/21997456/
Radaelli R, Fleck SJ, Leite T, et al. Dose-response of 1, 3, and 5 sets of resistance exercise on strength, local muscular endurance, and hypertrophy. J Strength Cond Res. 2015;29(5):1349-1358. doi:10.1519/JSC.0000000000000758 https://pubmed.ncbi.nlm.nih.gov/25546444/
Krieger JW. Single vs. multiple sets of resistance exercise for muscle hypertrophy: a meta-analysis. J Strength Cond Res. 2010;24(4):1150-1159. doi:10.1519/JSC.0b013e3181d4d436 https://pubmed.ncbi.nlm.nih.gov/20300012/
Pinto RS, Gomes N, Radaelli R, Botton CE, Brown LE, Bottaro M. Effect of range of motion on muscle strength and thickness. J Strength Cond Res. 2012;26(8):2140-2145. doi:10.1519/JSC.0b013e31823a3b15 https://pubmed.ncbi.nlm.nih.gov/22027847/
Kassiano W, Nunes JP, Costa B, Ribeiro AS, Schoenfeld BJ, Cyrino ES. Does Varying Resistance Exercises Promote Superior Muscle Hypertrophy and Strength Gains? A Systematic Review. J Strength Cond Res. 2022;36(6):1753-1762. doi:10.1519/JSC.0000000000004258 https://pubmed.ncbi.nlm.nih.gov/35438660/
Vieira AF, Umpierre D, Teodoro JL, et al. Effects of Resistance Training Performed to Failure or Not to Failure on Muscle Strength, Hypertrophy, and Power Output: A Systematic Review With Meta-Analysis. J Strength Cond Res. 2021;35(4):1165-1175. doi:10.1519/JSC.0000000000003936 https://pubmed.ncbi.nlm.nih.gov/33555822/
Schoenfeld BJ, Ratamess NA, Peterson MD, Contreras B, Sonmez GT, Alvar BA. Effects of different volume-equated resistance training loading strategies on muscular adaptations in well-trained men. J Strength Cond Res. 2014;28(10):2909-2918. doi:10.1519/JSC.0000000000000480 https://pubmed.ncbi.nlm.nih.gov/24714538/
Carvalho L, Junior RM, Barreira J, Schoenfeld BJ, Orazem J, Barroso R. Muscle hypertrophy and strength gains after resistance training with different volume-matched loads: a systematic review and meta-analysis. Appl Physiol Nutr Metab. 2022;47(4):357-368. doi:10.1139/apnm-2021-0515 https://pubmed.ncbi.nlm.nih.gov/35015560/
Vieira JG, Sardeli AV, Dias MR, et al. Effects of Resistance Training to Muscle Failure on Acute Fatigue: A Systematic Review and Meta-Analysis. Sports Med. 2022;52(5):1103-1125. doi:10.1007/s40279-021-01602-x https://pubmed.ncbi.nlm.nih.gov/34881412/
Grgic J, Schoenfeld BJ, Davies TB, Lazinica B, Krieger JW, Pedisic Z. Effect of Resistance Training Frequency on Gains in Muscular Strength: A Systematic Review and Meta-Analysis. Sports Med. 2018;48(5):1207-1220. doi:10.1007/s40279-018-0872-x https://pubmed.ncbi.nlm.nih.gov/29470825/
Aube D, Wadhi T, Rauch J, et al. Progressive Resistance Training Volume: Effects on Muscle Thickness, Mass, and Strength Adaptations in Resistance-Trained Individuals. J Strength Cond Res. 2022;36(3):600-607. doi:10.1519/JSC.0000000000003524 https://pubmed.ncbi.nlm.nih.gov/32058362/
La Scala Teixeira CV, Motoyama Y, de Azevedo PHSM, Evangelista AL, Steele J, Bocalini DS. Effect of resistance training set volume on upper body muscle hypertrophy: are more sets really better than less?. Clin Physiol Funct Imaging. 2018;38(5):727-732. doi:10.1111/cpf.12476 https://pubmed.ncbi.nlm.nih.gov/29024332/
Schoenfeld BJ, Grgic J, Haun C, Itagaki T, Helms ER. Calculating Set-Volume for the Limb Muscles with the Performance of Multi-Joint Exercises: Implications for Resistance Training Prescription. Sports (Basel). 2019;7(7):177. Published 2019 Jul 22. doi:10.3390/sports7070177 https://pubmed.ncbi.nlm.nih.gov/31336594/
Nunes JP, Kassiano W, Costa BDV, Mayhew JL, Ribeiro AS, Cyrino ES. Equating Resistance-Training Volume Between Programs Focused on Muscle Hypertrophy. Sports Med. 2021;51(6):1171-1178. doi:10.1007/s40279-021-01449-2 https://pubmed.ncbi.nlm.nih.gov/33826122/
Figueiredo VC, de Salles BF, Trajano GS. Volume for Muscle Hypertrophy and Health Outcomes: The Most Effective Variable in Resistance Training. Sports Med. 2018;48(3):499-505. doi:10.1007/s40279-017-0793-0 https://pubmed.ncbi.nlm.nih.gov/29022275/
Rocha JNS, Pereira-Monteiro MR, Vasconcelos ABS, Pantoja-Cardoso A, Aragão-Santos JC, Da Silva-Grigoletto ME. Different resistance training volumes on strength, functional fitness, and body composition of older people: A systematic review with meta-analysis. Arch Gerontol Geriatr. 2024;119:105303. doi:10.1016/j.archger.2023.105303 https://pubmed.ncbi.nlm.nih.gov/38128241/
Hamarsland H, Moen H, Skaar OJ, Jorang PW, Rødahl HS, Rønnestad BR. Equal-Volume Strength Training With Different Training Frequencies Induces Similar Muscle Hypertrophy and Strength Improvement in Trained Participants. Front Physiol. 2022;12:789403. Published 2022 Jan 5. doi:10.3389/fphys.2021.789403 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8766679/
Lasevicius T, Ugrinowitsch C, Schoenfeld BJ, et al. Effects of different intensities of resistance training with equated volume load on muscle strength and hypertrophy. Eur J Sport Sci. 2018;18(6):772-780. doi:10.1080/17461391.2018.1450898 https://pubmed.ncbi.nlm.nih.gov/29564973/
Jenkins ND, Housh TJ, Buckner SL, et al. Neuromuscular Adaptations After 2 and 4 Weeks of 80% Versus 30% 1 Repetition Maximum Resistance Training to Failure. J Strength Cond Res. 2016;30(8):2174-2185. doi:10.1519/JSC.0000000000001308 https://pubmed.ncbi.nlm.nih.gov/26848545/
Davies T, Orr R, Halaki M, Hackett D. Erratum to: Effect of Training Leading to Repetition Failure on Muscular Strength: A Systematic Review and Meta-Analysis. Sports Med. 2016;46(4):605-610. doi:10.1007/s40279-016-0509-x https://pubmed.ncbi.nlm.nih.gov/26893097/
Martorelli S, Cadore EL, Izquierdo M, et al. Strength Training with Repetitions to Failure does not Provide Additional Strength and Muscle Hypertrophy Gains in Young Women. Eur J Transl Myol. 2017;27(2):6339. Published 2017 Jun 27. doi:10.4081/ejtm.2017.6339 https://pubmed.ncbi.nlm.nih.gov/28713535/
Morán-Navarro R, Pérez CE, Mora-Rodríguez R, et al. Time course of recovery following resistance training leading or not to failure. Eur J Appl Physiol. 2017;117(12):2387-2399. doi:10.1007/s00421-017-3725-7 https://pubmed.ncbi.nlm.nih.gov/28965198/
Santos WDND, Vieira CA, Bottaro M, et al. Resistance Training Performed to Failure or Not to Failure Results in Similar Total Volume, but With Different Fatigue and Discomfort Levels. J Strength Cond Res. 2021;35(5):1372-1379. doi:10.1519/JSC.0000000000002915 https://pubmed.ncbi.nlm.nih.gov/30615007/
Sampson JA, Groeller H. Is repetition failure critical for the development of muscle hypertrophy and strength?. Scand J Med Sci Sports. 2016;26(4):375-383. doi:10.1111/sms.12445 https://pubmed.ncbi.nlm.nih.gov/25809472/
Steele J, Endres A, Fisher J, Gentil P, Giessing J. Ability to predict repetitions to momentary failure is not perfectly accurate, though improves with resistance training experience. PeerJ. 2017;5:e4105. Published 2017 Nov 30. doi:10.7717/peerj.4105 https://pubmed.ncbi.nlm.nih.gov/29204323/
Sundstrup E, Jakobsen MD, Andersen CH, Zebis MK, Mortensen OS, Andersen LL. Muscle activation strategies during strength training with heavy loading vs. repetitions to failure. J Strength Cond Res. 2012;26(7):1897-1903. doi:10.1519/JSC.0b013e318239c38e https://pubmed.ncbi.nlm.nih.gov/21986694/
Zourdos MC, Goldsmith JA, Helms ER, et al. Proximity to Failure and Total Repetitions Performed in a Set Influences Accuracy of Intraset Repetitions in Reserve-Based Rating of Perceived Exertion. J Strength Cond Res. 2021;35(Suppl 1):S158-S165. doi:10.1519/JSC.0000000000002995 https://pubmed.ncbi.nlm.nih.gov/30747900/
Washburn RA, Donnelly JE, Smith BK, Sullivan DK, Marquis J, Herrmann SD. Resistance training volume, energy balance and weight management: rationale and design of a 9 month trial. Contemp Clin Trials. 2012;33(4):749-758. doi:10.1016/j.cct.2012.03.002 https://pubmed.ncbi.nlm.nih.gov/22446169/
Starkey DB, Pollock ML, Ishida Y, et al. Effect of resistance training volume on strength and muscle thickness. Med Sci Sports Exerc. 1996;28(10):1311-1320. doi:10.1097/00005768-199610000-00016 https://pubmed.ncbi.nlm.nih.gov/8897390/
Roth C, Schwiete C, Happ K, Rettenmaier L, Schoenfeld BJ, Behringer M. Resistance training volume does not influence lean mass preservation during energy restriction in trained males. Scand J Med Sci Sports. 2023;33(1):20-35. doi:10.1111/sms.14237 https://pubmed.ncbi.nlm.nih.gov/36114738/
Mangine GT, Hoffman JR, Wang R, et al. Resistance training intensity and volume affect changes in rate of force development in resistance-trained men. Eur J Appl Physiol. 2016;116(11-12):2367-2374. doi:10.1007/s00421-016-3488-6 https://pubmed.ncbi.nlm.nih.gov/27744584/
Peterson MD, Pistilli E, Haff GG, Hoffman EP, Gordon PM. Progression of volume load and muscular adaptation during resistance exercise. Eur J Appl Physiol. 2011;111(6):1063-1071. doi:10.1007/s00421-010-1735-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4215195/
Borde R, Hortobágyi T, Granacher U. Dose-Response Relationships of Resistance Training in Healthy Old Adults: A Systematic Review and Meta-Analysis. Sports Med. 2015;45(12):1693-1720. doi:10.1007/s40279-015-0385-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656698/
Wilk M, Zajac A, Tufano JJ. The Influence of Movement Tempo During Resistance Training on Muscular Strength and Hypertrophy Responses: A Review. Sports Med. 2021;51(8):1629-1650. doi:10.1007/s40279-021-01465-2 https://pubmed.ncbi.nlm.nih.gov/34043184/
Grgic J, Lazinica B, Mikulic P, Krieger JW, Schoenfeld BJ. The effects of short versus long inter-set rest intervals in resistance training on measures of muscle hypertrophy: A systematic review. Eur J Sport Sci. 2017;17(8):983-993. doi:10.1080/17461391.2017.1340524 https://pubmed.ncbi.nlm.nih.gov/28641044/
Mike JN, Cole N, Herrera C, VanDusseldorp T, Kravitz L, Kerksick CM. The Effects of Eccentric Contraction Duration on Muscle Strength, Power Production, Vertical Jump, and Soreness. J Strength Cond Res. 2017;31(3):773-786. doi:10.1519/JSC.0000000000001675 https://pubmed.ncbi.nlm.nih.gov/27787464/
Coratella G. Appropriate Reporting of Exercise Variables in Resistance Training Protocols: Much more than Load and Number of Repetitions. Sports Med Open. 2022;8(1):99. Published 2022 Jul 30. doi:10.1186/s40798-022-00492-1 https://pubmed.ncbi.nlm.nih.gov/35907047/
Krzysztofik M, Matykiewicz P, Filip-Stachnik A, Humińska-Lisowska K, Rzeszutko-Bełzowska A, Wilk M. Range of motion of resistance exercise affects the number of performed repetitions but not a time under tension. Sci Rep. 2021;11(1):14847. Published 2021 Jul 21. doi:10.1038/s41598-021-94338-7 https://pubmed.ncbi.nlm.nih.gov/34290302/
Brandenburg JP, Docherty D. The effects of accentuated eccentric loading on strength, muscle hypertrophy, and neural adaptations in trained individuals. J Strength Cond Res. 2002;16(1):25-32. https://pubmed.ncbi.nlm.nih.gov/11834103/
Mang ZA, Realzola RA, Ducharme J, et al. The effect of repetition tempo on cardiovascular and metabolic stress when time under tension is matched during lower body exercise. Eur J Appl Physiol. 2022;122(6):1485-1495. doi:10.1007/s00421-022-04941-3 https://pubmed.ncbi.nlm.nih.gov/35394146/
Azevedo PHSM, Oliveira MGD, Schoenfeld BJ. Effect of different eccentric tempos on hypertrophy and strength of the lower limbs. Biol Sport. 2022;39(2):443-449. doi:10.5114/biolsport.2022.105335 https://pubmed.ncbi.nlm.nih.gov/35309524/
Headley SA, Henry K, Nindl BC, Thompson BA, Kraemer WJ, Jones MT. Effects of lifting tempo on one repetition maximum and hormonal responses to a bench press protocol. J Strength Cond Res. 2011;25(2):406-413. doi:10.1519/JSC.0b013e3181bf053b https://pubmed.ncbi.nlm.nih.gov/20351575/
Sooneste H, Tanimoto M, Kakigi R, Saga N, Katamoto S. Effects of training volume on strength and hypertrophy in young men. J Strength Cond Res. 2013;27(1):8-13. doi:10.1519/JSC.0b013e3182679215 https://pubmed.ncbi.nlm.nih.gov/23249767/
de França HS, Branco PA, Guedes Junior DP, Gentil P, Steele J, Teixeira CV. The effects of adding single-joint exercises to a multi-joint exercise resistance training program on upper body muscle strength and size in trained men. Appl Physiol Nutr Metab. 2015;40(8):822-826. doi:10.1139/apnm-2015-0109 https://pubmed.ncbi.nlm.nih.gov/26244600/
Slater LV, Hart JM. Muscle Activation Patterns During Different Squat Techniques. J Strength Cond Res. 2017;31(3):667-676. doi:10.1519/JSC.0000000000001323 https://pubmed.ncbi.nlm.nih.gov/26808843/
Bourne MN, Williams MD, Opar DA, Al Najjar A, Kerr GK, Shield AJ. Impact of exercise selection on hamstring muscle activation. Br J Sports Med. 2017;51(13):1021-1028. doi:10.1136/bjsports-2015-095739 https://pubmed.ncbi.nlm.nih.gov/27467123/
McCann MR, Flanagan SP. The effects of exercise selection and rest interval on postactivation potentiation of vertical jump performance. J Strength Cond Res. 2010;24(5):1285-1291. doi:10.1519/JSC.0b013e3181d6867c https://pubmed.ncbi.nlm.nih.gov/20393352/
Rauch JT, Ugrinowitsch C, Barakat CI, et al. Auto-Regulated Exercise Selection Training Regimen Produces Small Increases in Lean Body Mass and Maximal Strength Adaptations in Strength-trained Individuals. J Strength Cond Res. 2020;34(4):1133-1140. doi:10.1519/JSC.0000000000002272 https://pubmed.ncbi.nlm.nih.gov/29016481/
Smith E, Sepulveda A, Martinez VGF, Samaniego A, Marchetti PN, Marchetti PH. Exercise Variability Did Not Affect Muscle Thickness and Peak Force for Elbow Flexors After a Resistance Training Session in Recreationally-Trained Subjects. Int J Exerc Sci. 2021;14(3):1294-1304. Published 2021 Nov 1. https://pubmed.ncbi.nlm.nih.gov/35096238/
Nunes JP, Grgic J, Cunha PM, et al. What influence does resistance exercise order have on muscular strength gains and muscle hypertrophy? A systematic review and meta-analysis. Eur J Sport Sci. 2021;21(2):149-157. doi:10.1080/17461391.2020.1733672 https://pubmed.ncbi.nlm.nih.gov/32077380/
Gentil P, Fisher J, Steele J. A Review of the Acute Effects and Long-Term Adaptations of Single- and Multi-Joint Exercises during Resistance Training. Sports Med. 2017;47(5):843-855. doi:10.1007/s40279-016-0627-5 https://pubmed.ncbi.nlm.nih.gov/27677913/
Avelar A, Ribeiro AS, Nunes JP, et al. Effects of order of resistance training exercises on muscle hypertrophy in young adult men. Appl Physiol Nutr Metab. 2019;44(4):420-424. doi:10.1139/apnm-2018-0478 https://pubmed.ncbi.nlm.nih.gov/30248269/
Tomeleri CM, Ribeiro AS, Nunes JP, et al. Influence of Resistance Training Exercise Order on Muscle Strength, Hypertrophy, and Anabolic Hormones in Older Women: A Randomized Controlled Trial. J Strength Cond Res. 2020;34(11):3103-3109. doi:10.1519/JSC.0000000000003147 https://pubmed.ncbi.nlm.nih.gov/33105360/
Costa BDV, Kassiano W, Nunes JP, et al. Does Varying Resistance Exercises for the Same Muscle Group Promote Greater Strength Gains?. J Strength Cond Res. 2022;36(11):3032-3039. doi:10.1519/JSC.0000000000004042 https://pubmed.ncbi.nlm.nih.gov/35481889/
Helgerud J, Høydal K, Wang E, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39(4):665-671. doi:10.1249/mss.0b013e3180304570 https://pubmed.ncbi.nlm.nih.gov/17414804/
Acevedo EO, Goldfarb AH. Increased training intensity effects on plasma lactate, ventilatory threshold, and endurance. Med Sci Sports Exerc. 1989;21(5):563-568. https://pubmed.ncbi.nlm.nih.gov/2607946/
McConell GK, Costill DL, Widrick JJ, Hickey MS, Tanaka H, Gastin PB. Reduced training volume and intensity maintain aerobic capacity but not performance in distance runners. Int J Sports Med. 1993;14(1):33-37. doi:10.1055/s-2007-1021142 https://pubmed.ncbi.nlm.nih.gov/8440543/
Belman MJ, Gaesser GA. Exercise training below and above the lactate threshold in the elderly. Med Sci Sports Exerc. 1991;23(5):562-568. https://pubmed.ncbi.nlm.nih.gov/2072834/
Ito G, Feeley M, Sawai T, et al. High-intensity interval training improves respiratory and cardiovascular adjustments before and after initiation of exercise. Front Physiol. 2024;15:1227316. Published 2024 Mar 11. doi:10.3389/fphys.2024.1227316 https://pubmed.ncbi.nlm.nih.gov/38529482/
Mølmen KS, Øfsteng SJ, Rønnestad BR. Block periodization of endurance training – a systematic review and meta-analysis. Open Access J Sports Med. 2019;10:145-160. Published 2019 Oct 17. doi:10.2147/OAJSM.S180408 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6802561/
Meyer T, Auracher M, Heeg K, Urhausen A, Kindermann W. Effectiveness of low-intensity endurance training. Int J Sports Med. 2007;28(1):33-39. doi:10.1055/s-2006-924037 https://pubmed.ncbi.nlm.nih.gov/17213964/
Ferretti G, Fagoni N, Taboni A, Bruseghini P, Vinetti G. The physiology of submaximal exercise: The steady state concept. Respir Physiol Neurobiol. 2017;246:76-85. doi:10.1016/j.resp.2017.08.005 https://pubmed.ncbi.nlm.nih.gov/28818484/
Neufeld EV, Wadowski J, Boland DM, Dolezal BA, Cooper CB. Heart Rate Acquisition and Threshold-Based Training Increases Oxygen Uptake at Metabolic Threshold in Triathletes: A Pilot Study. Int J Exerc Sci. 2019;12(2):144-154. Published 2019 Jan 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6355121/
Zhu Z, Li H, Xiao J, Xu W, Huang MC. A fitness training optimization system based on heart rate prediction under different activities. Methods. 2022;205:89-96. doi:10.1016/j.ymeth.2022.06.006 https://pubmed.ncbi.nlm.nih.gov/35750282/
Lim AY, Chen YC, Hsu CC, Fu TC, Wang JS. The Effects of Exercise Training on Mitochondrial Function in Cardiovascular Diseases: A Systematic Review and Meta-Analysis. Int J Mol Sci. 2022;23(20):12559. Published 2022 Oct 19. doi:10.3390/ijms232012559 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9603958/
Shiraev T, Barclay G. Evidence based exercise – clinical benefits of high intensity interval training. Aust Fam Physician. 2012;41(12):960-962. https://pubmed.ncbi.nlm.nih.gov/23210120/
Laursen PB, Jenkins DG. The scientific basis for high-intensity interval training: optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med. 2002;32(1):53-73. doi:10.2165/00007256-200232010-00003 https://pubmed.ncbi.nlm.nih.gov/11772161/
Kubukeli ZN, Noakes TD, Dennis SC. Training techniques to improve endurance exercise performances. Sports Med. 2002;32(8):489-509. doi:10.2165/00007256-200232080-00002 https://pubmed.ncbi.nlm.nih.gov/12076176/
Laursen PB, Shing CM, Peake JM, Coombes JS, Jenkins DG. Influence of high-intensity interval training on adaptations in well-trained cyclists. J Strength Cond Res. 2005;19(3):527-533. doi:10.1519/15964.1 https://pubmed.ncbi.nlm.nih.gov/16095414/
Esfarjani F, Laursen PB. Manipulating high-intensity interval training: effects on VO2max, the lactate threshold and 3000 m running performance in moderately trained males. J Sci Med Sport. 2007;10(1):27-35. doi:10.1016/j.jsams.2006.05.014 https://pubmed.ncbi.nlm.nih.gov/16876479/
Normand-Gravier T, Britto F, Launay T, Renfree A, Toussaint JF, Desgorces FD. Exercise Dose Equalization in High-Intensity Interval Training: A Scoping Review. Int J Environ Res Public Health. 2022;19(9):4980. Published 2022 Apr 20. doi:10.3390/ijerph19094980 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9104727/
Carey DG. Quantifying differences in the “fat burning” zone and the aerobic zone: implications for training. J Strength Cond Res. 2009;23(7):2090-2095. doi:10.1519/JSC.0b013e3181bac5c5 https://pubmed.ncbi.nlm.nih.gov/19855335/
Huang G, Wang R, Chen P, Huang SC, Donnelly JE, Mehlferber JP. Dose-response relationship of cardiorespiratory fitness adaptation to controlled endurance training in sedentary older adults. Eur J Prev Cardiol. 2016;23(5):518-529. doi:10.1177/2047487315582322 https://pubmed.ncbi.nlm.nih.gov/25901000/
Huang G, Gibson CA, Tran ZV, Osness WH. Controlled endurance exercise training and VO2max changes in older adults: a meta-analysis. Prev Cardiol. 2005;8(4):217-225. doi:10.1111/j.0197-3118.2005.04324.x https://pubmed.ncbi.nlm.nih.gov/16230876/
Katzel LI, Sorkin JD, Fleg JL. A comparison of longitudinal changes in aerobic fitness in older endurance athletes and sedentary men. J Am Geriatr Soc. 2001;49(12):1657-1664. doi:10.1046/j.1532-5415.2001.t01-1-49276.x https://pubmed.ncbi.nlm.nih.gov/11844000/
Rogers MA, Hagberg JM, Martin WH 3rd, Ehsani AA, Holloszy JO. Decline in VO2max with aging in master athletes and sedentary men. J Appl Physiol (1985). 1990;68(5):2195-2199. doi:10.1152/jappl.1990.68.5.2195 https://pubmed.ncbi.nlm.nih.gov/2361923/
Vajda M, Oreská Ľ, Černáčková A, et al. Aging and Possible Benefits or Negatives of Lifelong Endurance Running: How Master Male Athletes Differ from Young Athletes and Elderly Sedentary?. Int J Environ Res Public Health. 2022;19(20):13184. Published 2022 Oct 13. doi:10.3390/ijerph192013184 https://pubmed.ncbi.nlm.nih.gov/36293774/
Montero D, Díaz-Cañestro C. Endurance training and maximal oxygen consumption with ageing: Role of maximal cardiac output and oxygen extraction. Eur J Prev Cardiol. 2016;23(7):733-743. doi:10.1177/2047487315617118 https://pubmed.ncbi.nlm.nih.gov/26553969/
Montero D, Diaz-Cañestro C, Lundby C. Endurance Training and V˙O2max: Role of Maximal Cardiac Output and Oxygen Extraction. Med Sci Sports Exerc. 2015;47(10):2024-2033. doi:10.1249/MSS.0000000000000640 https://pubmed.ncbi.nlm.nih.gov/25680086/
Tanisho K, Hirakawa K. Training effects on endurance capacity in maximal intermittent exercise: comparison between continuous and interval training. J Strength Cond Res. 2009;23(8):2405-2410. doi:10.1519/JSC.0b013e3181bac790 https://pubmed.ncbi.nlm.nih.gov/19826281/
Ziemann E, Grzywacz T, Łuszczyk M, Laskowski R, Olek RA, Gibson AL. Aerobic and anaerobic changes with high-intensity interval training in active college-aged men. J Strength Cond Res. 2011;25(4):1104-1112. doi:10.1519/JSC.0b013e3181d09ec9 https://pubmed.ncbi.nlm.nih.gov/20661160/
Wang C, Xu Y, Zhang L, et al. Comparative efficacy of different exercise methods to improve cardiopulmonary function in stroke patients: a network meta-analysis of randomized controlled trials. Front Neurol. 2024;15:1288032. Published 2024 Jan 17. doi:10.3389/fneur.2024.1288032 https://pubmed.ncbi.nlm.nih.gov/38313560/
Mikkonen RS, Ihalainen JK, Hackney AC, Häkkinen K. Perspectives on Concurrent Strength and Endurance Training in Healthy Adult Females: A Systematic Review. Sports Med. 2024;54(3):673-696. doi:10.1007/s40279-023-01955-5 https://pubmed.ncbi.nlm.nih.gov/37948036/
Markov A, Hauser L, Chaabene H. Effects of Concurrent Strength and Endurance Training on Measures of Physical Fitness in Healthy Middle-Aged and Older Adults: A Systematic Review with Meta-Analysis. Sports Med. 2023;53(2):437-455. doi:10.1007/s40279-022-01764-2 https://pubmed.ncbi.nlm.nih.gov/36222981/
Heyne E, Zeeb S, Junker C, et al. Exercise Training Differentially Affects Skeletal Muscle Mitochondria in Rats with Inherited High or Low Exercise Capacity. Cells. 2024;13(5):393. Published 2024 Feb 24. doi:10.3390/cells13050393 https://pubmed.ncbi.nlm.nih.gov/38474357/
Nikolaidis PT, Knechtle B. Predictors of half-marathon performance in male recreational athletes. EXCLI J. 2023;22:559-566. Published 2023 Jun 22. doi:10.17179/excli2023-6198 https://pubmed.ncbi.nlm.nih.gov/37534223/
Daussin FN, Ponsot E, Dufour SP, et al. Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur J Appl Physiol. 2007;101(3):377-383. doi:10.1007/s00421-007-0499-3 https://pubmed.ncbi.nlm.nih.gov/17661072/
Sperlich B, Matzka M, Holmberg HC. The proportional distribution of training by elite endurance athletes at different intensities during different phases of the season. Front Sports Act Living. 2023;5:1258585. Published 2023 Oct 27. doi:10.3389/fspor.2023.1258585 https://pubmed.ncbi.nlm.nih.gov/37964776/
Cao M, Quan M, Zhuang J. Effect of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Cardiorespiratory Fitness in Children and Adolescents: A Meta-Analysis. Int J Environ Res Public Health. 2019;16(9):1533. Published 2019 Apr 30. doi:10.3390/ijerph16091533 https://pubmed.ncbi.nlm.nih.gov/31052205/
Monserdà-Vilaró A, Balsalobre-Fernández C, Hoffman JR, Alix-Fages C, Jiménez SL. Effects of Concurrent Resistance and Endurance Training Using Continuous or Intermittent Protocols on Muscle Hypertrophy: Systematic Review With Meta-Analysis. J Strength Cond Res. 2023;37(3):688-709. doi:10.1519/JSC.0000000000004304 https://pubmed.ncbi.nlm.nih.gov/36508686/
Burgomaster KA, Howarth KR, Phillips SM, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol. 2008;586(1):151-160. doi:10.1113/jphysiol.2007.142109 https://pubmed.ncbi.nlm.nih.gov/17991697/
Hawley JA. Specificity of training adaptation: time for a rethink?. J Physiol. 2008;586(1):1-2. doi:10.1113/jphysiol.2007.147397 https://pubmed.ncbi.nlm.nih.gov/18167367/
Gibala MJ, Little JP, van Essen M, et al. Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol. 2006;575(Pt 3):901-911. doi:10.1113/jphysiol.2006.112094 https://pubmed.ncbi.nlm.nih.gov/16825308/
Gibala MJ, Jones AM. Physiological and performance adaptations to high-intensity interval training. Nestle Nutr Inst Workshop Ser. 2013;76:51-60. doi:10.1159/000350256 https://pubmed.ncbi.nlm.nih.gov/23899754/
Ekkekakis P, Swinton P, Tiller NB. Extraordinary Claims in the Literature on High-Intensity Interval Training (HIIT): I. Bonafide Scientific Revolution or a Looming Crisis of Replication and Credibility?. Sports Med. 2023;53(10):1865-1890. doi:10.1007/s40279-023-01880-7 https://pubmed.ncbi.nlm.nih.gov/37561389/
Ekkekakis P, Vallance J, Wilson PM, Ewing Garber C. Extraordinary claims in the literature on high-intensity interval training (HIIT): III. Critical analysis of four foundational arguments from an interdisciplinary lens. Psychol Sport Exerc. 2023;66:102399. doi:10.1016/j.psychsport.2023.102399 https://pubmed.ncbi.nlm.nih.gov/37665861/
Ekkekakis P, Biddle SJH. Extraordinary claims in the literature on high-intensity interval training (HIIT): IV. Is HIIT associated with higher long-term exercise adherence?. Psychol Sport Exerc. 2023;64:102295. doi:10.1016/j.psychsport.2022.102295 https://pubmed.ncbi.nlm.nih.gov/37665824/
Coates AM, Joyner MJ, Little JP, Jones AM, Gibala MJ. A Perspective on High-Intensity Interval Training for Performance and Health. Sports Med. 2023;53(Suppl 1):85-96. doi:10.1007/s40279-023-01938-6 https://pubmed.ncbi.nlm.nih.gov/37804419/
Cochran AJ, Percival ME, Tricarico S, et al. Intermittent and continuous high-intensity exercise training induce similar acute but different chronic muscle adaptations. Exp Physiol. 2014;99(5):782-791. doi:10.1113/expphysiol.2013.077453 https://pubmed.ncbi.nlm.nih.gov/24532598/
Laursen PB. Training for intense exercise performance: high-intensity or high-volume training?. Scand J Med Sci Sports. 2010;20 Suppl 2:1-10. doi:10.1111/j.1600-0838.2010.01184.x https://pubmed.ncbi.nlm.nih.gov/20840557/
Ross A, Leveritt M. Long-term metabolic and skeletal muscle adaptations to short-sprint training: implications for sprint training and tapering. Sports Med. 2001;31(15):1063-1082. doi:10.2165/00007256-200131150-00003 https://pubmed.ncbi.nlm.nih.gov/11735686/
Soylu Y, Krustrup P, Mohr M, Arslan E, Kilit B, Radzimiński Ł. Effects of Two Different Self-Paced Training Modalities on the Aerobic Fitness Levels, Psychophysiological Responses, and Antioxidant Status in Physically Active Young Adults. J Clin Med. 2023;12(23):7232. Published 2023 Nov 22. doi:10.3390/jcm12237232 https://pubmed.ncbi.nlm.nih.gov/38068283/
Little JP, Safdar A, Wilkin GP, Tarnopolsky MA, Gibala MJ. A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: potential mechanisms. J Physiol. 2010;588(Pt 6):1011-1022. doi:10.1113/jphysiol.2009.181743 https://pubmed.ncbi.nlm.nih.gov/20100740/
Hood MS, Little JP, Tarnopolsky MA, Myslik F, Gibala MJ. Low-volume interval training improves muscle oxidative capacity in sedentary adults. Med Sci Sports Exerc. 2011;43(10):1849-1856. doi:10.1249/MSS.0b013e3182199834 https://pubmed.ncbi.nlm.nih.gov/21448086/
Gibala MJ, McGee SL. Metabolic adaptations to short-term high-intensity interval training: a little pain for a lot of gain?. Exerc Sport Sci Rev. 2008;36(2):58-63. doi:10.1097/JES.0b013e318168ec1f https://pubmed.ncbi.nlm.nih.gov/18362686/
Astorino TA, Schubert MM, Palumbo E, et al. Magnitude and time course of changes in maximal oxygen uptake in response to distinct regimens of chronic interval training in sedentary women. Eur J Appl Physiol. 2013;113(9):2361-2369. doi:10.1007/s00421-013-2672-1 https://pubmed.ncbi.nlm.nih.gov/23754097/
Hickson RC, Bomze HA, Holloszy JO. Linear increase in aerobic power induced by a strenuous program of endurance exercise. J Appl Physiol Respir Environ Exerc Physiol. 1977;42(3):372-376. doi:10.1152/jappl.1977.42.3.372 https://pubmed.ncbi.nlm.nih.gov/838658/
Habibi E, Dehghan H, Moghiseh M, Hasanzadeh A. Study of the relationship between the aerobic capacity (VO2 max) and the rating of perceived exertion based on the measurement of heart beat in the metal industries Esfahan. J Educ Health Promot. 2014;3:55. Published 2014 Jun 23. doi:10.4103/2277-9531.134751 https://pubmed.ncbi.nlm.nih.gov/25077148/
Losnegard T, Skarli S, Hansen J, et al. Is Rating of Perceived Exertion a Valuable Tool for Monitoring Exercise Intensity During Steady-State Conditions in Elite Endurance Athletes?. Int J Sports Physiol Perform. 2021;16(11):1589-1595. doi:10.1123/ijspp.2020-0866 https://pubmed.ncbi.nlm.nih.gov/33831841/
Zamunér AR, Moreno MA, Camargo TM, et al. Assessment of Subjective Perceived Exertion at the Anaerobic Threshold with the Borg CR-10 Scale. J Sports Sci Med. 2011;10(1):130-136. Published 2011 Mar 1. https://pubmed.ncbi.nlm.nih.gov/24149305/
Cunha FA, Midgley AW, Monteiro WD, Campos FK, Farinatti PT. The relationship between oxygen uptake reserve and heart rate reserve is affected by intensity and duration during aerobic exercise at constant work rate. Appl Physiol Nutr Metab. 2011;36(6):839-847. doi:10.1139/h11-100 https://pubmed.ncbi.nlm.nih.gov/22034854/
Hwang J, Moon NR, Heine O, Yang WH. The ability of energy recovery in professional soccer players is increased by individualized low-intensity exercise. PLoS One. 2022;17(6):e0270484. Published 2022 Jun 30. doi:10.1371/journal.pone.0270484 https://pubmed.ncbi.nlm.nih.gov/35771850/
Stanley J, Peake JM, Buchheit M. Cardiac parasympathetic reactivation following exercise: implications for training prescription. Sports Med. 2013;43(12):1259-1277. doi:10.1007/s40279-013-0083-4 https://pubmed.ncbi.nlm.nih.gov/23912805/
Buchheit M, Simon C, Piquard F, Ehrhart J, Brandenberger G. Effects of increased training load on vagal-related indexes of heart rate variability: a novel sleep approach. Am J Physiol Heart Circ Physiol. 2004;287(6):H2813-H2818. doi:10.1152/ajpheart.00490.2004 https://pubmed.ncbi.nlm.nih.gov/15308479/
Iwasaki K, Zhang R, Zuckerman JH, Levine BD. Dose-response relationship of the cardiovascular adaptation to endurance training in healthy adults: how much training for what benefit?. J Appl Physiol (1985). 2003;95(4):1575-1583. doi:10.1152/japplphysiol.00482.2003 https://pubmed.ncbi.nlm.nih.gov/12832429/
Weeks KL, McMullen JR. The athlete’s heart vs. the failing heart: can signaling explain the two distinct outcomes?. Physiology (Bethesda). 2011;26(2):97-105. doi:10.1152/physiol.00043.2010 https://pubmed.ncbi.nlm.nih.gov/21487028/
Tomlin DL, Wenger HA. The relationship between aerobic fitness and recovery from high intensity intermittent exercise. Sports Med. 2001;31(1):1-11. doi:10.2165/00007256-200131010-00001 https://pubmed.ncbi.nlm.nih.gov/11219498/
Børsheim E, Bahr R. Effect of exercise intensity, duration and mode on post-exercise oxygen consumption. Sports Med. 2003;33(14):1037-1060. doi:10.2165/00007256-200333140-00002 https://pubmed.ncbi.nlm.nih.gov/14599232/
Jones AM, Carter H. The effect of endurance training on parameters of aerobic fitness. Sports Med. 2000;29(6):373-386. doi:10.2165/00007256-200029060-00001 https://pubmed.ncbi.nlm.nih.gov/10870864/
Bell GJ, Snydmiller GD, Davies DS, Quinney HA. Relationship between aerobic fitness and metabolic recovery from intermittent exercise in endurance athletes . Can J Appl Physiol. 1997;22(1):78-85. doi:10.1139/h97-008 https://pubmed.ncbi.nlm.nih.gov/9018410/
Sloth M, Sloth D, Overgaard K, Dalgas U. Effects of sprint interval training on VO2max and aerobic exercise performance: A systematic review and meta-analysis. Scand J Med Sci Sports. 2013;23(6):e341-e352. doi:10.1111/sms.12092 https://pubmed.ncbi.nlm.nih.gov/23889316/
Lundberg TR, Larsson G, Alstermark R, Mandić M, Fernandez-Gonzalo R. Relationship between maximal oxygen uptake, within-set fatigue and between-set recovery during resistance exercise in resistance-trained men and women. BMC Sports Sci Med Rehabil. 2024;16(1):45. Published 2024 Feb 12. doi:10.1186/s13102-024-00830-8 https://pubmed.ncbi.nlm.nih.gov/38347629/
Saw AE, Main LC, Gastin PB. Monitoring the athlete training response: subjective self-reported measures trump commonly used objective measures: a systematic review. Br J Sports Med. 2016;50(5):281-291. doi:10.1136/bjsports-2015-094758 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4789708/
Muñoz I, Seiler S, Bautista J, España J, Larumbe E, Esteve-Lanao J. Does polarized training improve performance in recreational runners?. Int J Sports Physiol Perform. 2014;9(2):265-272. doi:10.1123/ijspp.2012-0350 https://pubmed.ncbi.nlm.nih.gov/23752040/
Alizadeh S, Daneshjoo A, Zahiri A, et al. Resistance Training Induces Improvements in Range of Motion: A Systematic Review and Meta-Analysis. Sports Med. 2023;53(3):707-722. doi:10.1007/s40279-022-01804-x https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9935664/
Afonso J, Ramirez-Campillo R, Moscão J, et al. Strength Training versus Stretching for Improving Range of Motion: A Systematic Review and Meta-Analysis. Healthcare (Basel). 2021;9(4):427. Published 2021 Apr 7. doi:10.3390/healthcare9040427 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8067745/
Opplert J, Babault N. Acute Effects of Dynamic Stretching on Muscle Flexibility and Performance: An Analysis of the Current Literature. Sports Med. 2018;48(2):299-325. doi:10.1007/s40279-017-0797-9 https://pubmed.ncbi.nlm.nih.gov/29063454/
Stathokostas L, McDonald MW, Little RM, Paterson DH. Flexibility of older adults aged 55-86 years and the influence of physical activity. J Aging Res. 2013;2013:743843. doi:10.1155/2013/743843 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3703899/
Leite T, de Souza Teixeira A, Saavedra F, Leite RD, Rhea MR, Simão R. Influence of strength and flexibility training, combined or isolated, on strength and flexibility gains. J Strength Cond Res. 2015;29(4):1083-1088. doi:10.1519/JSC.0000000000000719 https://pubmed.ncbi.nlm.nih.gov/25268286/
Stathokostas L, Little RM, Vandervoort AA, Paterson DH. Flexibility training and functional ability in older adults: a systematic review. J Aging Res. 2012;2012:306818. doi:10.1155/2012/306818 https://pubmed.ncbi.nlm.nih.gov/23209904/
Treacy D, Hassett L, Schurr K, Fairhall NJ, Cameron ID, Sherrington C. Mobility training for increasing mobility and functioning in older people with frailty. Cochrane Database Syst Rev. 2022;6(6):CD010494. Published 2022 Jun 30. doi:10.1002/14651858.CD010494.pub2 https://pubmed.ncbi.nlm.nih.gov/35771806/
Pfeifer CE, Ross LM, Weber SR, Sui X, Blair SN. Are flexibility and muscle-strengthening activities associated with functional limitation?. Sports Med Health Sci. 2022;4(2):95-100. Published 2022 Mar 18. doi:10.1016/j.smhs.2022.03.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9219252/
Gleim GW, McHugh MP. Flexibility and its effects on sports injury and performance. Sports Med. 1997;24(5):289-299. doi:10.2165/00007256-199724050-00001 https://pubmed.ncbi.nlm.nih.gov/9368275/
Granacher U, Hortobágyi T. Exercise to Improve Mobility in Healthy Aging. Sports Med. 2015;45(12):1625-1626. doi:10.1007/s40279-015-0405-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656693/
Morton SK, Whitehead JR, Brinkert RH, Caine DJ. Resistance training vs. static stretching: effects on flexibility and strength. J Strength Cond Res. 2011;25(12):3391-3398. doi:10.1519/JSC.0b013e31821624aa https://pubmed.ncbi.nlm.nih.gov/21969080/
Iwata M, Yamamoto A, Matsuo S, et al. Dynamic Stretching Has Sustained Effects on Range of Motion and Passive Stiffness of the Hamstring Muscles. J Sports Sci Med. 2019;18(1):13-20. Published 2019 Feb 11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6370952/
Thomas E, Bellafiore M, Petrigna L, Paoli A, Palma A, Bianco A. Peripheral Nerve Responses to Muscle Stretching: A Systematic Review. J Sports Sci Med. 2021;20(2):258-267. Published 2021 Mar 8. doi:10.52082/jssm.2021.258 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8219270/
Micheo W, Baerga L, Miranda G. Basic principles regarding strength, flexibility, and stability exercises. PM R. 2012;4(11):805-811. doi:10.1016/j.pmrj.2012.09.583 https://pubmed.ncbi.nlm.nih.gov/23174542/
Witvrouw E, Mahieu N, Danneels L, McNair P. Stretching and injury prevention: an obscure relationship. Sports Med. 2004;34(7):443-449. doi:10.2165/00007256-200434070-00003 https://pubmed.ncbi.nlm.nih.gov/15233597/
Davies G, Riemann BL, Manske R. CURRENT CONCEPTS OF PLYOMETRIC EXERCISE. Int J Sports Phys Ther. 2015;10(6):760-786. https://pubmed.ncbi.nlm.nih.gov/26618058/
Grgic J, Schoenfeld BJ, Mikulic P. Effects of plyometric vs. resistance training on skeletal muscle hypertrophy: A review. J Sport Health Sci. 2021;10(5):530-536. doi:10.1016/j.jshs.2020.06.010 https://pubmed.ncbi.nlm.nih.gov/32579911/
Sáez de Villarreal E, Requena B, Cronin JB. The effects of plyometric training on sprint performance: a meta-analysis. J Strength Cond Res. 2012;26(2):575-584. doi:10.1519/JSC.0b013e318220fd03 https://pubmed.ncbi.nlm.nih.gov/22240550/
Ramírez-delaCruz M, Bravo-Sánchez A, Esteban-García P, Jiménez F, Abián-Vicén J. Effects of Plyometric Training on Lower Body Muscle Architecture, Tendon Structure, Stiffness and Physical Performance: A Systematic Review and Meta-analysis. Sports Med Open. 2022;8(1):40. Published 2022 Mar 21. doi:10.1186/s40798-022-00431-0 https://pubmed.ncbi.nlm.nih.gov/35312884/
Ramirez-Campillo R, Perez-Castilla A, Thapa RK, et al. Effects of Plyometric Jump Training on Measures of Physical Fitness and Sport-Specific Performance of Water Sports Athletes: A Systematic Review with Meta-analysis. Sports Med Open. 2022;8(1):108. Published 2022 Aug 29. doi:10.1186/s40798-022-00502-2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9424421/
Watkins CM, Storey AG, McGuigan MR, Gill ND. Implementation and Efficacy of Plyometric Training: Bridging the Gap Between Practice and Research. J Strength Cond Res. 2021;35(5):1244-1255. doi:10.1519/JSC.0000000000003985 https://pubmed.ncbi.nlm.nih.gov/33780396/
Makaruk H, Starzak M, Suchecki B, Czaplicki M, Stojiljković N. The Effects of Assisted and Resisted Plyometric Training Programs on Vertical Jump Performance in Adults: A Systematic Review and Meta-Analysis. J Sports Sci Med. 2020;19(2):347-357. Published 2020 May 1. https://pubmed.ncbi.nlm.nih.gov/32390728/
Hill J, Leiszler M. Review and role of plyometrics and core rehabilitation in competitive sport. Curr Sports Med Rep. 2011;10(6):345-351. doi:10.1249/JSR.0b013e31823b3b94 https://pubmed.ncbi.nlm.nih.gov/22071395/
Bedoya AA, Miltenberger MR, Lopez RM. Plyometric Training Effects on Athletic Performance in Youth Soccer Athletes: A Systematic Review. J Strength Cond Res. 2015;29(8):2351-2360. doi:10.1519/JSC.0000000000000877 https://pubmed.ncbi.nlm.nih.gov/25756326/
Fradkin AJ, Zazryn TR, Smoliga JM. Effects of warming-up on physical performance: a systematic review with meta-analysis. J Strength Cond Res. 2010;24(1):140-148. doi:10.1519/JSC.0b013e3181c643a0 https://pubmed.ncbi.nlm.nih.gov/19996770/
McGowan CJ, Pyne DB, Thompson KG, Rattray B. Warm-Up Strategies for Sport and Exercise: Mechanisms and Applications. Sports Med. 2015;45(11):1523-1546. doi:10.1007/s40279-015-0376-x https://pubmed.ncbi.nlm.nih.gov/26400696/
Bishop D. Warm up I: potential mechanisms and the effects of passive warm up on exercise performance. Sports Med. 2003;33(6):439-454. doi:10.2165/00007256-200333060-00005 https://pubmed.ncbi.nlm.nih.gov/12744717/
Bishop D. Warm up II: performance changes following active warm up and how to structure the warm up. Sports Med. 2003;33(7):483-498. doi:10.2165/00007256-200333070-00002 https://pubmed.ncbi.nlm.nih.gov/12762825/
Bengtsson V, Yu JG, Gilenstam K. Could the negative effects of static stretching in warm-up be balanced out by sport-specific exercise?. J Sports Med Phys Fitness. 2018;58(9):1185-1189. doi:10.23736/S0022-4707.17.07101-8 https://pubmed.ncbi.nlm.nih.gov/28409517/
Fradkin AJ, Gabbe BJ, Cameron PA. Does warming up prevent injury in sport? The evidence from randomised controlled trials?. J Sci Med Sport. 2006;9(3):214-220. doi:10.1016/j.jsams.2006.03.026 https://pubmed.ncbi.nlm.nih.gov/16679062/
McCrary JM, Ackermann BJ, Halaki M. A systematic review of the effects of upper body warm-up on performance and injury. Br J Sports Med. 2015;49(14):935-942. doi:10.1136/bjsports-2014-094228 https://pubmed.ncbi.nlm.nih.gov/25694615/
Taylor KL, Sheppard JM, Lee H, Plummer N. Negative effect of static stretching restored when combined with a sport specific warm-up component. J Sci Med Sport. 2009;12(6):657-661. doi:10.1016/j.jsams.2008.04.004 https://pubmed.ncbi.nlm.nih.gov/18768355/
Li FY, Guo CG, Li HS, Xu HR, Sun P. A systematic review and net meta-analysis of the effects of different warm-up methods on the acute effects of lower limb explosive strength. BMC Sports Sci Med Rehabil. 2023;15(1):106. Published 2023 Aug 29. doi:10.1186/s13102-023-00703-6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10463540/
Sander A, Keiner M, Schlumberger A, Wirth K, Schmidtbleicher D. Effects of functional exercises in the warm-up on sprint performances. J Strength Cond Res. 2013;27(4):995-1001. doi:10.1519/JSC.0b013e318260ec5e https://pubmed.ncbi.nlm.nih.gov/22692105/
Silva LM, Neiva HP, Marques MC, Izquierdo M, Marinho DA. Effects of Warm-Up, Post-Warm-Up, and Re-Warm-Up Strategies on Explosive Efforts in Team Sports: A Systematic Review. Sports Med. 2018;48(10):2285-2299. doi:10.1007/s40279-018-0958-5 https://pubmed.ncbi.nlm.nih.gov/29968230/
Shellock FG. Physiological Benefits of Warm-Up. Phys Sportsmed. 1983;11(10):134-139. doi:10.1080/00913847.1983.11708664 https://pubmed.ncbi.nlm.nih.gov/27442476/
Shellock FG, Prentice WE. Warming-up and stretching for improved physical performance and prevention of sports-related injuries. Sports Med. 1985;2(4):267-278. doi:10.2165/00007256-198502040-00004 https://pubmed.ncbi.nlm.nih.gov/3849057/
Smith CA. The warm-up procedure: to stretch or not to stretch. A brief review. J Orthop Sports Phys Ther. 1994;19(1):12-17. doi:10.2519/jospt.1994.19.1.12 https://pubmed.ncbi.nlm.nih.gov/8156057/
Afonso J, Brito J, Abade E, et al. Revisiting the ‘Whys’ and ‘Hows’ of the Warm-Up: Are We Asking the Right Questions?. Sports Med. 2024;54(1):23-30. doi:10.1007/s40279-023-01908-y https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10798919/
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. doi:10.1136/bjsports-2020-102955 https://pubmed.ncbi.nlm.nih.gov/33239350/
Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020-2028. doi:10.1001/jama.2018.14854 https://pubmed.ncbi.nlm.nih.gov/30418471/
O’Donovan G, Blazevich AJ, Boreham C, et al. The ABC of Physical Activity for Health: a consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci. 2010;28(6):573-591. doi:10.1080/02640411003671212 https://pubmed.ncbi.nlm.nih.gov/20401789/
Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423-1434. doi:10.1249/mss.0b013e3180616b27 https://pubmed.ncbi.nlm.nih.gov/17762377/
Du Y, Liu B, Sun Y, Snetselaar LG, Wallace RB, Bao W. Trends in Adherence to the Physical Activity Guidelines for Americans for Aerobic Activity and Time Spent on Sedentary Behavior Among US Adults, 2007 to 2016. JAMA Netw Open. 2019;2(7):e197597. Published 2019 Jul 3. doi:10.1001/jamanetworkopen.2019.7597 https://pubmed.ncbi.nlm.nih.gov/31348504/
Ding D, Mutrie N, Bauman A, Pratt M, Hallal PRC, Powell KE. Physical activity guidelines 2020: comprehensive and inclusive recommendations to activate populations. Lancet. 2020;396(10265):1780-1782. doi:10.1016/S0140-6736(20)32229-7 https://pubmed.ncbi.nlm.nih.gov/33248019/
DiPietro L, Al-Ansari SS, Biddle SJH, et al. Advancing the global physical activity agenda: recommendations for future research by the 2020 WHO physical activity and sedentary behavior guidelines development group. Int J Behav Nutr Phys Act. 2020;17(1):143. Published 2020 Nov 26. doi:10.1186/s12966-020-01042-2 https://pubmed.ncbi.nlm.nih.gov/33239105/
Burtscher J, Burtscher M. Run for your life: tweaking the weekly physical activity volume for longevity. Br J Sports Med. 2020;54(13):759-760. doi:10.1136/bjsports-2019-101350 https://pubmed.ncbi.nlm.nih.gov/31630092/
Marin-Couture E, Pérusse L, Tremblay A. The fit-active profile to better reflect the benefits of a lifelong vigorous physical activity participation: mini-review of literature and population data. Appl Physiol Nutr Metab. 2021;46(7):763-770. doi:10.1139/apnm-2020-1109 https://pubmed.ncbi.nlm.nih.gov/33667123/
O’Keefe JH, O’Keefe EL, Lavie CJ. The Goldilocks Zone for Exercise: Not Too Little, Not Too Much. Mo Med. 2018;115(2):98-105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139866/
O’Keefe JH, O’Keefe EL, Eckert R, Lavie CJ. Training Strategies to Optimize Cardiovascular Durability and Life Expectancy. Mo Med. 2023;120(2):155-162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10121111/
Lee DH, Rezende LFM, Joh HK, et al. Long-Term Leisure-Time Physical Activity Intensity and All-Cause and Cause-Specific Mortality: A Prospective Cohort of US Adults. Circulation. 2022;146(7):523-534. doi:10.1161/CIRCULATIONAHA.121.058162 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9378548/
Master H, Annis J, Huang S, et al. Association of step counts over time with the risk of chronic disease in the All of Us Research Program [published correction appears in Nat Med. 2023 Dec;29(12):3270]. Nat Med. 2022;28(11):2301-2308. doi:10.1038/s41591-022-02012-w https://pubmed.ncbi.nlm.nih.gov/36216933/
Choi BC, Pak AW, Choi JC, Choi EC. Daily step goal of 10,000 steps: a literature review. Clin Invest Med. 2007;30(3):E146-E151. doi:10.25011/cim.v30i3.1083 https://pubmed.ncbi.nlm.nih.gov/17716553/
Tudor-Locke C, Bassett DR Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34(1):1-8. doi:10.2165/00007256-200434010-00001 https://pubmed.ncbi.nlm.nih.gov/14715035/
Paluch AE, Bajpai S, Bassett DR, et al. Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public Health. 2022;7(3):e219-e228. doi:10.1016/S2468-2667(21)00302-9 https://pubmed.ncbi.nlm.nih.gov/35247352/
Hall KS, Hyde ET, Bassett DR, et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int J Behav Nutr Phys Act. 2020;17(1):78. Published 2020 Jun 20. doi:10.1186/s12966-020-00978-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7305604/
Yuenyongchaiwat K. Effects of 10,000 steps a day on physical and mental health in overweight participants in a community setting: a preliminary study. Braz J Phys Ther. 2016;20(4):367-373. doi:10.1590/bjpt-rbf.2014.0160 https://pubmed.ncbi.nlm.nih.gov/27556393/
Ahmadi MN, Rezende LFM, Ferrari G, Del Pozo Cruz B, Lee IM, Stamatakis E. Do the associations of daily steps with mortality and incident cardiovascular disease differ by sedentary time levels? A device-based cohort study. Br J Sports Med. 2024;58(5):261-268. Published 2024 Mar 8. doi:10.1136/bjsports-2023-107221 https://pubmed.ncbi.nlm.nih.gov/38442950/
Castres I, Tourny C, Lemaitre F, Coquart J. Impact of a walking program of 10,000 steps per day and dietary counseling on health-related quality of life, energy expenditure and anthropometric parameters in obese subjects. J Endocrinol Invest. 2017;40(2):135-141. doi:10.1007/s40618-016-0530-9 https://pubmed.ncbi.nlm.nih.gov/27600387/
Morgan AL, Tobar DA, Snyder L. Walking toward a new me: the impact of prescribed walking 10,000 steps/day on physical and psychological well-being. J Phys Act Health. 2010;7(3):299-307. doi:10.1123/jpah.7.3.299 https://pubmed.ncbi.nlm.nih.gov/20551485/
Bishop PA, Jones E, Woods AK. Recovery from training: a brief review: brief review. J Strength Cond Res. 2008;22(3):1015-1024. doi:10.1519/JSC.0b013e31816eb518 https://pubmed.ncbi.nlm.nih.gov/18438210/
Spiering BA, Mujika I, Sharp MA, Foulis SA. Maintaining Physical Performance: The Minimal Dose of Exercise Needed to Preserve Endurance and Strength Over Time. J Strength Cond Res. 2021;35(5):1449-1458. doi:10.1519/JSC.0000000000003964 https://pubmed.ncbi.nlm.nih.gov/33629972/
Lloyd RS, Cronin JB, Faigenbaum AD, et al. National Strength and Conditioning Association Position Statement on Long-Term Athletic Development. J Strength Cond Res. 2016;30(6):1491-1509. doi:10.1519/JSC.0000000000001387 https://pubmed.ncbi.nlm.nih.gov/26933920/
Stone MH, Hornsby WG, Haff GG, et al. Periodization and Block Periodization in Sports: Emphasis on Strength-Power Training-A Provocative and Challenging Narrative [published correction appears in J Strength Cond Res. 2021 Nov 1;35(11):e290]. J Strength Cond Res. 2021;35(8):2351-2371. doi:10.1519/JSC.0000000000004050 https://pubmed.ncbi.nlm.nih.gov/34132223/
Kraemer WJ, Ratamess NA. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. 2004;36(4):674-688. doi:10.1249/01.mss.0000121945.36635.61 https://pubmed.ncbi.nlm.nih.gov/15064596/
Blanchard S, Glasgow P. A theoretical model to describe progressions and regressions for exercise rehabilitation. Phys Ther Sport. 2014;15(3):131-135. doi:10.1016/j.ptsp.2014.05.001 https://pubmed.ncbi.nlm.nih.gov/24913914/
Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;2009(3):CD002759. Published 2009 Jul 8. doi:10.1002/14651858.CD002759.pub2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4324332/
American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687-708. doi:10.1249/MSS.0b013e3181915670 https://pubmed.ncbi.nlm.nih.gov/19204579/
Bell LR, McNicol AJ, McNeil E, Van Nguyen H, Hunter JR, O’Brien BJ. The impact of progressive overload on the proportion and frequency of positive cardio-respiratory fitness responders. J Sci Med Sport. 2023;26(10):561-563. doi:10.1016/j.jsams.2023.08.175 https://pubmed.ncbi.nlm.nih.gov/37643931/
Taylor NF, Dodd KJ, Damiano DL. Progressive resistance exercise in physical therapy: a summary of systematic reviews. Phys Ther. 2005;85(11):1208-1223. https://pubmed.ncbi.nlm.nih.gov/16253049/
Hollings M, Mavros Y, Freeston J, Fiatarone Singh M. The effect of progressive resistance training on aerobic fitness and strength in adults with coronary heart disease: A systematic review and meta-analysis of randomised controlled trials. Eur J Prev Cardiol. 2017;24(12):1242-1259. doi:10.1177/2047487317713329 https://pubmed.ncbi.nlm.nih.gov/28578612/
Fujimoto N, Prasad A, Hastings JL, et al. Cardiovascular effects of 1 year of progressive endurance exercise training in patients with heart failure with preserved ejection fraction. Am Heart J. 2012;164(6):869-877. doi:10.1016/j.ahj.2012.06.028 https://pubmed.ncbi.nlm.nih.gov/23194487/
Plotkin D, Coleman M, Van Every D, et al. Progressive overload without progressing load? The effects of load or repetition progression on muscular adaptations. PeerJ. 2022;10:e14142. Published 2022 Sep 30. doi:10.7717/peerj.14142 https://pubmed.ncbi.nlm.nih.gov/36199287/
McNicol AJ, O’Brien BJ, Paton CD, Knez WL. The effects of increased absolute training intensity on adaptations to endurance exercise training. J Sci Med Sport. 2009;12(4):485-489. doi:10.1016/j.jsams.2008.03.001 https://pubmed.ncbi.nlm.nih.gov/18762454/
Lorenz D, Morrison S. CURRENT CONCEPTS IN PERIODIZATION OF STRENGTH AND CONDITIONING FOR THE SPORTS PHYSICAL THERAPIST. Int J Sports Phys Ther. 2015;10(6):734-747. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4637911/
Mann JB, Thyfault JP, Ivey PA, Sayers SP. The effect of autoregulatory progressive resistance exercise vs. linear periodization on strength improvement in college athletes. J Strength Cond Res. 2010;24(7):1718-1723. doi:10.1519/JSC.0b013e3181def4a6 https://pubmed.ncbi.nlm.nih.gov/20543732/
Greig L, Stephens Hemingway BH, Aspe RR, Cooper K, Comfort P, Swinton PA. Autoregulation in Resistance Training: Addressing the Inconsistencies. Sports Med. 2020;50(11):1873-1887. doi:10.1007/s40279-020-01330-8 https://pubmed.ncbi.nlm.nih.gov/32813181/
Hartmann H, Wirth K, Keiner M, Mickel C, Sander A, Szilvas E. Short-term Periodization Models: Effects on Strength and Speed-strength Performance. Sports Med. 2015;45(10):1373-1386. doi:10.1007/s40279-015-0355-2 https://pubmed.ncbi.nlm.nih.gov/26133514/
Kildow AR, Wright G, Reh RM, Jaime S, Doberstein S. Can Monitoring Training Load Deter Performance Drop-off During Off-season Training in Division III American Football Players?. J Strength Cond Res. 2019;33(7):1745-1754. doi:10.1519/JSC.0000000000003149 https://pubmed.ncbi.nlm.nih.gov/31145385/
González-Ravé JM, González-Mohino F, Rodrigo-Carranza V, Pyne DB. Reverse Periodization for Improving Sports Performance: A Systematic Review. Sports Med Open. 2022;8(1):56. Published 2022 Apr 21. doi:10.1186/s40798-022-00445-8 https://pubmed.ncbi.nlm.nih.gov/35445953/
Moesgaard L, Beck MM, Christiansen L, Aagaard P, Lundbye-Jensen J. Effects of Periodization on Strength and Muscle Hypertrophy in Volume-Equated Resistance Training Programs: A Systematic Review and Meta-analysis. Sports Med. 2022;52(7):1647-1666. doi:10.1007/s40279-021-01636-1 https://pubmed.ncbi.nlm.nih.gov/35044672/
Williams TD, Tolusso DV, Fedewa MV, Esco MR. Comparison of Periodized and Non-Periodized Resistance Training on Maximal Strength: A Meta-Analysis. Sports Med. 2017;47(10):2083-2100. doi:10.1007/s40279-017-0734-y https://pubmed.ncbi.nlm.nih.gov/28497285/
Miranda F, Simão R, Rhea M, et al. Effects of linear vs. daily undulatory periodized resistance training on maximal and submaximal strength gains. J Strength Cond Res. 2011;25(7):1824-1830. doi:10.1519/JSC.0b013e3181e7ff75 https://pubmed.ncbi.nlm.nih.gov/21499134/
Monteiro AG, Aoki MS, Evangelista AL, et al. Nonlinear periodization maximizes strength gains in split resistance training routines. J Strength Cond Res. 2009;23(4):1321-1326. doi:10.1519/JSC.0b013e3181a00f96 https://pubmed.ncbi.nlm.nih.gov/19528843/
Harries SK, Lubans DR, Callister R. Systematic review and meta-analysis of linear and undulating periodized resistance training programs on muscular strength. J Strength Cond Res. 2015;29(4):1113-1125. doi:10.1519/JSC.0000000000000712 https://pubmed.ncbi.nlm.nih.gov/25268290/
De Souza EO, Tricoli V, Rauch J, et al. Different Patterns in Muscular Strength and Hypertrophy Adaptations in Untrained Individuals Undergoing Nonperiodized and Periodized Strength Regimens. J Strength Cond Res. 2018;32(5):1238-1244. doi:10.1519/JSC.0000000000002482 https://pubmed.ncbi.nlm.nih.gov/29683914/
Bartolomei S, Zaniboni F, Verzieri N, Hoffman JR. New Perspectives in Resistance Training Periodization: Mixed Session vs. Block Periodized Programs in Trained Men. J Strength Cond Res. 2023;37(3):537-545. doi:10.1519/JSC.0000000000004465 https://pubmed.ncbi.nlm.nih.gov/36727999/
Bartolomei S, Hoffman JR, Merni F, Stout JR. A comparison of traditional and block periodized strength training programs in trained athletes. J Strength Cond Res. 2014;28(4):990-997. doi:10.1519/JSC.0000000000000366 https://pubmed.ncbi.nlm.nih.gov/24476775/
Evans JW. Periodized Resistance Training for Enhancing Skeletal Muscle Hypertrophy and Strength: A Mini-Review. Front Physiol. 2019;10:13. Published 2019 Jan 23. doi:10.3389/fphys.2019.00013 https://pubmed.ncbi.nlm.nih.gov/30728780/
Fleck SJ. Non-linear periodization for general fitness & athletes. J Hum Kinet. 2011;29A:41-45. doi:10.2478/v10078-011-0057-2 https://pubmed.ncbi.nlm.nih.gov/23486658/
Kiely J. Periodization paradigms in the 21st century: evidence-led or tradition-driven?. Int J Sports Physiol Perform. 2012;7(3):242-250. doi:10.1123/ijspp.7.3.242 https://pubmed.ncbi.nlm.nih.gov/22356774/
Kiely J. Periodization Theory: Confronting an Inconvenient Truth. Sports Med. 2018;48(4):753-764. doi:10.1007/s40279-017-0823-y https://pubmed.ncbi.nlm.nih.gov/29189930/
Mujika I, Halson S, Burke LM, Balagué G, Farrow D. An Integrated, Multifactorial Approach to Periodization for Optimal Performance in Individual and Team Sports. Int J Sports Physiol Perform. 2018;13(5):538-561. doi:10.1123/ijspp.2018-0093 https://pubmed.ncbi.nlm.nih.gov/29848161/
Issurin VB. New horizons for the methodology and physiology of training periodization. Sports Med. 2010;40(3):189-206. doi:10.2165/11319770-000000000-00000 https://pubmed.ncbi.nlm.nih.gov/20199119/
Issurin V. Block periodization versus traditional training theory: a review. J Sports Med Phys Fitness. 2008;48(1):65-75. https://pubmed.ncbi.nlm.nih.gov/18212712/
Issurin VB. Benefits and Limitations of Block Periodized Training Approaches to Athletes’ Preparation: A Review. Sports Med. 2016;46(3):329-338. doi:10.1007/s40279-015-0425-5 https://pubmed.ncbi.nlm.nih.gov/26573916/
Cunanan AJ, DeWeese BH, Wagle JP, et al. The General Adaptation Syndrome: A Foundation for the Concept of Periodization. Sports Med. 2018;48(4):787-797. doi:10.1007/s40279-017-0855-3 https://pubmed.ncbi.nlm.nih.gov/29307100/
Buckner SL, Mouser JG, Dankel SJ, Jessee MB, Mattocks KT, Loenneke JP. The General Adaptation Syndrome: Potential misapplications to resistance exercise. J Sci Med Sport. 2017;20(11):1015-1017. doi:10.1016/j.jsams.2017.02.012 https://pubmed.ncbi.nlm.nih.gov/28377133/
Fisher JP, Csapo R. Periodization and Programming in Sports. Sports (Basel). 2021;9(2):13. Published 2021 Jan 20. doi:10.3390/sports9020013 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7909405/
Larsen S, Kristiansen E, van den Tillaar R. Effects of subjective and objective autoregulation methods for intensity and volume on enhancing maximal strength during resistance-training interventions: a systematic review. PeerJ. 2021;9:e10663. Published 2021 Jan 12. doi:10.7717/peerj.10663 https://pubmed.ncbi.nlm.nih.gov/33520457/
Hickmott LM, Chilibeck PD, Shaw KA, Butcher SJ. The Effect of Load and Volume Autoregulation on Muscular Strength and Hypertrophy: A Systematic Review and Meta-Analysis. Sports Med Open. 2022;8(1):9. Published 2022 Jan 15. doi:10.1186/s40798-021-00404-9 https://pubmed.ncbi.nlm.nih.gov/35038063/
Vann CG, Haun CT, Osburn SC, et al. Molecular Differences in Skeletal Muscle After 1 Week of Active vs. Passive Recovery From High-Volume Resistance Training. J Strength Cond Res. 2021;35(8):2102-2113. doi:10.1519/JSC.0000000000004071 https://pubmed.ncbi.nlm.nih.gov/34138821/
Alves RC, Prestes J, Enes A, et al. Training Programs Designed for Muscle Hypertrophy in Bodybuilders: A Narrative Review. Sports (Basel). 2020;8(11):149. Published 2020 Nov 18. doi:10.3390/sports8110149 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7698840/
Bell L, Nolan D, Immonen V, et al. “You can’t shoot another bullet until you’ve reloaded the gun”: Coaches’ perceptions, practices and experiences of deloading in strength and physique sports. Front Sports Act Living. 2022;4:1073223. Published 2022 Dec 21. doi:10.3389/fspor.2022.1073223 https://pubmed.ncbi.nlm.nih.gov/36619355/
Coleman M, Burke R, Augustin F, et al. Gaining more from doing less? The effects of a one-week deload period during supervised resistance training on muscular adaptations. PeerJ. 2024;12:e16777. Published 2024 Jan 22. doi:10.7717/peerj.16777 https://pubmed.ncbi.nlm.nih.gov/38274324/
Bell L, Strafford BW, Coleman M, Androulakis Korakakis P, Nolan D. Integrating Deloading into Strength and Physique Sports Training Programmes: An International Delphi Consensus Approach. Sports Med Open. 2023;9(1):87. Published 2023 Sep 21. doi:10.1186/s40798-023-00633-0 https://pubmed.ncbi.nlm.nih.gov/37730925/
Rogerson D, Nolan D, Korakakis PA, Immonen V, Wolf M, Bell L. Deloading Practices in Strength and Physique Sports: A Cross-sectional Survey. Sports Med Open. 2024;10(1):26. Published 2024 Mar 18. doi:10.1186/s40798-024-00691-y https://pubmed.ncbi.nlm.nih.gov/38499934/

Paddy Farrell
Hey, I'm Paddy!
I am a coach who loves to help people master their health and fitness. I am a personal trainer, strength and conditioning coach, and I have a degree in Biochemistry and Biomolecular Science. I have been coaching people for over 10 years now.
When I grew up, you couldn't find great health and fitness information, and you still can't really. So my content aims to solve that!
I enjoy training in the gym, doing martial arts and hiking in the mountains (around Europe, mainly). I am also an avid reader of history, politics and science. When I am not in the mountains, exercising or reading, you will likely find me in a museum.